Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 12
Deterioration of quality of life is associated with the exacerbation frequency in individuals with alpha-1-antitrypsin deficiency – analysis from the German Registry
Authors Bernhard N, Lepper PM, Vogelmeier C, Seibert M, Wagenpfeil S , Bals R, Fähndrich S
Received 22 December 2016
Accepted for publication 22 March 2017
Published 12 May 2017 Volume 2017:12 Pages 1427—1437
DOI https://doi.org/10.2147/COPD.S130925
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 6
Editor who approved publication: Dr Richard Russell
Nikolas Bernhard,1 Philipp M Lepper,1 Claus Vogelmeier,2 Martina Seibert,1 Stefan Wagenpfeil,3 Robert Bals,1 Sebastian Fähndrich1
1Department of Internal Medicine V – Pulmonology, Allergology, Intensive Care Medicine, Saarland University Hospital, Homburg, 2Department of Medicine, Pulmonary and Critical Care Medicine, University Medical Center Giessen and Marburg, Philipps-University Marburg, Member of the German Center for Lung Research (DZL), 3Faculty of Medicine, Institute of Medical Biometry, Epidemiology and Medical Informatics, Saarland University, Campus Homburg, Germany
Background: Alpha-1-antitrypsin deficiency (AATD) is a rare hereditary disease that is associated with a higher risk to develop chronic obstructive pulmonary disease and liver cirrhosis. Previous cross-sectional studies on AATD individuals have shown a relationship between worse St George’s Respiratory Questionnaire (SGRQ) scores and elevated exacerbation rate or high cigarette consumption. There is a lack of longitudinal data on the relationship between the exacerbation rate and worsening of SGRQ during disease. The aim of this study was to provide not only cross-sectional data but also information about the deterioration in quality of life over a follow-up period up to 7 years (median follow-up period of 3.33 years).
Methods: We investigated questionnaire-based data of the German AATD registry concerning the relationship between SGRQ and exacerbation frequency, smoking history, forced expiratory volume in 1 second (FEV1) and carbon monoxide diffusion capacity (DLCO) first in cross-sectional analysis and later in longitudinal analysis.
Results: Eight hundred sixty-eight individuals with protease inhibitor ZZ (PiZZ) genotype with an average age of 52.6±12.8 years had an SGRQ score of 45.7±20.6. SGRQ significantly correlated with the exacerbation frequency within the last 2 years (r=0.464; P<0.001), smoking history (r=0.233; P<0.001), FEV1 (r=−0.436; P<0.001), DLCO (r=−0.333; P<0.001), and patients’ age (r=0.292; P<0.001). Individuals with occupational dust exposure had significantly worse quality of life (P<0.001). Mean annual deterioration of SGRQ in all patients with available follow-up data (n=286) was 1.21±4.45 points per year. Univariate and multivariate analysis showed a significant relationship between worsening of SGRQ/year and exacerbation frequency in the follow-up period (r=0.144; P=0.015).
Conclusion: Worsening of SGRQ is associated with the exacerbation frequency in individuals with PiZZ AATD.
Keywords: SGRQ, quality of life, AATD, alpha-1-antitrypsin deficiency, COPD, exacerbations, emphysema, FEV1
Background
Alpha-1-antitrypsin deficiency (AATD) is a genetic disorder that leads to low circulating levels of alpha-1-antitrypsin (AAT). Affected individuals are at higher risk of developing chronic obstructive pulmonary disease (COPD) and liver cirrhosis.1,2 The frequency of the AATD genotype protease inhibitor ZZ (PiZZ) in Western Europe is about 1:5,000–15,000.3 Patient registries are helpful to get more insights into this orphan disease.4 The German registry for individuals with AATD (AATDR) is a questionnaire-based collection of data that currently includes 1,074 individuals (12/2015).5 It was established in 2003 and is continuously recruiting further participants. The data are self-reported with reports on pulmonary function provided by the patient’s physician.
The assessment of quality of life has been established as a patient-related outcome, which correlates with airway obstruction and disease severity in COPD.6–8 St George’s Respiratory Questionnaire (SGRQ) was developed by Jones et al in the year 1991 to quantify health of patients with diseases causing chronic airflow limitation.6 The questionnaire comprises three parts: the symptoms-, the activity- and the impacts-component. Previous studies showed a significant relationship between SGRQ-scores and exacerbation frequency, daily wheezing, sputum and dyspnea, bronchitis symptoms, 12-minute walking test and forced expiratory volume in 1 second (FEV1) in patients with COPD.9,10 Total SGRQ correlated significantly with prognosis and mortality in these patients.7,8 Studies from other AATD registries have shown a relationship between worse SGRQ-scores and elevated exacerbation rate or high cigarette consumption.11–13 Most of these studies only provided cross-sectional data about the relationship between SGRQ and exacerbation rate11,12 except for two prior studies. Campos et al, investigated the longitudinal deterioration of SGRQ over a period of 12 months. In their study, they could not find significance between change in SGRQ and frequent exacerbations within 1 year.13 Needham and Stockley also did not find a significant correlation between deterioration of SGRQ and exacerbations; however, they describe a greater improvement in the SGRQ symptoms-score in individuals with no or infrequent exacerbations.14
Our aim was not only to analyze cross-sectional data but also to investigate the influence of the exacerbation rate, the deterioration of FEV1 (ΔFEV1/year) and carbon monoxide diffusion capacity (ΔDLCO/year) on the change of health-related quality of life (ΔSGRQ/year) during a longer follow-up period (up to 7 years/median follow-up period of 3.33 years). The research question was whether the longitudinal deterioration of health-related quality of life is dependent on the exacerbation rate in individuals with PiZZ AATD.
To answer this question, our paper is divided into a cross-sectional (n=868) and a longitudinal follow-up analysis (n=286).
Materials and methods
Structure of the German registry for individuals with AATD
The AATDR was founded in 2003 and comprises a registry for adult patients and for individuals below 18 years of age.5 The children’s registry was excluded from the present analysis. The registry study is continuously enrolling individuals with AATD.
The inclusion criterion for the registry is severe AAT deficiency, reflected by low serum concentrations of AAT with PiZZ, protease inhibitor SZ (PiSZ) genotype or other deficient allelic variants. The questionnaires and the data storage concept were approved by the ethics committees of the Marburg University and the Landesärztekammer Saarland (SN80/10) and the Data Safety Office of the State of Hessen (all in Germany). A declaration of informed consent was signed by all individuals.
Structure of questionnaire
The AATDR is based on a ten-page questionnaire that is sent to participants and their physicians. Exacerbations are defined as an excessive worsening of COPD symptoms with a duration of more than 2 days that required hospitalization or treatment with antibiotics or systemic corticosteroids. The questionnaire contains questions on pulmonary diseases, for example, chronic bronchitis, emphysema or pneumonia. Data on smoking history are recorded and used to calculate the cumulative nicotine consumption in pack-years. Several items of the questionnaire had to be completed by the patients’ physician, for example, questions on treatment, pulmonary function, such as FEV1, forced vital capacity (FVC) and VC and the carbon monoxide diffusion capacity (DLCO). The SGRQ was applied to measure the health-related quality of life.6 The SGRQ consists of 50 items and three sub-scales (symptoms-, activity- and impacts-score). The scores range from 0 to 100, with higher results symbolizing worse quality of life. Questionnaires were sent to the registered patients for follow-up assessments after 2 and 7 years. The collected data were archived in an MS Access 2010 – database.
Data analysis
Data collected between 06/2004 and 12/2015 were used for the present analysis and transferred into SPSS (IBM, version 23). Patients with lung transplantation or lung volume reduction in the follow-up period were excluded from the longitudinal analysis. We analyzed data on at least one follow-up survey for 286 individuals over a period of ~2 years. Furthermore, data were available for a second follow-up survey after ~7 years for 90 individuals. In individuals with more than one follow-up survey, we averaged the available values. The follow-up period differed in some cases by several months.
Data sets are not totally complete because questionnaires were not always perfectly answered. Figure 1 shows the study enrollment process and the numbers of valid data for the investigated variables. For the longitudinal analysis, changes over time in FEV1, DLCO and SGRQ were standardized by calculating the change in mL, mmol/min/kPa and score per 12 months.
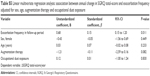
Statistical analysis
Continuous variables were expressed as means ± standard deviation. The mean values of continuous variables in different groups were compared by independent samples t-test or Kruskal–Wallis test/one-way analysis of variance. The correlations between continuous variables were verified by multivariate linear regression models as sensitivity analysis. Due to multicollinearity between most of the variables in the multivariate regression analysis, we could not include all variables in a common model. Therefore, univariate results were analyzed by different models, including only a number of potential confounders (Tables S1–S5). In addition to the two-tailed significance, we specified the estimated effect of respective regression coefficients (β) and the 95% confidence interval. Categorical data are shown by frequencies and percentages. Statistical significance was considered for two-sided P-values <0.05. Our analysis was performed by IBM SPSS version 23.
Ethics approval and consent to participate
The research on the registry data including the questionnaires and the data storage concept and the publication of the data were approved by the ethical committees of the Marburg University and the Landesärztekammer Saarland (SN80/10) and the Data Safety Office of the State of Hessen (all in Germany). A declaration of informed consent was signed by all participating individuals.
Results
Characteristics of patients
In December 2015, 1,074 AATD individuals with PiZZ, PiSZ and other deficient alleles were registered in the AATDR. We analyzed the data of 868 PiZZ AATD subjects (male n=490; female n=378). About three quarters of analyzed individuals had a history of smoking; however, most of them had quit smoking before being registered. The most common reason for diagnosis was pulmonary disorder followed by family screening. Most patients reported that they suffered from pulmonary disease, most frequently from emphysema and chronic bronchitis. Detailed baseline characteristics are summarized in Table 1.
Increased age correlates with worse quality of life (cross-sectional analysis)
We found a significant relationship between age and SGRQ total-score (r=0.29; P<0.001) (and respectively to each SGRQ sub-score, all P<0.001; Table 2). We further confirmed a significant relationship in multivariate regression analysis, adjusted for sex, nicotine consumption, exposure of occupational dust and augmentation therapy (P<0.001; Table S1).
Positive association between inhaled exposure (nicotine consumption and occupational dust exposure) and SGRQ (cross-sectional analysis)
Correlation analysis between SGRQ score and smoking history (pack-years) showed significant positive association in all sub-scores of SGRQ in a cross-sectional approach (P<0.001; Table 2; n=840). The adjusted values in multivariate analysis (Table S1; for sex, age, exposure of occupational dust and augmentation therapy) showed in some parts even higher regression coefficients in total-, symptoms-, activity- and impacts-score (β=0.24; β=0.20; β=0.30; β=0.17; all P<0.001). Patients who reported an occupational dust exposure (n=335) had significantly higher SGRQ scores as compared to patients without exposure (all P<0.001; Table 3).
Worse SGRQ is associated with the exacerbation frequency (cross-sectional analysis)
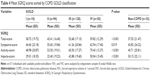
The SGRQ total-score just as the sub-scales (symptoms-, activity- and impacts-score showed a correlation with the exacerbation rate within the last 2 years (all P<0.001; Figure 2; Table 2; n=833). Multivariate regression analysis (including sex, augmentation therapy and occupational dust exposure) confirmed the significant associations (total-score [β=0.41; P<0.001]; symptoms-score [β=0.41; P<0.001]; activity-score [β=0.34; P<0.001]; impacts-score [β=0.40; P<0.001]) (Table S2). SGRQ total-score correlated with the use of systemic corticosteroids (r=0.480; P<0.001), the increase of current medication (r=0.469; P<0.001), the need of antibiotics (r=0.466; P<0.001) and the hospitalization rate (r=0.455; P<0.001). Multivariate regression evaluation (adjusted for sex, augmentation therapy and occupational dust exposure) confirmed significance for the use of systemic corticosteroids, the increase of current medication, the need of antibiotics and the hospitalization rate (β=0.40; β=0.40; β=0.40; β=0.38; all P<0.001).
  | Figure 2 Worse SGRQ total-score is associated with frequent exacerbations within the last 2 years in univariate analysis. |
FEV1 and diffusion capacity (DLCO) correlate significantly with SGRQ (cross-sectional analysis)
Low baseline bronchodilator FEV1 % of predicted (% pred.) (available in n=400 individuals) is associated with worse quality of life total-, symptoms-, activity- and impacts-scores (all P<0.001) (Table 2; Figure 3). The correlation with SGRQ activity-score was stronger as compared to SGRQ total-score. Here, multivariate linear regression confirmed significance between low FEV1 and SGRQ total-score (including sex, augmentation therapy and occupational dust exposure) (β=−0.41; P<0.001) (Table S3). The relationship between baseline diffusion capacity (DLCO % pred.) (available in n=485 individuals) and health-related quality of life (including sub-scales symptoms-, activity- and impacts-scores) was significant in multivariate analysis adjusted for sex, augmentation therapy and occupational dust exposure (β=−0.30; P<0.001) (Table S4). Individuals with available postbronchodilator FEV1 and FVC (n=317) were classified into COPD severity levels: Global Initiative for Chronic Obstructive Lung Disease (GOLD) I (3.1%), GOLD II (29.6%), GOLD III (40.4%), GOLD IV (15.8%) and non-COPD (11.0%). The mean values of SGRQ scores were stratified according to the FEV1-based GOLD classification (Figure 4; Table 4). The SGRQ total-score differed significantly between GOLD I–IV (P<0.001). In summary, patients with lower DLCO and FEV1 or more severe spirometric GOLD stage showed higher SGRQ scores.
Individuals on augmentation therapy have worse SGRQ (cross-sectional analysis)
Individuals who reported an AAT augmentation therapy had significantly worse SGRQ total-, symptoms-, activity- and impacts-scores at baseline (all P<0.001) compared with subjects without this therapy (Table 5). Significant lower FEV1 and DLCO values could be demonstrated for subjects receiving augmentation therapy (all P<0.001).
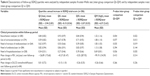
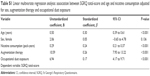
Deterioration of SGRQ in follow-up period correlates with exacerbation rate (longitudinal analysis)
In a next step, we analyzed the longitudinal data from follow-up surveys to identify the factors that are associated with changes of SGRQ score. The mean annual deterioration of quality of life in all patients with available follow-up data (n=286) was expressed by an increase of SGRQ score (1.21±4.45 points/year). In univariate analysis, we found significant relationship between the change of SGRQ score per year and the annual frequency of exacerbations in the follow-up period (r=0.144; P=0.015) (n=285). We confirmed this significant relationship in multivariate analysis adjusted for sex, age, augmentation therapy and occupational dust exposure (β=0.15; P=0.011) (Table S5).
Two hundred eighty-six individuals were divided into quartiles. Individuals in quartile I had low SGRQ rise or even loss of SGRQ score, patients in quartile IV had strong SGRQ rise within the follow-up period. Significant differences could be shown between quartiles of SGRQ total-score. Patients in the lowest quartile demonstrated lower exacerbation rate within the follow-up period than individuals in the top quartile (P=0.022). Significances between quartiles I and IV were also found for the need of corticosteroids (P=0.013), the increase of current medication (P=0.019) and the frequency of hospitalization (P=0.035). In inter-group comparison of all quartiles (I–IV), patients with higher deterioration in SGRQ score reported more often an increase of medication (P=0.035) and more frequent hospitalizations (P=0.036), while the need for corticosteroids (P=0.077) and antibiotics (P=0.394) only showed a trend. No significant correlations were found between the mean loss of FEV1 (mL/year) or DLCO (mmol/min/kPa/year) and the mean increase of SGRQ scores per year (n=82 individuals with available postbronchodilator FEV1 follow-up data; n=84 individuals with available DLCO follow-up data).
These data are summarized in Table 6. Taken together, worsening of quality of life is associated with frequent exacerbations in the follow-up period.
Discussion
The main finding of this study was a significant relationship between the longitudinal deterioration of health-related quality of life and the annual frequency of self-reported exacerbations in individuals with severe AATD. Moreover, the cross-sectional analysis revealed significant correlations between baseline SGRQ and smoking history, the rate of moderate and severe exacerbations, postbronchodilator FEV1 and DLCO. Most of the correlations in cross-sectional and longitudinal results were weak but significant. The study not only considered symptomatic AATD individuals but also included asymptomatic individuals with PiZZ who were diagnosed by family screening or incidental finding.
We provided longitudinal data of up to 7 years (median follow-up period of 3.33 years) and our results suggest that worsening of SGRQ is significantly associated with an elevated exacerbation rate. Previous longitudinal studies could not find a significant relationship between the deterioration of SGRQ total-score and the exacerbation frequency.13,14
Patient-reported outcomes, such as the assessment of health-related quality of life are increasingly recognized as important instruments in the evaluation of COPD patients.15 It has been shown that they predict prognosis and can be used to evaluate clinical severity.6–8 In COPD, numerous studies showed correlations between SGRQ-scores and exacerbation frequency, daily wheezing, sputum and dyspnea, bronchitis symptoms, BODE index, 12-minute walking test and FEV1.9,10,16
The results confirm other cross-sectional studies on AATD individuals that demonstrated the impact of exacerbations, lower FEV1 and DLCO and smoking history on the SGRQ.11,12,17
Detailed analysis showed that SGRQ sub-scores are differentially altered. The exacerbation rate had strong influence on SGRQ impacts-score, which is related to the disease’s impact on employment and daily life.6 In contrast, nicotine consumption was most strongly associated with SGRQ activity-score. Current or former smokers may be more affected by breathlessness and restriction in physical activities.
High levels of occupational dust exposure are associated with an increased risk of more severe GOLD–COPD stages.18 Our results showed significantly worse SGRQ in individuals with occupational dust exposure compared with unexposed individuals, underlining the importance of work-related exposure.
In accordance with studies on the Canadian AATD registry12 patients receiving augmentation therapy had worse quality of life, FEV1 % pred. and DLCO % pred. Augmentation therapy seems to be associated with an increased disease severity and more impaired lung function.
In the longitudinal analysis of this study, we evaluated the data of 286 individuals. However, there was a loss of 582 individuals for the follow-up assessments. Nevertheless, these individuals did not show significantly worse FEV1, DLCO and SGRQ at baseline compared with subjects with available follow-up data. This study shows a mean annual deterioration of SGRQ score of ~1.2 units in the whole population. In non-AATD COPD, two studies reported a deterioration of ~0.06 units per year or even an improvement.8,19 The patients in these two studies were older than in this analysis. Previous investigations on AATD individuals reported an annual worsening of SGRQ of ~1.05 points.20 A change in SGRQ score of 4 units is regarded as clinically significant.21 Therefore, we divided the individuals into quartiles of ΔSGRQ total-score/year in our longitudinal analysis. The quartile with the highest worsening of SGRQ (QIV) showed a clear significant mean deterioration of 6.57 units/year. Individuals with the highest deterioration of SGRQ (QIV) showed a significantly higher rate of exacerbations compared with individuals with lower deterioration or even improvement of SGRQ (QI). This concurs with the results of the study by Needham and Stockley.14 Furthermore, in our study, the number of exacerbations in the follow-up period correlates significantly with a stronger annual impairment of quality of life. In contrast to Needham and Stockley, we found significance for the correlation in the univariate analysis and in the multivariate regression model.
Next, we analyzed the relationship between ΔSGRQ total-score/year and the decline of FEV1 and DLCO in our longitudinal analysis. The correlation analysis as well as the comparison between high and low worsening quartiles of SGRQ (QIV vs QI) showed no significance.
We conclude that the change in health-related quality of life is more dependent on the exacerbation frequency than on the decline of FEV1 and DLCO.
This study has some limitations: the findings might not be representative for all individuals with AATD because individuals with more severe manifestations or increased burden of symptoms might be overrepresented. As the data depend largely on self-reported information (eg, exacerbations and lung function data), the quality of these data is likely less as compared to well-controlled clinical trials. Nevertheless, our results are premised on a large study group and a long period of observation (up to 7 years).
Conclusion
The annual worsening of health-related quality of life, assessed by the SGRQ, is significantly associated with the frequency of exacerbations in individuals with PiZZ AATD (symptomatic and asymptomatic subjects) in cross-sectional and longitudinal analysis.
Acknowledgments
The AATDR was supported by grants from the EU PAAIR, the Bundesministerium für Bildung und Forschung COSYCONET/ASCONET (BMBF 01GI1001) to RB and CV, and supported by a grant from Bayer/Talecris/Grifols from 2003 until 2012. The study was supported by a donation of the Bumm family to the Saarland University.
Availability of data and materials: The data sets of the AATDR are located at the Department of Internal Medicine V – Pulmonology, Allergology, Intensive Care Medicine, Saarland University Hospital, Homburg, Germany and are available from the corresponding author on reasonable request.
Author contributions
NB, PML, CV, RB, and SF contributed to conception of the study, patient recruitment and original data collection and interpretation. MS contributed to the patient recruitment. SW supported the statistical analysis. The authors alone are responsible for the content and the writing of the paper. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
RB, SF and CV have obtained research support and travel sponsoring from Talecris/Grifols and CSL Behring. CV has received honoraria for speaking engagements and for chairing a research prize committee from Talecris/Grifols. PML has received speaker fees from Talecris/Grifols. The authors report no other conflicts of interest in this work.
References
Laurell CB, Eriksson S. The electrophoretic alpha1-globulin pattern of serum in alpha1-antitrypsin deficiency. Scan J Clin Lab Invest. 1963;15:132–140. | ||
Fregonese L, Stolk J. Hereditary alpha-1-antitrypsin deficiency and its clinical consequences. Orphanet J Rare Dis. 2008;3:16. | ||
Blanco I, de Serres FJ, Fernandez-Bustillo E, Lara B, Miravitlles M. Estimated numbers and prevalence of PI*S and PI*Z alleles of alpha1-antitrypsin deficiency in European countries. Eur Respir J. 2006;27(1):77–84. | ||
Luisetti M, Campo I, Scabini R, et al. The problems of clinical trials and registries in rare diseases. Respir Med. 2010;104(Suppl 1):42–44. | ||
Fähndrich S, Herr C, Greulich T, et al. Sex differences in alpha-1-antitrypsin deficiency lung disease-analysis from the German registry. COPD. 2015;12(Suppl 1):58–62. | ||
Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A self-complete measure of health status for chronic airflow limitation. The St. George’s Respiratory Questionnaire. Am Rev Respir Dis. 1992;145(6):1321–1327. | ||
Domingo-Salvany A, Lamarca R, Ferrer M, et al. Health-related quality of life and mortality in male patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2002;166(5):680–685. | ||
Wilke S, Jones PW, Mullerova H, et al. One-year change in health status and subsequent outcomes in COPD. Thorax. 2015;70(5):420–425. | ||
Seemungal TA, Donaldson GC, Paul EA, Bestall JC, Jeffries DJ, Wedzicha JA. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157(5 Pt 1):1418–1422. | ||
Ketelaars CA, Schlosser MA, Mostert R, et al. Determinants of health-related quality of life in patients with chronic obstructive pulmonary disease. Thorax. 1996;51(1):39–43. | ||
Gauvain C, Mornex JF, Pison C, et al. Health-related quality of life in patients with alpha-1 antitrypsin deficiency: the French experience. COPD. 2015;12(Suppl 1):46–51. | ||
Bradi AC, Audisho N, Casey DK, Chapman KR. Alpha-1 antitrypsin deficiency in Canada: regional disparities in diagnosis and management. COPD. 2015;12(Suppl 1):15–21. | ||
Campos MA, Alazemi S, Zhang G, et al. Exacerbations in subjects with alpha-1 antitrypsin deficiency receiving augmentation therapy. Respir Med. 2009;103(10):1532–1539. | ||
Needham M, Stockley RA. Exacerbations in {alpha}1-antitrypsin deficiency. Eur Respir J. 2005;25(6):992–1000. | ||
Cazzola M, Hanania NA, MacNee W, Rüdell K, Hackford C, Tamimi N. A review of the most common patient-reported outcomes in COPD – revisiting current knowledge and estimating future challenges. Int J Chronic Obstr. 2015;10:725–738. | ||
Marin JM, Cote CG, Diaz O, et al. Prognostic assessment in COPD: health related quality of life and the BODE index. Respir Med. 2011;105(6):916–921. | ||
Manca S, Rodriguez E, Huerta A, et al. Usefulness of the CAT, LCOPD, EQ-5D and COPDSS scales in understanding the impact of lung disease in patients with alpha-1 antitrypsin deficiency. COPD. 2014;11(5):480–488. | ||
Mehta AJ, Miedinger D, Keidel D, et al. Occupational exposure to dusts, gases, and fumes and incidence of chronic obstructive pulmonary disease in the Swiss Cohort Study on Air Pollution and Lung and Heart Diseases in Adults. Am J Respir Crit Care Med. 2012;185(12):1292–1300. | ||
Nagai K, Makita H, Suzuki M, et al. Differential changes in quality of life components over 5 years in chronic obstructive pulmonary disease patients. Int J Chron Obstruct Pulmon Dis. 2015;10:745–757. | ||
Dowson LJ, Guest PJ, Stockley RA. Longitudinal changes in physiological, radiological, and health status measurements in alpha(1)-antitrypsin deficiency and factors associated with decline. Am J Respir Crit Care Med. 2001;164(10 Pt 1):1805–1809. | ||
Jones PW. Interpreting thresholds for a clinically significant change in health status in asthma and COPD. Eur Respir J. 2002;19(3):398–404. |
Supplementary materials
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.