Back to Journals » OncoTargets and Therapy » Volume 12
Detection Of Mutations In The Isocitrate Dehydrogenase Genes (IDH1/IDH2) Using castPCRTM In Patients With AML And Their Clinical Impact In Mexico City
Authors Olarte I , García A , Ramos C, Arratia B, Centeno F , Paredes J, Rozen E, Kassack J , Collazo J, Martínez A
Received 17 June 2019
Accepted for publication 1 September 2019
Published 1 October 2019 Volume 2019:12 Pages 8023—8031
DOI https://doi.org/10.2147/OTT.S219703
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Nicola Silvestris
Irma Olarte,1 Anel García,1 Christian Ramos,2 Brenda Arratia,1 Federico Centeno,3 Johanna Paredes,1 Etta Rozen,2 Juan Kassack,2 Juan Collazo,2 Adolfo Martínez1
1Department of Molecular Biology, Hematology Service, Hospital General de México, “Dr. Eduardo Liceaga”, Mexico City, Mexico; 2Department of Medical Hematology, Hospital General de México, “Dr. Eduardo Liceaga”, Mexico City, Mexico; 3Department Immunogenomics and Metabolic Disease, Instituto Nacional de Medicina Genómic, SS, Mexico City, Mexico
Correspondence: Adolfo Martínez
Laboratorio de Biología Molecular del Servicio de Hematología. Hospital General de México “Dr. Eduardo Liceaga”, Ciudad de México 06726, México
Email [email protected]
Objective: Approximately 40–50% of patients with acute myeloid leukaemia (AML) have been reported to present with a normal karyotype and a variable disease-free period, most likely due to the molecular heterogeneity presented by these patients. A variety of mutations have been identified at the molecular level, such as those in the IDH1/2 gene, which causes a gain of function of the isocitrate dehydrogenase enzyme, generating high levels of the (R)-2-hydroxyglutarate oncometabolite, which competitively inhibits dioxygenase enzymes. Therefore, the objective of this study was to evaluate the incidence of IDH1/2 gene mutations in AML patients and their impact on survival.
Materials and methods: A total of 101 patients with a diagnosis of AML were included; mononuclear cells were obtained for DNA extraction and purification. Mutations were detected using TaqMan™ competitive allele-specific probes (castPCR™). Overall survival curves were plotted using IBM SPSS Statistics 23 software.
Results: The frequency of IDH gene mutations was 19.8%. For the IDH1 gene, 13.8% of the mutations identified included R132H, V178I, G105G and R132C. The frequency of mutations of the IDH2 gene was 5.9%; the variants included R172K and R140Q. The mean survival time in patients without IDH1 gene mutations was 173.15 days (120.20–226.10), while the mean survival time for patients with mutations was 54.95 days (9.7–100.18), p = 0.001.
Conclusion: The frequency of IDH1 and IDH2 gene mutations in the sample was similar to that reported in other studies. The analysis of these mutations in AML patients is of great importance as a prognostic factor due to their impact on survival and their use as potential therapeutic targets or as targets of inhibitors of IDH1(Ivosidenib, Tibsovo) and IDH2 (Enasidenib, Idhifa).
Keywords: isocitrate dehydrogenase, competitive allele specific TaqMan, acute myeloid leukemia
Introduction
Acute myeloid leukaemia (AML) is one of the main haematological oncological neoplasias treated in reference centres; it is the most common type of acute leukaemia in adults, and its incidence increases with age.1–3 The incidence in Mexico is six cases per 100,000 inhabitants, with a mortality rate of 5.9/100,000 inhabitants. It has been reported that approximately 50% of AML patients present with normal karyotypes; however, at the molecular level, a variety of mutations have been identified, in which genes that regulate cell proliferation, differentiation and apoptosis are altered.4,5 These alterations impact the prognosis and survival of patients.6,7 It is important to highlight that the treatment of AML has consisted of a 7+3 protocol since 1973.8,9 However, the timely detection of gene alterations that cause AML will allow access to new drugs and therapeutic targets as inhibitors of the disease. The goal of kinase epigenetic modulators is to achieve greater overall survival.10,11 One type of mutation that is of great interest in AML is mutation of the IDH (isocitrate dehydrogenase) genes, which is present in > 80% of low-grade gliomas and secondary glioblastomas and in 20% of leukaemias.12–14 Three isoforms of the IDH enzyme have been identified: IDH1 is located in the cytoplasm, while IDH2 and IDH3 are located in the mitochondria.15,16 These genes have a high frequency of mutation in patients with AML and other tumour types.17–19 IDH mutations mainly affect the residues of the active site (e.g., IDH1 R132, IDH2 R140 or IDH2 R172), resulting in a gain of function with increased activity of the neomorphic enzyme and therefore accumulation of D-2-hydroxyglutarate (2-HG).20–22 The oncometabolite 2-HG can competitively inhibit multiple α-KG-dependent dioxygenases, including key epigenetic regulators such as histone demethylases and TET proteins.23,24 Consequently, IDH mutations are associated with chromatin alterations, including global histone alterations and DNA methylation.25,26
 |
Figure 1 Evaluation of castPCRTM Limit of Detection (LOD). The LODs of castPCRTM are shown in Figure 1A and B. We found that the mutated alleles were detectable by castPCRTM up to a dilution of 1:50 for both cases: R132H_rf; CT = (25.04–31.14), R132H_mu; CT = (24.32–30.10). |
It is important to identify the presence of IDH1/2 mutations in a rapid manner so that patients can benefit from targeted therapies. Therefore, it is necessary to seek reliable methodological alternatives, such as castPCRTM, which is characterised by its high sensitivity and specificity, because it can detect minimal amounts of mutated DNA in a sample that contains large amounts of normal wild-type DNA.27,28 The castPCRTM technique uses specific oligonucleotides for the mutated allele that compete with an MGB-blocking oligonucleotide to suppress the normal allele.29,30 It can robustly detect mutant alleles at values as low as 0.1% in a wild-type background and has a> 99% concordance with other technologies, including technology based on digital PCR and Sanger sequencing.31
It is important to highlight that although Sanger sequencing is the “gold standard” for the identification of mutations due to its low rate of false positives and high specificity, it has a number of disadvantages, including low sensitivity, the time required to perform the assay, requirement of high-quality tissue samples and the need for manual interpretation.32
Unlike other methods, such as the amplification refractory mutation system (ARMS), for which the sensitivity is 1%, and Sanger sequencing, with 10–25% sensitivity castPCRTM has a sensitivity of 0.1%.33 Moreover, next-generation sequencing (NGS) technology, which is used for the detection of multiple mutations, has the disadvantages of being time consuming and too costly to detect a specific genetic allele. In addition, the data produced by NGS are not suitable for routine clinical analysis.34
Based on the above information, we evaluated the incidence of gene mutations (IDH1/2) by castPCRTM in AML patients and the clinical impact of these mutations on diagnosis, prognosis and survival.
Materials And Methods
Description Of The Study Population
A total of 101 patients with de novo AML treated at the General Hospital of Mexico with complete clinical records were included. Among the patients, 50.5% were female (n = 51), and the remaining patients were male (n = 50, 49.5%). The mean age was 46 years (15–92 years). The majority of patients were younger than 60 years (n = 68, 66.6%). The diagnosis of AML was based on both morphological findings and flow cytometry; the majority of patients had leukaemia with monocytoid characteristics (AML-M4, 60.4%), followed by those with differentiation (AML-M2, 30.7%). The mean haemoglobin level was 11 g/dl (4–91), with a mean leukocyte count of 150 x 109/L (0.2-4870×109/L) and a mean platelet count of 48 × 109/L (3-241x109/L). Regarding the main genetic alterations identified, 45.5% of patients had a normal karyotype, and only one patient with hyperdiploidy was detected. The other clinical and laboratory parameters are described in Table 1.
 |
Table 1 Clinical Characteristics Of The Population Analyzed (n=101) |
Approval for the present study was provided by the Ethics Committee of the Hospital General de Mexico “Dr. Eduardo Liceaga”. The informed written consents were collected from all enrolled patients and the entire study was performed based on the Declaration of Helsinki.
Type Of Treatment
The main part of the treatment was based on the 7 + 3 protocol; the intensity of the treatment was mainly based on the age and functional status of the patients. The normal intensity 7 + 3 protocol (100 mg/m2cytarabine for 7 days plus 60 mg/m2daunorubicin for 3 days) was initiated in 78 patients (n = 77.2%), a total of 13 patients received a reduced dose of 7 + 3 (12.9%), and seven patients received cytarabine subcutaneously (6.9%).
Response To Treatment
After the initiation of induction therapy, the response to treatment was assessed according to the recovery of the blood count and the decrease in the number of blasts in bone marrow. Accordingly, patients were classified into different types of responses. A total of 36 patients (35.6%) met the criteria for complete remission, while 12 patients (11.9%) were considered to have a partial response.
Regarding refractory leukaemia, 21.8% (n =22) of patients showed resistance to the first treatment protocol, while 30.7% (n =31) died during the remission induction phase (26 cases of death due to aplasia and five cases of indeterminate death).
Separation Of Mononuclear Cells By A Ficoll-Hypaque Gradient
Peripheral blood samples were obtained from normal donors and AML patients. Mononuclear cells were separated usinga Ficoll-Hypaque gradient (Lymphoprep, Nycomed Pharma AS, density 1.077 g/L), and isolated mononuclear cells were stored at −70°C.
Extraction And Purification Of DNA
Genomic DNA (gDNA) was extracted using DNAzol® (Thermo Fisher, Paisley, UK) according to the supplier’s instructions. Isolated gDNA was analysed by 0.8% agarose gel electrophoresis to evaluate its quality. The amount of DNA was determined by the 260 nm/280 nm ratio using Genesys 10S UV-Vis (Thermo Scientific)
Subsequently, DNA purification was performed using a QIAamp DNA Mini Kit (Qiagen)
TaqMan Mutation Detection Assay (castPCRTM)
The following TaqMan assays were designed for the detection of IDH1 and IDH2 gene mutations (GenBank Accession number, NM005896.3 and NM_002168.2, respectively): c.395 G>A p.R132H (Hs00000981_mu); c.394 C>T p.R132C (Hs00000982_mu); c.532 G>A p.V178I; c.315 G>T p.G105G; c.515 G>A p.R172K; c.419 G>A p.R140Q. CastPCRTM analysis was performed using a real-time PCR System (Step OnePlus™ Real-Time PCR System, Applied Biosystems, USA, CA). The Master mix was prepared as recommended by the supplier. A total of 50 ng of gDNA per reaction and the probes described above were used. The cycling conditions were as follows: pre-PCR read 60°C for 30 s; holding stage 50°C for 2 min, 95°C for 10 min; cycling stage 95°C for 15 s, 60°C for 1 min for 40 cycles; and post-PCR 60°C for 30 s.
For each of the analysed IDH1/2 mutations, the limit of detection (LOD) of castPCR TM was determined by constructing dilution curves of samples from patients with and without IDH1/2 gene mutations. Each point was determined using different dilutions (1:1 to 1:50) of the mutated sample and a non-mutated sample (Figure 1).
Statistical Analysis
Multivariate analysis was performed based on the clinical parameters and the quantification of the mutations. Kaplan-Meier and log rank analyses were performed to assess survival in relation to each mutation; differences were considered significant when p ≤ 0.05. SPSS software version 23 Statistical Package for Social Sciences, SPSS Inc, Chicago IL, USA) was used for the statistical analysis.
Results
Frequency And Clinical Association Of IDH Mutations In AML Patients
The frequency of IDH mutations in AML patients was 19.8% (20/101). In the particular case of the IDH1 gene, the frequency of mutations was 13.8% (14/101); the mutations identified included R132H, with a frequency of 3.9% (4/101), and V178I, with a frequency of 3.9% (4/101), while G105G (2/101) and R132C (2/101) exhibited a frequency of 1.9%. Two patients had two mutations, R132H and R132C, resulting in a frequency of 1.9% (2/101). The mutation frequency of the IDH2 gene was 5.9% (6/101); the variants included R172K, with a frequency of 3.9% (4/101), and R140Q, with a frequency of 1.9% (2/101) (Table 2).
 |
Table 2 Frequency Of Mutations Of The IDH Gene |
Regarding the association between the karyotype and the presence of IDH gene mutations, 12% of patients did not present tumour growth. However, 21% of patients with a normal karyotype had mutations. The patient with an abnormal karyotype had no mutation in the IDH1 gene; in the case of IDH2, 1.8% of patients did not present tumour growth, and 12.19% of patients had a normal karyotype
Overall Survival Analysis In Patients With IDH1/2 Gene Mutations
The mean survival time of patients without IDH1 gene mutations was 173.15 days (120–226), while the mean survival time of patients with mutations was 54.95 days (9–100). Of the patients with mutations of this gene (n = 14), 85.7% died (12/14), log rank p = 0.010 (Figure 2). Among the six patients who presented mutations of the IDH2 gene, 66.7% died. The mean survival time in patients without mutations was 157.3 days (110–204), while in those with mutations, the mean survival time was 74.11 days (30–117). According to the log rank analysis (p = 0.829), there were no differences between the groups (Figure 3).
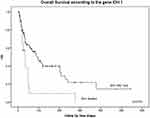 |
Figure 2 Global survival (OS) in patients with AML with mutated IDH1 gene. Of the patients with mutations in this gene, 85.7% died (12/14) (log rank p = 0.010). |
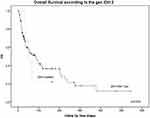 |
Figure 3 Global survival (OS) in patients with AML with mutated IDH2 gene. Of the patients with mutations in this gene, 66.7% died. There were no differences after the logrank test (p = 0.829, Figure 2). |
Association Of IDH Mutations With The Prognosis
The impact of different clinical variables on a favourable response to remission induction (complete remission or partial response versus therapeutic failure due to refractoriness or death) as well as its impact on survival was analysed. Individually, clinical variables and age older than 60 years (OR 3.777, 1.45–9.85), intermediate-high risk (OR: 1.936, 0.83–4.51) and mutations in IDH, especially IDH2 (OR 7.974, 0.4362–145.78), were associated with an increased risk of therapeutic failure. Among these variables, patients who were diagnosed after 60years of age (p = 0.006, 95% CI) and who required low-intensity treatment (p = 0.045, 95% CI) presented a significant risk for therapeutic failure. When evaluating the effect on medium-term survival, the IDH1 mutation (OR: 4.65, p = 0.052, 95% CI) and the presence of a leukocyte count above 30 × 109/L at the time of diagnosis (OR: 3.33, p = 0.008, 95% CI) showed significant impacts, and unlike the response to induction therapy, both low-intensity treatment and age did not show an impact on survival. The different risk values of each variable are described in Table 3.
 |
Table 3 AML Patients Mortality And OR Model According To Mutations In IDH Gene |
Discussion
In recent years, the biological roles of IDH enzymes in cancer have been described, including adaptation to hypoxia, histone demethylation and chromatin remodelling. However, the presence of mutations at the DNA level in these enzymes produces an increase in the production of the 2-HG oncometabolite, causing blockage of cell differentiation by inhibiting the activity of chromatin remodelling enzymes.35 Due to the frequent occurrence of IDH1 gene mutations in solid tumours and mutations in the IDH2 gene in haematologic neoplasias,36 we found that the frequency of mutations in the IDH gene in AML patients was 19.8%, which is consistent with values reported in other studies, and these mutations increased at frequency of approximately 20% according to age.37 Our study population showed mutations at younger ages, which is consistent with the diagnosis of this neoplasm in other populations. IDH1 gene mutations have been reported to be less common than IDH2 mutations in AML.38 The IDH mutations identified in our AML patients included R132H, V178I, G105G and R132C, and R132H exhibited the highest frequency. In the case of the IDH2 gene, the mutations detected included R172K and R140Q. Other studies have reported that the R132C and R132H mutations present greater frequencies in the IDH1 gene.39 In contrast to previous reports indicating a higher frequency of IDH2 mutations in AML, we found a higher frequency of IDH1 mutations due to the specificity and sensitivity of the castPCRTM technique, which had greater specificity and sensitivity than Sanger sequencing.
In the case of the G105G variant, a frequency of 10.6% has been reported. This is important because this variant can be a prognostic marker in patients with intermediate-risk FLT3-negative disease and can become a potential marker that benefits patients due to the development of new treatment alternatives.40,41 We found a frequency of 1.9% for this variant, which is much lower than that reported in the literature. In the case of the IDH2 gene, the mutations present included R140Q and R172H, the latter of which has been reported in adult patients.42 Only two AML patients showed two mutations in the IDH1 gene, R132H and R132C, and IDH1 and IDH2 mutations have been reported to be present in the same patient.43,44
The advent of NGS technologies has accelerated the discovery of new genetic alterations in AML.45,46 Among the main mutations detected are those in the FLT3, NPM1, CEBPA, MLL, NRAS, KIT, WT1, RUNX1, TET2, IDH1/2, DNMT3A, ASXL1, PHF6, SRSF2 and PTPN11 genes,47–49 indicating that these genes may impact the prognosis of AML patients.50,51 For example, mutations in FLT3 (37–46%) indicate unfavourable prognoses; in contrast, mutations in NPM1 (48–53%) and CEBPA (13–15%) indicate a better prognosis.52 In the case of mutations in DNMT3 and TET2, the prevalence rates of these mutation in the Mexican population are 2.7% and 11.8%, respectively, and they indicate an unfavourable prognosis.50 The prognostic impact of IDH gene mutations in AML remains controversial. Some studies have associated these mutations with adverse reactions, while other studies have not been able to identify an association with the clinical response or survival.53,54 In the case of gliomas and glioblastomas, IDH1/2 mutations have been associated with increased survival; therefore, the use of IDH inhibitors is not necessary, unlike for AML55 A meta-analysis that included 8,121 AML patients showed that those with mutations in the IDH1 gene had a lower overall survival and a lower rate of complete remission than patients without mutations.56 We found that AML patients with IDH1 mutations had decreased survival, which is consistent with previous reports. In the case of IDH2 gene mutations, no difference in survival was reported. These results agree with those reported for the IDH2 gene, in which the presence of a mutation has no effect on overall survival and complete remission.57,58 However, mutations have been associated with lower rates of complete remission and higher rates of relapse, which is similar to our results.
Finally, castPCRTM technology is considered a rapid and economical method for clinical practice that can be used as a diagnostic test for the detection of IDH1/2 gene mutations in AML.
Conclusion
The study of castPCRTM mutations allows rapid and timely diagnosis for the treatment of AML patients, and the importance of detecting other mutations, such as FLT3, TET2 and DNMT3, has been demonstrated. Our results revealed the frequency of IDH mutations in our population of AML patients and their impact on overall survival and risk of therapy failure. The presence of IDH gene mutations allows stratification of patients by risk group. In Mexico, there are no studies that demonstrate the frequency of these mutations to assess specific therapies, such as the use Ofivosidenib (Tibsovo), an IDH1 inhibitor, and Enasidenib (Idhifa), an IDH2 inhibitor.
Acknowledgments
This project was supported by CELGENE (AG221-TR-AML-PI-007979). This study was approved by the Ethics Committee of Hospital General of Mexico (Registration Number: HGM/DI/16/103/3/115). Clinical and informed consent was obtained from each patient or their family members.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Dohner H, Weisdorf DJ, Bloomfield CD. Acute myeloid leukemia. N Engl J Med. 2015;373:1136–1152. doi:10.1056/NEJMra1406184
2. Vardiman JW, Thiele J, Arber DA, et al. The 2008 revision of theWorldHealthOrganization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and importantchanges. Blood. 2009;114:937–951. doi:10.1182/blood-2009-03-209262
3. Rowe JM. AML in 2017: advances in clinical practice. Best Pract Res Clin Haematol. 2017;30:283–286. doi:10.1016/j.beha.2017.09.010
4. Mardis ER, Ding L, Dooling DJ, et al. Recurring mutations found by sequencing an acute myeloid leukemia genome. N Engl J Med. 2009;361:1058–1066. doi:10.1056/NEJMoa0903840
5. Conway O’Brien E, Prideaux S, Chevassut T. The epigenetic landscape of acute myeloid leukemia. Adv Hematol 2014. 2014;1. doi:10.1155/2014/103175
6. Marcucci G, Haferlach T, Dohner H. Molecular genetics of adult acute myeloid leukemia: prognostic and therapeutic implications. J ClinOncol. 2011;29:475–486. doi:10.1200/JCO.2010.30.2554
7. Patel JP, Gonen M, Figueroa ME, et al. Prognosticrelevance of integratedgeneticprofiling in acutemyeloidleukemia. N Engl J Med. 2012;366:1079–1089. doi:10.1056/NEJMoa1114705
8. Bertoli S, Bories P, Béné MC, et al. Prognostic impact of day 15 blast clearance in risk-adapted remission induction chemotherapy for younger patients with acute myeloid leukemia: long-term results of the multicenter prospective LAM-2001 trial by the GOELAMS study group. Haematologica. 2014;99(1):46–53. doi:10.3324/haematol.2013.091819
9. Brandwein JM, Zhu N, Kumar RLeber B, et al. Treatment of older patients with acute myeloid leukemia (AML): revised Canadian consensus guidelines. Am J Blood Res. 2017;7(4):30–40.
10. Bohl SR, Bullinger L, Rücker FG. New targeted agents in acute myeloid leukemia: new hope on the rise. Int J Mol Sci. 2019;20:8. doi:10.3390/ijms20081983
11. Kayser S, Levis MJ. Advances in targeted therapy for acute myeloid leukaemia. Br J Haematol. 2018;180(4):484–500. doi:10.1111/bjh.15032
12. Molenaar RJ, Maciejewski JP, Wilmink JW, van Noorden CJF. Wild-type and mutated IDH1/2 enzymes and therapy responses. Oncogene. 2018;37(43):5810. doi:10.1038/s41388-018-0455-1
13. Montalban-Bravo G, Di Nardo CD. The role of IDH mutations in acute myeloid leukemia. Future Oncol. 2018;14(10):979–993. doi:10.1038/s41388-017-0077-z
14. Tommasini- Ghelfi S, Murnan K, Kouri FM, Mahajan AS, May JL, Stegh AH. Cancer-associated mutation and beyond: the emerging biology of isocitrate dehydrogenases in human disease. Sci Adv. 2019;5(5):4593. doi:10.1126/sciadv.aaw4543
15. Medeiros BC, Fathi AT, DiNardo CD, Pollyea DA, Chan SM. Swords R Isocitrate dehydrogenase mutations in myeloid malignancies. Leukemia. 2017;31(2):272–281. doi:10.1038/leu.2016.275
16. Dang L, Yen K, Attar EC. IDH mutations in cancer and progress toward development of targeted therapeutics. Ann Oncol. 2016;27(4):599–608. doi:10.1093/annonc/mdw013
17. Petrova L, Vrbacky F, Lanska M, Zavrelova A, Zak P, Hrochova K. IDH1 and IDH2 mutations in patients with acute myeloid leukemia: suitable targets for minimal residual disease monitoring? Clin Biochem. 2018;61:34–39. doi:10.1016/j.clinbiochem.2018.08.012
18. Ferret Y, Boissel N, Helevaut N, et al. Clinical relevance of IDH1/2 mutant allele burden during follow-up in acute myeloid leukemia. A study by the French ALFA group. Haematologica. 2018;103(5):822–829. doi:10.3324/haematol.2017.183525
19. Dang L, Jin S, Su SM. IDH mutations in glioma and acute myeloid leukemia. Trends Mol Med. 2010;16:387–397. doi:10.1016/j.molmed.2010.07.002
20. Dang L, White DW, Gross S, et al. Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature. 2010;465(7300):966. doi:10.1038/nature09132
21. Tommasini-Ghelfi S, Murnan K, Kouri FM, Mahajan AS, May JL. Stegh AH cancer-associated mutation and beyond: the emerging biology of isocitrate dehydrogenases in human disease. Cancer-associated 739-44. Sci Adv. 2019;5(5):eaaw4543. doi:10.1126/sciadv.aaw4543
22. Kaminska B, Czapski B, Guzik R, Król SK, Gielniewski B. Consequences of IDH1/2 mutations in gliomas and an assessment of inhibitors targeting mutated IDH proteins. Molecules. 2019;24(5). doi:10.3390/molecules24050968
23. Reiter-Brennan C, Semmler L, Klein A. The effects of 2-hydroxyglutarate on the tumorigenesis of gliomas. Contemp Oncol (Pozn). 2018;22(4):215–222. doi:10.5114/wo.2018.82642
24. Ward PS, Patel J, Wise DR, et al. The commonfeature of leukemia-associated IDH1 and IDH2 mutationsis a neomorphic enzyme activity converting alpha-ketoglutarateto 2-hydroxyglutarate. CancerCell. 2010;17:225–234.
25. Medeiros BC, Fathi AT, DiNardo CD, Pollyea DA, Chan SM, Swords R. Isocitrate dehydrogenase mutations in myeloid malignancies. Leukemia. 2017;31(2):272–281. doi:10.1038/leu.2016.275
26. Garrett-Bakelman FE, Melnick AM, Mutant IDH. A targetable driver of leukemic phenotypes linking metabolism, epigenetics and transcriptional regulation. Epigenomics. 2016;8(7):945–957. doi:10.2217/epi-2016-0008
27. Barbano R, Pasculli B, Coco M, et al. Competitiveallele-specificTaqMan PCR (Cast-PCR) is a sensitive, specific and fast method for BRAF V600 mutation detection in Melanoma patients. Sci Rep. 2015;5:18592. doi:10.1038/srep18592
28. Bolton L, Reiman A, Lucas K, Timms J, Cree IA. KRAS mutation analysis by PCR: a comparison of two methods. PLoS One. 2015;10(1):e0115672. doi:10.1371/journal.pone.0115672
29. Yang Y, Shen X, Li R, Shen J, Zhang H, Yu L. The detection and significance of EGFR and BRAF in cell-free DNA of peripheral blood in NSCLC. Oncotarget. 2017;8(30):49773–49782. doi:10.18632/oncotarget.17937
30. Bronte G, Silvestris N, Castiglia M, et al. New findings on primary and acquired resistance to anti-EGFR therapy in metastatic colorectal cancer: do all roads lead to RAS? Oncotarget. 2015;6(28):24780–24796. doi:10.18632/oncotarget.4959
31. Yang Y, Meng Y, Zhang H, et al. Detection of EGFR and BRAF mutations by competitive allele-specific TaqMan polymerase chain reaction in lung adenocarcinoma. Oncol Lett. 2018;15(3):3295–3304. doi:10.3892/ol.2017.7652
32. Gao J, Wu H, Wang L, et al. Validation of targeted next-generation sequencing for RAS mutation detection in FFPE colorectal cancer tissues: comparison with Sanger sequencing and ARMS-Scorpion real-time PCR. BMJ Open. 2016;6:e009532. doi:10.1136/bmjopen-2015-009532
33. Huebner C, Weber R, Lloydd RA. HRM assay for identification of low level BRAF V600E and V600K mutations using the CADMA principle in FFPE specimens. Pathology. 2017;49(7):776–783. doi:10.1016/j.pathol.2017.08.011
34. Woo C, Mouanoutoua M, Moy B, et al. Validation of the Ion AmpliSeq™ comprehensive cancer panel (CCP) using castPCR™ technologies. Cancer Res. 2013;73(8 Suppl):S4218. doi:10.1158/1538-7445.AM2013-4218
35. Inoue S, Li WY, Tseng A, et al. Mutant IDH1 downregulates ATM and alters DNA repair and sensitivity to DNA damage independent of TET2. CancerCell. 2016;30(2):337–348. doi:10.1016/j.ccell.2016.05.018
36. Wiehle L, Raddatz G, Pusch S, et al. mIDH-associated DNA hypermethylation in acute myeloid leukemia reflects differentiation blockage rather than inhibition of TET-mediated demethylation. Cell Stress. 2017;1(1):55–67. doi:10.15698/cst2017.10.106
37. Buege MJ, DiPippo AJ, DiNardo CD. Evolving treatment strategies for elderly leukemia patients with IDH mutations. Cancers (Basel). 2018;10:6. doi:10.3390/cancers10060187
38. Fathi AT, Wander SA, Faramand R, Emadi A. Biochemical, epigenetic, andmetabolicapproachesto target IDH mutations in acutemyeloidleukemia. SeminHematol. 2015;52:165–171. doi:10.1053/j.seminhematol.2015.03.002
39. Im AP, Sehgal AR, Carroll MP, et al. DNMT3A and IDH mutations in acute myeloid leukemia and other myeloid malignancies: associations with prognosis and potential treatment strategies. Leukemia. 2014;28:1774–1783. doi:10.1038/leu.2014.124
40. Stein EM. IDH2 inhibition in AML: finallyprogress? Best Pract Res Clin Haematol. 2015;28:112–115. doi:10.1016/j.beha.2015.10.016
41. Willander K, Falk IJ, Chaireti R, et al. Mutations in the isocitrate dehydrogenase 2 gene and IDH1 SNP 105C4T have a prognostic value in acute myeloid leukemia. Biomark Res. 2014;2:18. doi:10.1186/2050-7771-2-18
42. Marcucci G, Maharry K, Wu YZ, et al. IDH1 and IDH2 gene mutations identify novel molecular subsets within de novo cytogenetically normal acute myeloid leukemia: a cancer and leukemiaGroupB study. J ClinOncol. 2010;28:2348–2355. doi:10.1200/JCO.2009.27.3730
43. Platt MY, Fathi AT, Borger DR, et al. Detectionof dual IDH1 and IDH2 mutations by targeted next-generation sequencing in acute myeloid leukemia and myelodysplastic syndromes. J Mol Diagn. 2015;17:661–668. doi:10.1016/j.jmoldx.2015.06.004
44. DiNardo CD, Ravandi F, Agresta S, et al. Characteristics, clinical outcome, and prognostic significance of IDH mutations inAML. Am J Hematol. 2015;90:732–736. doi:10.1002/ajh.24072
45. Sanders MA, Valk PJ. The evolving molecular genetic landscape in acute myeloid leukaemia. Curr Opin Hematol. 2013;20:79–85. doi:10.1097/MOH.0b013e32835d821c
46. Greif PA, Hartmann L, Vosberg S, et al. Evolution of cytogenetically normal acute myeloid leukemia during therapy and relapse: an exome sequencing study of 50 patients. Blood Cancer J. 2017;7:e559. doi:10.1038/bcj.2017
47. Grimwade D, Hills RK, Moorman AV, et al. Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood. 2010;116:354–365. doi:10.1182/blood-2009-11-254441
48. Togasaki E, Takeda J, Yoshida K, et al. Frequent somatic mutations in epigenetic regulators in newly diagnosed chronic myeloid. Blood Cancer J. 2017;7:e559. doi:10.1038/bcj.2017.36
49. Schlenk RF, Dohner K, Krauter J, et al. Mutations and treatment outcome in cytogenetically normal acute myeloid leukemia. N Engl J Med. 2008;358:1909–1918. doi:10.1056/NEJMoa074306
50. Ponciano-Gómez A, Martínez-Tovar A, Vela-Ojeda J, Olarte-Carrillo I, Centeno-Cruz F, Garrido E. Mutations in TET2 and DNMT3A genes are associated with changes in global and gene-specific methylation in acutemyeloid leukemia. Tumour Biol. 2017;39(10):1010428317732181. doi:10.1177/1010428317732181
51. Chaudry SF, Chevassut TJ. Epigenetic guardian: a review of the DNA Methyltransferase DNMT3A in acute myeloid leukaemia and clonal haematopoiesis. Biomed Res Int. 2017;2017:5473197. doi:10.1155/2017/5473197
52. Uy GL, Duncavage EJ, Chang GS, et al. Dynamic changes in the clonal structure of MDS and AML in response to epigenetic therapy. Leukemia. 2017;31(4):872–881. doi:10.1038/leu.2016.282
53. Aref S, KamelAreida ES, Abdel Aaal MF, et al. Prevalence and clinical effect of IDH1 and IDH2 mutations among cytogenetically normal acute myeloid leukemia patients. Clin Lymphoma Myeloma Leuk. 2015;15:550–555. doi:10.1016/j.clml.2015.05.009
54. Paschka P, Schlenk RF, Gaidzik VI, et al. IDH1and IDH2 mutations are frequent genetic alterations in acute myeloid leukemia and confer adverse prognosis in cytogenetically normal acute myeloid leukemia with NPM1 mutation without FLT3 internaltandem duplication. J ClinOncol. 2010;28:3636–3643. doi:10.1200/JCO.2010.28.3762
55. Chotirat S, Thongnoppakhun W, Promsuwicha O, Boonthimat C, Auewarakul CU. Molecular alterations of isocitratedehydrogenase 1 and 2 (IDH1 and IDH2) metabolic genes and additional genetic mutations in newly diagnosed acute myeloid leukemia patients. J HematolOncol. 2012;5:5. doi:10.1186/1756-8722-5-5
56. Abbas S, Lugthart S, Kavelaars FG, et al. Acquired mutations in the genes encoding IDH1 and IDH2 both are recurrent aberrations in acute myeloid leukemia: prevalence and prognostic value. Blood. 2010;116:2122–2126. doi:10.1182/blood-2009-11-250878
57. Feng JH, Guo XP, Chen YY, Wang ZJ, Cheng YP, Tang YM. Prognostic significance of IDH1 mutations in acute myeloid leukemia: a meta-analysis. Am J Blood Res. 2012;2:254–264.
58. Thol F, Damm F, Wagner K, et al. Prognostic impact of IDH2 mutations in cytogenetically normal acute myeloid leukemia. Blood. 2010;116:614–616. doi:10.1182/blood-2010-03-272146
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
