Back to Journals » Journal of Pain Research » Volume 15
Description of Clinical Features and Diagnoses of 444 Cases with Neck-Shoulder-Upper Extremity Pain: A Single-Center Retrospective Review
Authors Zhang H , Luo W, Li C, Zhao J, Zhang Q, Gu R
Received 29 June 2022
Accepted for publication 25 October 2022
Published 2 November 2022 Volume 2022:15 Pages 3483—3492
DOI https://doi.org/10.2147/JPR.S376205
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Alaa Abd-Elsayed
Hongchao Zhang, Wenqi Luo, Chaoyuan Li, Jianhui Zhao, Qiao Zhang, Rui Gu
Department of Orthopedics, The Multidisciplinary Consultation Center of Neck Shoulder Upper Extremity, China-Japan Union Hospital of Jilin University, Changchun, Jilin, People’s Republic of China
Correspondence: Qiao Zhang; Rui Gu, Department of Orthopedics, The Multidisciplinary Consultation Center of Neck Shoulder Upper Extremity, China-Japan Union Hospital, Jilin University, No. 126 Xiantai Street, Changchun, Jilin Province, 130033, People’s Republic of China, Tel +86 13578793723 ; +86 13804371075, Fax +86431-89876939, Email [email protected]; [email protected]
Purpose: Neck-shoulder-upper extremity pain (NSUEP) is a frequently occurring clinical constellation of syndromes. However, its etiology is complicated, and the diagnosis is challenging. We aimed to present detailed clinical characteristics and diagnoses of NSUEP from a single center and heighten clinicians’ understanding of this condition.
Patients and Methods: Prospectively collected databases were used to retrospectively evaluate patients with NSUEP who underwent treatment at the multidisciplinary consultation center for neck, shoulder, and upper extremity pain at the China-Japan Union Hospital of Jilin University between April 2014 and July 2021. We performed descriptive statistics regarding demographic data, symptoms, findings of physical and radiographic examinations, and each patient’s diagnosis.
Results: Development of NSUEP was primarily observed in individuals aged between 51 and 60 years (n = 157, 35.4%). Patients were most commonly referred for upper extremity pain (n = 306, 68.9%). Patients with upper extremity pain presented with hypoesthesia (n = 139, 45.4%), muscle weakness (n = 93, 30.4%), muscle atrophy (n = 90, 29.4%), hyperesthesia (n = 39, 12.7%), and turgidity (n = 18, 5.9%). Among the 22 patients with upper extremity swelling, 8 (36.4%) were diagnosed with autoimmune rheumatic diseases. Among the 352 patients with a single diagnosis, 51 (14.5%) presented with thoracic outlet syndrome, 49 (13.9%) with cervical radiculopathy, 16 (4.5%) with carpal tunnel syndrome, and 16 (4.5%) with brachial plexus injury. Further, among the 92 patients with compound diagnosis, 18 patients (19.6%) were diagnosed with cervical radiculopathy.
Conclusion: Among the NSUEP patients in this study, older individuals were the largest group. Pain, numbness, weakness, and mobility limitation are common complaints accompanying NSUEP. The common etiologies of NSUEP include cervical spondylosis, thoracic outlet syndrome, carpal tunnel syndrome, and brachial plexus injury. In addition, autoimmune rheumatic diseases should be considered in patients with NSUEP and swelling.
Keywords: neck, shoulder, upper extremity, pain, retrospective study, Spurling’s test
Introduction
Neck-shoulder-upper extremity pain (NSUEP) refers to a constellation of syndromes accompanied by neck, shoulder, or upper extremity pain. NSUEP includes at least one region of pain in the neck, shoulders, or upper extremities. Self-reported patient surveys indicate the prevalence of neck and upper limb pain at the 1-month point was 44%.1 Previous studies have also shown that the 12-month-period prevalence of neck pain is 31.4%, shoulder pain is 30.3%, elbow pain is 11.2%, and wrist or hand pain is 17.5% in the general population.2
 |
Figure 1 Flow diagram of patient selection. |
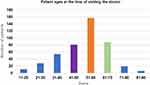 |
Figure 2 Age distribution of the 444 patients at the time of visit. The individuals who developed NSUEP are primarily between 51–60 years old (157 patients, 35.4%). |
 |
Figure 3 The regions of pain distribution of patients with NSUEP. The most common region of pain was the upper extremity. |
 |
Figure 4 Symptom distribution of patients with NSUEP. Numbness, weakness, and limited activity are common symptoms in addition to pain. |
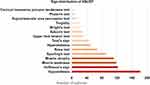 |
Figure 5 Sign distribution of patients with NSUEP. Hypoesthesia, Hoffmann’s sign, muscle weakness, muscle atrophy, and Spurling’s test were common signs. |
 |
Figure 6 Patients with a single diagnosis classified by department. |
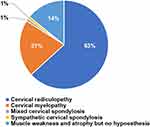 |
Figure 7 The diagnosis of cervical spondylosis was classified into five types by diagnostic category. |
 |
Table 1 Frequency and Percentage of the Clinical Signs of NSUEP by the Regions of Pain |
 |
Table 2 Diagnosis Rates of NSUEP According to the Clinical Signs |
 |
Table 3 Patients with Cervical Radiculopathy with Compound Diagnosis |
Machino et al3 reported that neck and shoulder pain was related to poor health-related quality of life in a middle-aged community-living population. Patients with NSUEP were associated with the existence of a variety of symptoms, resulting in impaired quality of life and also high societal costs.4 In Sweden, neck and shoulder problems account for 18% of all disability payments.5 In addition, the combination of the high incidence of such complaints and complex etiology causes many patients with no clear diagnosis.6 The treatments included non-pharmacological and pharmacological therapies7 and invasive/surgical interventions when significant pathology was involved.8
This study reviewed the prospective clinical data of the patients with NSUEP who visited the multidisciplinary consultation center for neck, shoulder, and upper extremity pain between 2014 and 2021. We aimed to present detailed clinical characteristics and diagnoses of NSUEP from a single center and heighten clinicians’ understanding of this condition.
Materials and Methods
All patients underwent treatment at the multidisciplinary consultation center for neck, shoulder, and upper extremity pain at the China-Japan Union Hospital of Jilin University between April 2014 and July 2021. The clinical data were prospectively collected, and we evaluated it retrospectively. This study ethics approval from the Institutional Review Board of the China-Japan Union Hospital of Jilin University (approval No.20220628022). All included patients signed an informed consent form to use their anonymized clinical data for scientific purposes. Our study was performed in accordance with the principles of the Declaration of Helsinki and its later amendments.
A multidisciplinary team is composed of core experts from six major departments: spine surgery, hand surgery, neurology, pain, rheumatology, and vascular surgery. Patients who met either of the following criteria were eligible for consultation: 1) patients who visited two or more specialties with an unclear diagnosis or inadequate treatment, or 2) if a single core expert failed to give advice on diagnosis or treatment, patients were referred for consultation at the multidisciplinary consultation center for neck, shoulder, and upper extremity (Figure 1). The clinician determines to rule in or out a limited range of motion by physical evaluation. Measuring includes a cervical active range of motion, the cervical flexion-rotation test, cervical thoracic segmental mobility tests, and active or passive range of motion in the joints of the shoulder, elbow, or wrist-hand-fingers.5,9–11 Muscle weakness assessed by manual muscle testing.12,13 The diagnoses of the patients or treatment plan were decided by mutual agreement by the core experts of the team based on their expertise in light of the clinical presentation and clinical experience (each of the core experts > 10 years of experience in the treatment of NSUEP). The patients’ data, including demographic and clinical data, and treatment recommendations, were recorded by consulting experts and trained clinicians.
Two independent observers screened patients through a review of the consultation records. Our sample population includes patients with NSUEP who met the eligibility criteria: 1) at least one region of pain in the neck, shoulders, or upper extremities, 2) a clear diagnosis and treatment recommendations were included, and 3) complete clinical data (Figure 1).
Based on available data, the clinical characteristics of NSUEP were subdivided into three main categories: symptoms, signs (including objective signs, provocative test, and ancillary test), and treatments. The diagnoses were categorized as single or compound diagnoses. The compound diagnosis was defined as the “diagnosis of two or more diseases.” Data were entered into a Microsoft Excel (Version 16.0) database. Descriptive statistics are presented for patient clinical features and diagnoses. Frequency and percentages were used for categorical variables, and the mean was estimated for continuous variables.
Results
A total of 444 patients with NSUEP participated in this study. Female and male patients constituted 50.9% (n = 226) and 49.1% (n = 218) of the participants, respectively. The oldest patient was 88 years old, while the youngest patient was 11 years old. The mean age of the total study population was 51.5 years. The proportion of NSUEP was highest in individuals between the ages of 51 and 60 (n = 157, 35.4%) (Figure 2).
Symptoms
Patients were most commonly referred for upper extremity pain (n = 306, 68.9%) (Figure 3). Patients with NSUEP complained of numbness (n = 189), weakness (n = 56), mobility limitation (n = 52), muscle atrophy (n = 49), dizziness (n = 23), turgidity (n = 19), neck muscle stiffness14 (n = 17), stiffness of other muscles (n = 11), and tinnitus (n = 5) (Figure 4). The shortest history of symptoms was 3.5 h, whereas the longest was 50 years. The average duration of symptoms reported by the patients was 23.55 months.
Signs
Patients of NSUEP presented with hypoesthesia, muscle weakness, muscle atrophy, hyperesthesia, and turgidity, patients with upper extremity pain accounted for 45.4%, 30.4%, 29.4%, 12.7%, 5.9% in each sign mentioned before, respectively (Table 1). Hypoesthesia (n = 182, 41.0%), Hoffmann’s sign (n = 122, 27.5%), muscle weakness (n = 118, 26.6%), muscle atrophy (n = 111, 25.0%), and Spurling’s test (n = 91, 20.5%) are easily manifested (Figure 5).
Among the 22 patients with upper extremity turgidity, 8 (36.4%) were diagnosed with autoimmune rheumatic diseases (Table 2). Among the 67 patients with cervical radiculopathy, 36 (53.7%) had positive Spurling’s test. Sixty-six patients were diagnosed with thoracic outlet syndrome, including 32 (48.5%) with a positive Roos test, 18 (27.3%) with a positive Adson’s test, 15 (22.7%) with a positive upper limb tension test, and 12 (18.2%) with a positive Wright’s test.
Diagnoses
Among the 444 patients with NSUEP, 106 (23.9%) were diagnosed with cervical spondylosis, 67 (15.1%) with cervical radiculopathy, and 66 (14.9%) with thoracic outlet syndrome. Among the 352 patients with a single diagnosis, spinal surgical, hand surgical, and neurological diseases accounted for a relatively high proportion (Figure 6). Fifty-one patients (14.5%) presented with thoracic outlet syndrome, 49 (13.9%) with cervical radiculopathy, 16 (4.5%) with carpal tunnel syndrome, and 16 (4.5%) with brachial plexus injury. The remaining 92 patients received a compound diagnosis: 18 (19.6%) diagnosed with cervical radiculopathy (Table 3) and 15 (16.3%) with thoracic outlet syndrome.
Among the 106 patients with cervical spondylosis, 67 (63.2%) were diagnosed with cervical radiculopathy, 22 (20.8%) diagnosed with cervical myelopathy, and 1 (0.9%) diagnosed with mixed cervical spondylosis and sympathetic cervical spondylosis. Additionally, 15 (14.2%) patients with cervical spondylosis experienced muscle weakness and atrophy without hypoesthesia (Figure 7).
Treatments
Of the 444 patients with NSUEP, 170 (38.3%) were recommended for conservative therapy. A total of 164 cases (36.9%) were recommended for surgical treatment, including 84 requiring hand surgery, 74 requiring spine surgery, 6 requiring neurosurgery, and 1 requiring vascular surgery. In addition, scalene block injection was recommended in 10 cases. Ninety-nine patients (22.3%) were recommended for medical treatment, including 24 for neurology treatments and 21 for rheumatology treatments. Moreover, 11 patients (2.5%) required combined treatment from multiple departments.
Discussion
In this study, the proportion of patients with NSUEP increased with age until 51–61, after which it declined. This variation with age is also described in other studies.15 The higher proportion of NSUEP in older individuals may be related to the different priorities for pain and other health problems or the normalization of pain in older individuals.16 The mean duration of symptoms reported by the patients was 23.55 months. In a study investigating whether lag signs were valid tools in diagnosing full-thickness tears of the rotator cuff, the average time since onset of shoulder pain was 37.5 months.17 Among the 22 patients with upper extremity turgidity, 8 (36.4%) were diagnosed with autoimmune rheumatic diseases, including rheumatoid arthritis, systemic sclerosis (scleroderma), and idiopathic inflammatory myositis. Autoimmune rheumatic diseases share many common features, such as constitutional disturbance, arthralgia and arthritis, myalgia, and neurological involvement.18,19 Therefore, autoimmune rheumatic diseases should be considered in patients with NSUEP and swelling.
Thoracic outlet syndrome and cervical spondylotic radiculopathy were the two most common diagnoses recorded at the multidisciplinary consultation center. In the case of thoracic outlet syndrome, it is common for patients to consult multiple specialists without a clear diagnosis or understanding of the cause of their symptoms due to the complex mechanisms involving compression in the area of the thoracic outlet by the brachial plexus, subclavian vein, or subclavian artery.20–22 Although provocative tests have limited sensitivity and specificity, positive tests increase the probability of diagnosing thoracic outlet syndrome.21,23 Imaging can also play an important role in identifying the underlying cause, supporting the diagnosis, and excluding other conditions.24
Scalene block injection was recommended in 10 patients. Scalene block injection may aid diagnosis in patients with complications and an unclear understanding of the cause of their symptoms.25 In addition, it can be useful in identifying patients who may respond favorably to surgery.26 According to Braun et al,27 the tight scalene muscles may cause the symptoms. A scalene block induces the scalene muscle temporary paralysis, resulting in decompression of the neurovascular elements in the scalene muscle space. The pain may reduce or disappear after the injection; paresthesia is considered a positive result. Multidisciplinary consultation is preferred if the clinical findings are atypical, in which case, electromyography and scalene blocking injection are recommended.
Cervical spondylotic radiculopathy was the most common type of cervical spondylosis. The classic clinical picture includes neck pain, paresthesia in the arms and hands in conjunction with diminished muscle tendon reflexes, sensory disturbances, and/or motor weakness.28 Clinically, Spurling’s test is valuable when the patient has symptoms consistent with radiculopathy. Among the 67 patients with cervical radiculopathy, 36 (53.7%) had positive Spurling’s test. Rubinstein et al29 reported that a calculation for Spurling’s test yielded a sensitivity of 52.9% and specificity of 93.8%. Some authors proposed that the sensitivity of Spurling’s test varied from moderate to high while its specificity was high.12,30
Cervical spondylotic amyotrophy is characterized by upper limb muscle weakness and atrophy without sensory deficits.31–33 In this study, among 106 patients with cervical spondylosis, muscle weakness, atrophy, and absence of hypoesthesia in the upper extremities were observed in 15 patients. These patients will be analyzed in detail in the follow-up study.
Our study focused on a group of patients with neck, shoulder, or upper extremity pain whose etiology is complex and difficult to diagnose. These descriptions can serve as a reference for health professionals caring for patients with NSUEP, including rheumatologists, neurologists, and general practitioners, as well as orthopedic surgeons. A multicenter study with a large sample size is required in the future to further clarify the clinical features and disease spectrum of NSUEP.
There were several limitations in our study. First, there were no standardized procedures during the assessment of the patients and data collection. Second, this study was a single-center study, and the generalizability is limited. Third, the findings are unsuitable for generalizing other levels of health care.
Conclusion
Patients with NSUEP are most commonly older individuals with typical complaints of numbness, weakness, and limited activity. Hypoesthesia, Hoffmann’s sign, muscle weakness, muscle atrophy, and Spurling’s test are easily manifested. Cervical spondylosis, thoracic outlet syndrome, carpal tunnel syndrome, and brachial plexus injury are prevalent in patients with NSUEP. Autoimmune rheumatic diseases should be considered in patients with NSUEP and swelling.
Abbreviation
NSUEP, neck-shoulder-upper extremity pain.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study was supported by the Jilin Province Department of Finance (2018SCZ013: 2019SCZ023), Jilin Provincial Science and Technology Program (20200201341JC).
Disclosure
The authors report no conflicts of interest for this work.
References
1. Sim J, Lacey RJ, Lewis M. The impact of workplace risk factors on the occurrence of neck and upper limb pain: a general population study. BMC Public Health. 2006;6(1):234. doi:10.1186/1471-2458-6-234
2. Picavet HSJ, Schouten JS. Musculoskeletal pain in the Netherlands: prevalences, consequences and risk groups, the DMC3-study. Pain. 2003;102(1):167–178. doi:10.1016/s0304-3959(02)00372-x
3. Machino M, Ando K, Kobayashi K, et al. Impact of neck and shoulder pain on health-related quality of life in a middle-aged community-living population. BioMed Res Int. 2021;2021:6674264. doi:10.1155/2021/6674264
4. van Tilburg ML, Kloek CJJ, Pisters MF, et al. Stratified care integrated with eHealth versus usual primary care physiotherapy in patients with neck and/or shoulder complaints: protocol for a cluster randomized controlled trial. BMC Musculoskelet Disord. 2021;22:143. doi:10.1186/s12891-021-03989-0
5. Blanpied PR, Gross AR, Elliott JM, et al. Neck pain: revision 2017. J Orthop Sports Phys Ther. 2017;47:A1–A83. doi:10.2519/jospt.2017.0302
6. Storheil B, Klouman E, Holmvik S, Emaus N, Fleten N. Intertester reliability of shoulder complaints diagnoses in primary health care. Scand J Prim Health Care. 2016;34:224–231. doi:10.1080/02813432.2016.1207139
7. Kloppenburg M, Kroon FP, Blanco FJ, et al. 2018 update of the EULAR recommendations for the management of hand osteoarthritis. Ann Rheum Dis. 2019;78:16–24. doi:10.1136/annrheumdis-2018-213826
8. Côté P, Wong JJ, Sutton D, et al. Management of neck pain and associated disorders: a clinical practice guideline from the Ontario Protocol for Traffic Injury Management (Optima) Collaboration. Eur Spine J. 2016;25:2000–2022. doi:10.1007/s00586-016-4467-7
9. Kelley MJ, Shaffer MA, Kuhn JE, et al. Shoulder pain and mobility deficits: adhesive capsulitis. J Orthop Sports Phys Ther. 2013;43:A1–A31. doi:10.2519/jospt.2013.0302
10. van de Pol RJ, van Trijffel E, Lucas C. Inter-rater reliability for measurement of passive physiological range of motion of upper extremity joints is better if instruments are used: a systematic review. J Physiother. 2010;56(1):7–17. doi:10.1016/s1836-9553(10)70049-7
11. Diercks R, Bron C, Dorrestijn O, et al. Guideline for diagnosis and treatment of subacromial pain syndrome: a multidisciplinary review by the Dutch Orthopaedic Association. Acta Orthop. 2014;85(3):314–322. doi:10.3109/17453674.2014.920991
12. Thoomes EJ, van Geest S, van der Windt DA, et al. Value of physical tests in diagnosing cervical radiculopathy: a systematic review. Spine J. 2018;18(1):179–189. doi:10.1016/j.spinee.2017.08.241
13. Shefner JM. Strength testing in motor neuron diseases. Neurotherapeutics. 2017;14(1):154–160. doi:10.1007/s13311-016-0472-0
14. Dieterich AV, Yavuz UŞ, Petzke F, Nordez A, Falla D. Neck muscle stiffness measured with shear wave elastography in women with chronic nonspecific neck pain. J Orthop Sports Phys Ther. 2020;50(4):179–188. doi:10.2519/jospt.2020.8821
15. Bergman S, Herrström P, Högström K, Petersson IF, Svensson B, Jacobsson LT. Chronic musculoskeletal pain, prevalence rates, and sociodemographic associations in a Swedish population study. J Rheumatol. 2001;28(6):1369–1377.
16. Parsons S, Breen A, Foster NE, et al. Prevalence and comparative troublesomeness by age of musculoskeletal pain in different body locations. Fam Pract. 2007;24(4):308–316. doi:10.1093/fampra/cmm027
17. Miller CA, Forrester GA, Lewis JS. The validity of the lag signs in diagnosing full-thickness tears of the rotator cuff: a preliminary investigation. Arch Phys Med Rehabil. 2008;89(6):1162–1168. doi:10.1016/j.apmr.2007.10.046
18. Goldblatt F, O’Neill SG. Clinical aspects of autoimmune rheumatic diseases. Lancet. 2013;382(9894):797–808. doi:10.1016/S0140-6736(13)61499-3
19. Joseph A, Brasington R, Kahl L, Ranganathan P, Cheng TP, Atkinson J. Immunologic rheumatic disorders. J Allergy Clin Immunol. 2010;125(suppl 2):S204–S215. doi:10.1016/j.jaci.2009.10.067
20. Illig KA, Rodriguez-Zoppi E. How common is thoracic outlet syndrome? Thorac Surg Clin. 2021;31(1):11–17. doi:10.1016/j.thorsurg.2020.09.001
21. Laulan J, Fouquet B, Rodaix C, Jauffret P, Roquelaure Y, Descatha A. Thoracic outlet syndrome: definition, aetiological factors, diagnosis, management and occupational impact. J Occup Rehabil. 2011;21(3):366–373. doi:10.1007/s10926-010-9278-9
22. Grunebach H, Arnold MW, Lum YW. Thoracic outlet syndrome. Vasc Med. 2015;20(5):493–495. doi:10.1177/1358863X15598391
23. Gillard J, Pérez-Cousin M, Hachulla E, et al. Diagnosing thoracic outlet syndrome: contribution of provocative tests, ultrasonography, electrophysiology, and helical computed tomography in 48 patients. Joint Bone Spine. 2001;68(5):416–424. doi:10.1016/S1297-319X(01)00298-6
24. Raptis CA, Sridhar S, Thompson RW, Fowler KJ, Bhalla S. Imaging of the patient with thoracic outlet syndrome. RadioGraphics. 2016;36(4):984–1000. doi:10.1148/rg.2016150221
25. Brooke BS, Freischlag JA. Contemporary management of thoracic outlet syndrome. Curr Opin Cardiol. 2010;25(6):535–540. doi:10.1097/HCO.0b013e32833f028e
26. Jordan SE, Machleder HI. Diagnosis of thoracic outlet syndrome using electrophysiologically guided anterior scalene blocks. Ann Vasc Surg. 1998;12(3):260–264. doi:10.1007/s100169900150
27. Braun RM, Shah KN, Rechnic M, Doehr S, Woods N. Quantitative Assessment of Scalene Muscle Block for the Diagnosis of Suspected Thoracic Outlet Syndrome. J Hand Surg Am. 2015;40(11):2255–2261. doi:10.1016/j.jhsa.2015.08.015
28. Kuijper B, Tans JT, Schimsheimer RJ, et al. Degenerative cervical radiculopathy: diagnosis and conservative treatment. A review. Eur J Neurol. 2009;16(1):15–20. doi:10.1111/j.1468-1331.2008.02365.x
29. Rubinstein SM, Pool JJ, van Tulder MW, Riphagen II, de Vet HC. A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy. Eur Spine J. 2007;16(3):307–319. doi:10.1007/s00586-006-0225-6
30. Sleijser-Koehorst MLS, Coppieters MW, Epping R, Rooker S, Verhagen AP, Scholten-Peeters GGM. Diagnostic accuracy of patient interview items and clinical tests for cervical radiculopathy. Physiotherapy. 2021;111:74–82. doi:10.1016/j.physio.2020.07.007
31. Luo W, Li Y, Xu Q, Gu R, Zhao J. Cervical spondylotic amyotrophy: a systematic review. Eur Spine J. 2019;28:2293–2301. doi:10.1007/s00586-019-05990-7
32. Takahashi T, Hanakita J, Minami M, Tomita Y, Sasagasako T, Kanematsu R. Cervical spondylotic amyotrophy: case series and review of the literature. Neurospine. 2019;16:579–588. doi:10.14245/ns.1938210.105
33. Tauchi R, Imagama S, Inoh H, et al. Characteristics and surgical results of the distal type of cervical spondylotic amyotrophy. J Neurosurg Spine. 2014;21:411–416. doi:10.3171/2014.4.SPINE13681
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
