Back to Journals » Patient Preference and Adherence » Volume 17
Derivation and Validation of a Prognostic Model for Acute Decompensated Cirrhosis Patients
Authors Zhang Y, Chen P, Zhang W, Huang C, Zhu X
Received 24 March 2023
Accepted for publication 12 May 2023
Published 19 May 2023 Volume 2023:17 Pages 1293—1302
DOI https://doi.org/10.2147/PPA.S412063
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Yue Zhang,* Peng Chen,* Wang Zhang, Chenkai Huang,* Xuan Zhu*
Department of Gastroenterology, Jiangxi Province and Jiangxi Clinical Research Center for Gastroenterology, The First Affiliated Hospital of Nanchang University, Nanchang, Jiangxi, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xuan Zhu; Chenkai Huang, Department of Gastroenterology, Jiangxi Province and Jiangxi Clinical Research Center for Gastroenterology, the First Affiliated Hospital of Nanchang University, Nanchang, Jiangxi, People’s Republic of China, Email [email protected]; [email protected]
Background: Acute decompensated cirrhosis (AD) is related to high medical costs and high mortality. We recently proposed a new score model to predict the outcome of AD patients and compared it with the common score model (CTP, MELD and CLIF-C AD score) in the training and validation sets.
Materials and Methods: A total of 703 patients with AD were enrolled from The First Affiliated Hospital of Nanchang University between December 2018 and May 2021. These patients were randomly assigned to the training set (n=528) and validation set (n=175). Risk factors affecting prognosis were identified by Cox regression analysis and then used to establish a new score model. The prognostic value was determined by the area under the receiver operating characteristic curve (AUROC).
Results: A total of 192 (36.3%) patients in the training cohort and 51 (29.1%) patients in the validation cohort died over the course of 6 months. A new score model was developed with predictors including age, bilirubin, INR, WBC, albumin, ALT and BUN. The new prognostic score (0.022×Age + 0.003×TBil + 0.397×INR + 0.023×WBC- 0.07×albumin + 0.001×ALT + 0.038×BUN) for long-term mortality was superior to three other scores based on both training and internal validation studies.
Conclusion: This new score model appears to be a valid tool for assessing the long-term survival of AD patients, improving the prognostic value compared with the CTP, MELD and CLIF-C AD scores.
Keywords: new score, prognosis, CTP score, MELD score, CLIF-C AD score
Introduction
Liver cirrhosis is an end-stage liver disease caused by various etiologies, such as viral hepatitis, alcoholic hepatitis, and nonalcoholic steatohepatitis.1 Liver cirrhosis is divided into compensated cirrhosis and decompensated cirrhosis. The development of complications such as variceal bleeding, hepatic encephalopathy, jaundice and ascites formation herald the onset of acute decompensated cirrhosis (AD).2 The precipitant factor of AD may be derived from the major clinical event. Bacterial infection is thought to be a major cause of AD in patients; it is the inducer of systemic inflammation through the release of pathogen-associated molecular patterns (PAMPs), which has been confirmed as a trigger for developing acute on chronic liver failure (ACLF).3,4 ACLF is characterized by the failure of one or more organs, has high short-term mortality, and always occurs in the setting of an episode of AD.5 The survival date of AD patients drops to 2–4 years.6 Therefore, it is essential to develop a prognostic model to predict outcomes in AD patients.
Currently, many scoring models for liver cirrhosis are available, including the Child‒Pugh score, Model for End-Stage Liver Disease (MELD) and Chronic Liver Failure-Consortium AD score (CLIF-C AD).7–9 The CTP score is established according to albumin, prothrombin time, serum bilirubin, ascites and hepatic encephalopathy.7 The accuracy of the CTP score is influenced by subjective criteria such as ascites and HE.10 The MELD score was developed based on the following laboratory test results: international normalized ratio (INR), creatinine and bilirubin.8 However, the MELD score does not include inflammatory biomarkers such as white blood cells. The CLIF-C AD score is proposed to be capable of predicting prognosis in patients with decompensated cirrhosis without ACLF.9 A previous study confirmed that the CLIF-C AD score was not superior to other well-established prognostic scores in predicting mortality among AD patients.11 Therefore, the aim of our study was to establish a new prognostic model for AD patients.
Materials and Methods
Patients and Study Design
This study included a total of 703 acute decompensated cirrhosis patients at the Department of Gastroenterology, The First Affiliated Hospital of Nanchang University, between December 2018 and May 2021. Inclusion criteria included the following: (1) age ≥18; (2) diagnosed with cirrhosis (based on histology and/or compatible laboratory and radiologic findings); and (3) acute decompensated events, including gastroesophageal variceal hemorrhage, development of large ascites, hepatic encephalopathy (HE), hepatorenal syndrome (HRS), spontaneous bacterial peritonitis (SBP) or any combination of these. (4) developed a first episode of AD at the time of hospital admission or within 2 weeks before admission. Patients were excluded if they (1) had hepatocellular carcinoma; (2) had evidence of chronic renal disease or other severe chronic extrahepatic diseases; (3) had evidence of infection with human immunodeficiency virus; or (4) had a history of liver transplantation. A total of 703 AD patients were enrolled in the study and randomly assigned to the training set (n=528) or validation set (n=175). Informed consent for participation in this study was obtained from each patient or his or her legal surrogate. This study was approved by the Ethics Committee of The First Affiliated Hospital of Nanchang University.
Data Collection and Treatment
Clinical information, laboratory results, demographic data and acute decompensation events were recorded from medical records. We collected all laboratory results within 24 h after admission. The primary endpoint of this study was 6-month mortality. The CTP score was calculated based on prothrombin time (PT), ascites, albumin, serum bilirubin, and HE.7 The MELD score was computed according to the formula: MELD=11.2×ln[prothrombin time (international normalized ratio (INR))] + 9.6×ln [serum creatinine (Scr) (mg/dl)] +3.8×ln[total bilirubin (mg/dl)] + 6.43×(etiology: 0 if cholestatic or alcoholic, 1 otherwise).8 The CLIF-C AD score was calculated as follows: CLIF-C AD= 10×0.03×age (years) + 0.66×ln [serum creatinine (Scr) (mg/dl)] + 1.71×ln (INR) + 0.88×ln [WBC (109 cells/L)]-0.05×sodium (mmol/L) +8.9 For AD patients, standard medical therapies were used, including antiviral treatment, anti-infective therapy, endoscopic hemostatic therapy and other treatments to prevent complications.
Statistical Analysis
Statistical analysis was performed using SPSS 24.0 (SPSS Inc., Chicago, IL, USA) and R 4.2.0 (http://www.r-project.org/). Continuous data are expressed as the mean ± standard deviation, which was compared by using t-tests or the Mann‒Whitney test. The chi-squared test or Fisher’s exact test was used to analyze the differences in proportions of clinical variables. Independent prognostic indicators of mortality were identified through univariate and multivariate Cox regression analyses. The training set was applied to develop the new score according to the β coefficients from the multivariable Cox analysis. Patients were separated into low-risk and high-risk groups based on the median value of the new score.
Continuous variables are expressed as the mean (SD) and were compared using an unpaired, 2-tailed t-test or the Mann‒Whitney test. Categorical variables were compared using the chi-squared test or Fisher’s exact test. Univariate risk factors that reached p<0.2 were subjected to Cox regression analysis. The Kaplan–Meier survival curves of the high- and low-risk groups were plotted using the R packages “survival” and “survminer” to demonstrate the survival probability of the patients. The ROC curves were calculated using the “survminer”, “survival”, “timeROC”, and “pROC” packages in R software. The heatmap was computed by using the “pheatmap” package. A P value < 0.05 in a two-tailed test was considered statistically significant.
Results
Baseline Characteristics of Acute Decompensated Cirrhosis Patients
A total of 703 AD patients were included in this study, of whom 528 patients were randomly assigned to the training set, and 175 patients were assigned to the validation set (Figure 1). The clinical characteristics of AD patients in the training and validation sets are shown in Table 1. The median age was 54.5±11.8 years, with 77.1% of the patients being male. The main etiology of cirrhosis was hepatitis B virus infection in both the training (364/528, 68.9%) and validation sets (125/175, 71.4%). Variceal bleeding was the most common acute decompensation event in the training (348/528, 65.9%) and validation sets (103/175, 58.9%). There were no significant differences in clinical indicators between the two sets.
 |
Table 1 Clinical Characteristics of Cirrhosis Patients with AD |
 |
Figure 1 Study flow chart for the training and validation cohorts. |
Clinical Characteristics of the Nonsurviving and Surviving Patients
We compared the clinical characteristics between survivors and nonsurvivors in the training set. Comparative data showed that bilirubin, creatinine, international normalized ratio (INR), prothrombin time (PT), white blood cell count (WBC), albumin, alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), serum urea (BUN), sodium, CTP, MELD and CLIF-C AD were significantly different between survivors and nonsurvivors (all P values<0.05). No significant difference was found in the platelet count (P value>0.05). The clinical characteristics of the training set patients are presented in Table 2.
 |
Table 2 Comparing the Clinical Variables Between Non-Surviving and Surviving Patients in Training Set |
Construction of the New Score
Furthermore, we confirmed independent prognostic factors for AD patients. As shown in Table 3, in univariate Cox regression analysis, age, bilirubin, creatinine, INR, PT, WBC, albumin, ALT, AST, ALP and BUN were correlated with the mortality of AD patients. In multivariate Cox regression analysis, age, bilirubin, INR, WBC, ALT and BUN were associated with worse prognosis, and elevated albumin predicted a better survival rate. Then, the new score model was established based on multivariate Cox regression analysis. Finally, the formula was as follows: 0.022×Age + 0.003×TBil + 0.397×INR + 0.023×WBC- 0.07×Albumin + 0.001×ALT + 0.038×BUN.
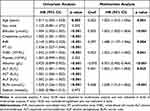 |
Table 3 Univariate and Multivariate Cox Regression Analyses of Factors Associated with Mortality in Training Set |
Predictive Performance of the New Score in the Training Set
In the training set, by using the median cutoff value (0.68) to divide the low- and high-risk AD patients, low-risk and high-risk groups were obtained (Figure 2a). Kaplan‒Meier survival plots were generated to compare the survival probability between the low- and high-risk groups (Figure 2b), and the patients in the high-risk group had a lower survival probability than those in the low-risk group (P<0.001). The area under the ROC curve (AUCROC) was calculated to compare the prognostic value between the new score and the other three common scores. The AUROC of the new score was 0.814 (95% CI: 0.778–0.847), which was significantly higher than that of the MELD, CTP and CLIF-C AD scores (0.777 (95% CI: 0.739–0.812); 0.764 (95% CI: 0.726–0.800) and 0.637 (95% CI: 0.594–0.678), respectively) (Table 4 and Figure 2c).
 |
Table 4 The Predictive Value Comparison of New Score and Other Score Systems in Training Set |
Internal Validation of the New Score
In the validation set, the low-risk and high-risk groups were divided according to the median cutoff value (0.68) (Figure 3a). The survival analysis indicated that the patients in the low-risk group had a higher survival probability than those in the high-risk group (P<0.001) (Figure 3b). The new score had the highest AUROC (0.837, 95% CI: 0.774–0.889), followed by the MELD score (0.805, 95% CI: 0.738–0.861), CTP score (0.763, 95% CI: 0.693–0.824) and CLIF-C AD score (0.694, 95% CI: 0.620–0.762) (Table 5 and Figure 3c).
 |
Table 5 The Predictive Value Comparison of New Score and Other Score Systems in Validation Cohort |
Relationship Between the New Score and the Three Scores
To further evaluate the correlation between the new score model and the three score models, a heatmap was generated in the training and validation sets. In the training set, the heatmap revealed that patients with high risk scores exhibited higher CTP, MELD and CLIF-C AD scores (Figure 4a). Additionally, the correlations between the risk score and the three scores were also calculated, and the results showed that the CTP, MELD and CLIF-C AD scores were elevated in the high-risk group (Figure 4b) (all P<0.001). Similar results were also confirmed in the validation set (Figure 5a and b).
Discussion
In the present study, a new score model was established to assess the individual long-term prognosis of AD patients. This new score model presented superior predictive performance relative to the current prognostic score models, including the CTP, MELD and CLIF-C AD scores.
In the training and validation sets, the leading etiology of AD patients was HBV, which is highly endemic in China.12 A total of 348 (65.9%) and 103 (58.9%) patients were admitted with variceal bleeding in the training and validation sets, respectively, and variceal hemorrhage is one of the most relevant causes of death in AD patients and clinically significant portal hypertension.13 According to the results of multivariate Cox regression analysis, we developed the new score model. This new score had better prognostic value than the CTP, MELD and CLIF-C AD scores; moreover, we adopted the internal validation cohort to confirm the prognostic performance of the new score model.
The CTP score is generally applied to evaluate the prognosis of patients with cirrhosis, and the 2 subjective indicators reduce the accuracy of mortality prediction.14 The MELD score was established to evaluate liver function and confirmed as an independent risk predictor for the prognosis of AD patients, but the calculation of the score was complicated and inconvenient for clinical practice.15 A previous study confirmed that the CLIF-C AD score had a lower prognostic value than the CTP or MELD score for HBV-AD patients.16 The new score model was developed based on age, bilirubin, INR, WBC, albumin, ALT and BUN, which had better prognostic value in both the training and validation sets. Numerous studies have revealed that older age is an important factor in predicting poor prognosis for cirrhosis patients.17,18 Bilirubin is an important blood index for assessing liver function and is also the primary element of the CTP and MELD scores. As an indicator of severe liver injury, INR was included in the MELD and CLIF-C AD scores. WBC count is an inflammatory biomarker, and systemic inflammation is related to the development of one or more organ failures in AD patients.19,20 Albumin was confirmed as a biomarker of malnutrition–inflammation syndrome, and decreased albumin had a negative impact on the prognosis of AD patients.21,22 ALT (alanine aminotransferase) is a significant enzyme in the liver, and a previous study confirmed that elevated ALT levels were associated with an increased risk of hepatic complications, which may influence the prognosis of cirrhosis patients.23 BUN was the surrogate biomarker for increased severity of renal or systemic illness, and a recent study showed that BUN was a predictive factor for poor prognosis in advanced liver diseases by using machine learning.24 The new score incorporated these indicators and exhibited better prognostic value in predicting the outcome for AD patients. Moreover, the excellent prognostic performance of the new score was confirmed in the validation set. The new score was significantly correlated with the CTP, MELD and CLIF-C AD scores. These results showed better prognostic value for predicting the outcome in AD patients.
Certainly, our study has some limitations. First, this is a single-center and retrospective study, which may lead to selection bias. Second, our findings may be limited in China, with cohorts of predominantly HBV-related cirrhosis patients. Third, our study lacks external validation, so a prospective, large sample size and multicenter study need to be designed in the future.
In conclusion, this new score model has better prognostic value than the CTP, MELD and CLIF-C AD scores in predicting long-term mortality for AD patients, which may facilitate risk stratification and clinical decision-making for AD patients.
Data Sharing Statement
The datasets used and/or analyzed in the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The study was performed according to the principles of the Declaration of Helsinki. The study was approved by the ethics committee of the First Affiliated Hospital of Nanchang University. Only subjects who signed the informed consent form were included in the data collection and interviews.
Acknowledgments
We would like to thank the National Natural Science Foundation of China (81660110; 81960120), the “Gan-Po Talent 555” Project of Jiangxi Province (GCZ (2012)-1), the Postgraduate Innovation Special Foundation of Jiangxi Province (YC2022-B052) and the Jiangxi Clinical Research Center for Gastroenterology (20201ZDG02007).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the National Natural Science Foundation of China (grant number: 81660110), the National Natural Science Foundation of China (grant number: 81960120), the “Gan-Po Talent 555” Project of Jiangxi Province (GCZ (2012)-1) and the Postgraduate Innovation Special Foundation of Jiangxi Province (YC2022-B052).
Disclosure
The authors declare that they have no competing interests.
References
1. Gines P, Krag A, Abraldes JG, et al. Liver cirrhosis. Lancet. 2021;398(10308):1359–1376. doi:10.1016/S0140-6736(21)01374-X
2. D’Amico G, Bernardi MAngeli P, Angeli P. Towards a new definition of decompensated cirrhosis. J Hepatol. 2022;76(1):202–207. doi:10.1016/j.jhep.2021.06.018
3. Arroyo V, Angeli P, Moreau R, et al. The systemic inflammation hypothesis: towards a new paradigm of acute decompensation and multiorgan failure in cirrhosis. J Hepatol. 2021;74(3):670–685. doi:10.1016/j.jhep.2020.11.048
4. Elsing C, Harenberg S, Stremmel W, et al. Serum levels of soluble Fas, nitric oxide and cytokines in acute decompensated cirrhotic patients. World J Gastroenterol. 2007;13(3):421–425. doi:10.3748/wjg.v13.i3.421
5. Weiss E, de la Pena-Ramirez C, Aguilar F, et al. Sympathetic nervous activation, mitochondrial dysfunction and outcome in acutely decompensated cirrhosis: the metabolomic prognostic models (CLIF-C MET). Gut. 2023:gutjnl-2022–328708. doi:10.1136/gutjnl-2022-328708
6. D’Amico G, Garcia-Tsao GPagliaro L, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44(1):217–231. doi:10.1016/j.jhep.2005.10.013
7. Pugh RN, Murray-Lyon IM, Dawson JL, et al. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60(8):646–649. doi:10.1002/bjs.1800600817
8. Kamath PS, Wiesner RH, Malinchoc M, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33(2):464–470. doi:10.1053/jhep.2001.22172
9. Jalan R, Pavesi M, Saliba F, et al. The CLIF consortium acute decompensation score (CLIF-C ADs) for prognosis of hospitalised cirrhotic patients without acute-on-chronic liver failure. J Hepatol. 2015;62(4):831–840. doi:10.1016/j.jhep.2014.11.012
10. Durand F, Valla D. Assessment of the prognosis of cirrhosis: child-Pugh versus MELD. J Hepatol. 2005;42(1):S100–S107. doi:10.1016/j.jhep.2004.11.015
11. Picon RV, Bertol FS, Tovo CV, et al. Chronic liver failure-consortium acute-on-chronic liver failure and acute decompensation scores predict mortality in Brazilian cirrhotic patients. World J Gastroenterol. 2017;23(28):5237–5245. doi:10.3748/wjg.v23.i28.5237
12. Ott JJ, Horn J, Krause G, et al. Time trends of chronic HBV infection over prior decades - A global analysis. J Hepatol. 2017;66(1):48–54. doi:10.1016/j.jhep.2016.08.013
13. Zanetto A, Shalaby S, Feltracco P, et al. Recent advances in the management of acute variceal hemorrhage. J Clin Med. 2021;10(17):3018. doi:10.3390/jcm10173818
14. Cholongitas E, Papatheodoridis GV, Vangeli M, et al. Systematic review: the model for end-stage liver disease-should it replace Child-Pugh’s classification for assessing prognosis in cirrhosis? Aliment Pharmacol Ther. 2005;22(11–12):1079–1089. doi:10.1111/j.1365-2036.2005.02691.x
15. Zheng YX, Zhong X, Li YJ, et al. Performance of scoring systems to predict mortality of patients with acute-on-chronic liver failure: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2017;32(10):1668–1678. doi:10.1111/jgh.13786
16. Gao F, Li X, Wan G, et al. Development and external validation of a prognostic nomogram for acute decompensation of chronic hepatitis B cirrhosis. BMC Gastroenterol. 2018;18(1):179. doi:10.1186/s12876-018-0911-y
17. Faber W, Stockmann M, Schirmer C, et al. Significant impact of patient age on outcome after liver resection for HCC in cirrhosis. Eur J Surg Oncol. 2014;40(2):208–213. doi:10.1016/j.ejso.2013.10.018
18. Kim IH, Kisseleva T, Brenner DA. Kisseleva TBrenner DA. Aging and liver disease. Curr Opin Gastroenterol. 2015;31(3):184–191. doi:10.1097/MOG.0000000000000176
19. Claria J, Stauber RE, Coenraad MJ, et al. Systemic inflammation in decompensated cirrhosis: characterization and role in acute-on-chronic liver failure. Hepatology. 2016;64(4):1249–1264. doi:10.1002/hep.28740
20. Kim JH, Kim SE, Song DS, et al. Platelet-to-white blood cell ratio is associated with adverse outcomes in cirrhotic patients with acute deterioration. J Clin Med. 2022;11(9):2463. doi:10.3390/jcm11092463
21. Akirov A, Masri-Iraqi H, Atamna A, et al. Low albumin levels are associated with mortality risk in hospitalized patients. Am J Med. 2017;130(12):1465.e11–1465.e19. doi:10.1016/j.amjmed.2017.07.020
22. Di Pascoli M, Fasolato S, Piano S, et al. Long-term administration of human albumin improves survival in patients with cirrhosis and refractory ascites. Liver Int. 2019;39(1):98–105. doi:10.1111/liv.13968
23. Wong GL, Wong VW, Choi PC, et al. Evaluation of alanine transaminase and hepatitis B virus DNA to predict liver cirrhosis in hepatitis B e antigen-negative chronic hepatitis B using transient elastography. Am J Gastroenterol. 2008;103(12):3071–3081. doi:10.1111/j.1572-0241.2008.02157.x
24. Yu CS, Chen YD, Chang SS, et al. Exploring and predicting mortality among patients with end-stage liver disease without cancer: a machine learning approach. Eur J Gastroenterol Hepatol. 2021;33(8):1117–1123. doi:10.1097/MEG.0000000000002169
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




