Back to Journals » Neuropsychiatric Disease and Treatment » Volume 15
Dementia-related neuropsychiatric symptoms: inequalities in pharmacological treatment and institutionalization
Authors Mar J , Arrospide A , Soto-Gordoa M , Iruin Á , Tainta M , Gabilondo A , Mar-Barrutia L, Calvo M, Mateos M, Ibarrondo O
Received 17 March 2019
Accepted for publication 24 June 2019
Published 17 July 2019 Volume 2019:15 Pages 2027—2034
DOI https://doi.org/10.2147/NDT.S209008
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Javier Mar,1–4 Arantzazu Arrospide,2–4 Myriam Soto-Gordoa,5 Álvaro Iruin,4,6 Mikel Tainta,7,8 Andrea Gabilondo,4,6 Lore Mar-Barrutia,9 Montserrat Calvo,10 Maider Mateos,10 Oliver Ibarrondo2,4
1Clinical Management Unit, OSI Alto Deba, Arrasate-Mondragón, España; 2AP-OSIs Gipuzkoa Research Unit, OSI Alto Deba, Arrasate-Mondragón, España; 3Economic Evaluation Department, Health Services Research on Chronic Patients Network (REDISSEC), Bilbao, Spain; 4Economic Evaluation Department, Biodonostia Health Research Institute, Donostia-San Sebastián, Spain; 5Departamento de Ingeniería de Organización, Mondragón Unibertsitatea, Arrasate-Mondragón, España; 6Psychiatry Service, Gipuzkoa Mental Health Network, Donostia-San Sebastián, España; 7Psychiatry Service, CITA Alzheimer Foundation, Donostia-San Sebastián, España; 8Neurology Service, OSI Goierri-Alto Urola, Zumárraga, España; 9Psychiatry Service, Hospital Bellvitge, Hospitalet de Llobregat, España; 10Health Department, Basque Government, Vitoria-Gasteiz, España
Background: Dementia-related neuropsychiatric symptoms (NPS) are the main determinant of family stress and institutionalization of patients. This study aimed to identify inequalities by gender and socioeconomic status in the management of NPS in patients diagnosed with dementia.
Methods: An observational study was carried out to study all the cases of dementia in the corporate database of the Basque Health Service (29,864 patients). The prescription of antipsychotics and antidepressants and admission to a nursing home were used to establish the presence of NPS. The socioeconomic status of individuals was classified by a deprivation index. Logistic regressions were used to identify drivers for drug prescriptions and institutionalization.
Results: NPS are poorly recorded in the clinical databases (12%). Neuropsychiatric symptoms were severe enough in two thirds of patients with dementia to be treated with psychoactive medication. Institutionalization showed an increase from those who did not receive medication to those who had been prescribed antidepressants (OR: 1.546), antipsychotics (OR: 2.075) or both (OR: 2.741). The resulting inequalities were the increased prescription of antidepressant drugs in women and more nursing-home admissions for women who were the least socioeconomically deprived and men who were the most deprived.
Conclusions: In large clinical databases, psychoactive drugs prescriptions can be useful to underscore the considerable burden of dementia-related NPS. Specific tools are needed to monitor social and health care programs targeted to dementia-related NPS from a population perspective. Programs aimed at reducing the family burden of care of dementia patients at home become the key elements in reducing inequalities in these patients’ care. Socioeconomic status is the most important driver of inequality, and gender inequality may simply be hidden within the social environment. Integrated programs boosting the continuity of care are an objective for which compliance could be measured according to the NPS coding in the electronic health record.
Keywords: neuropsychiatric symptoms, prevalence, dementia, antidepressant drugs, antipsychotic drugs, nursing home, inequalities, deprivation index
Introduction
Dementia is more than an aggregation of symptoms that causes serious deterioration of memory, cognition and social skills; it also harms mood and behavior, which is then expressed as distress in patients and caregivers.1 Dementia-related neuropsychiatric symptoms (NPS) are clinically important since they correlate strongly with the degree of functional damage.2,3 However, they are relevant mainly because they are independently associated with an increase in the economic burden and the loss of quality of life in patients and caregivers.4 As repeatedly reported, they are the main determinant of family giving up to home informal care and, consequently, of institutionalization of patients.1,3,5 It is estimated that up to 90% of all patients with dementia suffer from NPS during the course of their disease.3 Part of the negative impact of dementia on the quality of life of patients’ relatives is mediated by the mechanism of expressed emotion that is significantly aggravated by the presence of NPS.6
Although the clinical research is extensive,7,8 the epidemiology of NPS has not been thoroughly studied because of the lack of population registries. Also, the scarce information that is available has been dispersed because of separate collection by social and health services.1,9 The available prevalence data come from cross-sectional studies with small patient samples, and their results vary, depending on the origin of these investigations.1,4,10 For example, in samples recruiting subjects with dementia living in the community, NPS are generally less frequent and less severe than in patients living in long-term care centers.3,5 Given the difficulties in performing this type of study, epidemiological approximations have been carried out through the analysis of the prescription of antipsychotics.11,12 Although there are reports of validation of dementia identification algorithms in the clinical and administrative databases,9,13 no such study has explored the coding of dementia-related NPS in clinical databases.
Social determinants, such as social class, level of education and degree of deprivation based on the area of residence, play a key role in the health of individuals and populations.14 Their analysis is complex because of different ways to classify individuals socially, and the results depend on whether the impact is evaluated by measuring mortality, morbidity or utilization of health or social services.15 The appearance of dementia is also related to the unequal distribution of these determinants and to a socially determined increase in incidence that has shown higher rates in the groups with lower socioeconomic levels.16 Up to the present, no study has been available analyzing inequalities related to social factors in association with NPS in patients with dementia. However, it is possible that socioeconomic status and gender determine in some way the prevalence of NPS in dementia patients and how their care is socially managed.
This study aimed to identify inequalities by gender and socioeconomic status in the management of neuropsychiatric symptoms in patients diagnosed with dementia in the entire Basque Health Service by analyzing the use of psychoactive medication in association with the probability of admission to a nursing home.
Methods
An observational and cross-sectional study was carried out to examine inequalities related to NPS based on all the cases recorded in the corporate database of the Basque Health Service Oracle Business Intelligence (OBI). This database contains fully anonymous information updated daily from administrative and clinical records of primary care, hospitalization, emergencies and hospital outpatient consultations. This project was approved by the Ethics Committee of the Basque Country (PI2018087).
Subjects
The study sample included patients diagnosed with dementia in the OBI database and alive as of December 31, 2016. The search for the diagnosis of dementia was made by tracking validated criteria with a positive predictive value of 95.1% and a negative predictive value of 99.4% 9. The searches included dementia codes (Table S1 in Supplementary Material) in ICD9-CM and ICD 10 because from January 1, 2016, it has been the official ICD. The identification of dementia also included patients with a specific prescription for Alzheimer’s disease.9 As previously reported, our approach includes two thirds of the forecasted population prevalence and therefore we assume that the sample size is big enough to overcome the selection bias associate to the observational design.9
Variables
Dementia cases with NPS were sought in primary care, neurology and psychiatric consultations and hospitalizations (Table S1 in Supplementary Material). Estimating that the coding of these diagnoses was incomplete, we also looked within the clinical record for at least one pharmacological treatment of mood disorders (depression, anxiety and apathy) and psychotic disorders (aggression, irritability, restlessness, screaming, delusions and visual and auditory hallucinations). As private assurances in Spain cover diagnosis and surgical treatment but not drug treatment, prescription records also included patients treated in private practice. To this end, the prescription of antipsychotic medication was used as a surrogate indicator of the presence of psychotic-type NPS, and prescription of antidepressant medication was an indicator of depressive or mood-type NPS. The joint use of the two types of prescriptions allowed the classification of patients with dementia into four categories: without psychoactive treatment (no NPS), with depressive-type NPS, with psychotic-type NPS and with both types.
The following variables for all patients identified with dementia were recorded: age, sex, living in a nursing home, comorbidities (diabetes mellitus, hypertension, dyslipidemia, thyroid disease, Parkinson’s disease, stroke, cardiovascular disease, head trauma, depressive disorder), pharmacological treatment (antipsychotic medication, antidepressant medication) and deprivation index.
The deprivation index is an indicator of the individuals’ socioeconomic status that depends on their small area of residence. It is defined as a state of observable and demonstrable disadvantage in relation to the local community to which an individual belongs16,17 and has been adapted for the Spanish population.17 This composite index was calculated by the Research Service of the Health Department of the Basque Government, with the criteria of the Mortality and Health Inequalities in Spain (MEDEA) project based on simple indicators in the 2011 census.17 This index is divided into quintiles, with the first (Q1) being the least disadvantaged (rich) and the fifth (Q5) the most disadvantaged (poor). Given that social functions help to explain the gender differences observed in health and women systematically report poorer health than men,16 an integrated social and gender framework has been proposed to understand inequalities in health.14
Statistical analysis
The statistical analysis was performed in R (version 3.2.2) in several steps. First, a univariate analysis of the characteristics of the patients was carried out with Chi-square test for the categorical variables and the variance analysis (anova) for the comparison of means. The α statistical significance level was set up at 0.05. Subsequently, multivariate logistic regression models were constructed to analyze the probability of antipsychotic treatment, antidepressant treatment or both. Logistic regression was also used to analyze the probability of residence in a nursing home. All the logistic regression models were adjusted according to gender, deprivation index, type of psychoactive treatment and age and comorbidities. Finally, the interactions between the variables of gender and socioeconomic deprivation were included in the four logistic regression models. The variable that included five Q1–Q5 levels of the socioeconomic deprivation area index was re-grouped into two categories: higher (Q1-Q3) and lower (Q4-Q5) socioeconomic levels, to simplify the interpretation of the results. This allowed us to analyze the probability of living in a nursing home and receiving treatment with antipsychotics, antidepressants or both in four subgroups (men Q1–Q3, women Q1–Q3, men Q4–Q5 and women Q4–Q5).
Results
Of the 30,544 patients diagnosed with dementia and alive on December 31, 2016, 680 were ruled out due to lack of a deprivation index, so the final study sample study was 29,864. Table 1 shows their disaggregated characteristics by type of psychoactive treatment; 69.4% were women, and 27.6% lived in a nursing home. From the total sample, diabetes mellitus had been diagnosed in 23.9%, traumatic brain injury in 13.6% and stroke in 18.6%. Only one third (33.6%) had never received either antipsychotic or antidepressant treatment. The rest had received antidepressant treatment (34.0%), antipsychotic treatment (11.0%) or both (21.5%). The percentage of patients living in a nursing home was 19.8% in the untreated group, 26.8% in those treated with antidepressants, 31.7% in those treated with antipsychotics and 38.9% in those having been treated with both. Only 12% of patients had a record of the code for dementia-related NPS.
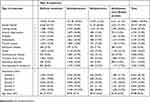 |
Table 1 Characteristics of patients with dementia disaggregated by psychoactive treatment type |
The probability of individuals being treated with antipsychotics and antidepressants decreased with age, and prescription of antidepressants was higher in women (Table 2). The deprivation index behaved inconsistently, since the probability of prescription of antidepressants was significantly lower in groups Q3, Q4 and Q5. The group with the highest socioeconomic status (Q1) was the most likely to receive antipsychotic treatment, although the differences among some groups were not statistically significant.
 |
Table 2 Logistic regressions analyzing the probability of patients being treated with antidepressants, antipsychotics or both |
When the probability of individuals being institutionalized was analyzed by logistic regression (Table 3), an increase developed from those who did not receive medication to those who had taken only antidepressants with an odds ratio (OR) of 1.556 to those who had taken only antipsychotics (OR, 2.075) to those who had taken both (OR, 2.741). Women had a higher likelihood of institutionalization, with a statistically significant OR of 1.286. Also, the patients having lower socioeconomic status in quintiles 4 and 5 were associated with a higher probability of living in a nursing home, with statistically significant OR of 1.131 and 1.309, respectively.
 |
Table 3 Logistic regression analyzing the probability that patients were living in a nursing home |
The subgroup analysis (Table 4) showed that women from the most advantaged group (Q1–Q3) lived more frequently in a nursing home (OR.1.27), while that characteristic appeared in men at a lower socioeconomic level (Q4–Q5) (OR, 1.12). Table 4 also shows that the only statistically significant inequality in the use of psychoactive drug was increased prescription of antidepressants in women within the highest socioeconomic status.
Discussion
The NPS were severe enough in two thirds of all patients living with dementia for them to have received at some time a prescription for psychoactive medication (antidepressants and/or antipsychotics). The inequalities that we found in prescription for psychoactive drugs and nursing-home admissions were related more to gender than to socioeconomic status. The strength of the study is its population approach that includes in the sample the entire population of cases of declared dementia. The Basque Health Service is a tax-funded Beveridge-type system and covers a population of 2.2 million inhabitants. The registered dementia cases included two thirds of the cases that would be expected according to the prevalence indicated by Ferri et al for the European countries, which indicates a high level of identification.9,18 However, the 12% registration of the NPS indicates a low explicit recognition of the problem, despite the fact that evidence shows that the prescription of antipsychotics and antidepressants is one of the biggest clinical challenges in dementia care.19 The figures in our analysis for prescription of antipsychotic (33%) and antidepressant (55%) treatment in dementia cases are similar to those described in other studies and correspond to a mixture of the population living in the community and in institutions.10 Olfson et al described higher figures in the American population more than 75 years of age with a diagnosis of dementia (37% for 75–79 years of age and 48% for 80–84 years).11 The finding that 27% of dementia patients are institutionalized is close to the 33% described in the United Kingdom.20
Although the use of antipsychotics did not show differences by gender, our results showed an inequality in antidepressant treatment, since these drugs were prescribed more often for women in all the statistical models. In studying differences in the NPS of male and female patients with Alzheimer’s disease in a clinical sample, Tao et al concluded that women displayed greater heterogeneity in the presentation of NPS, but no significant differences in the number.21 In our study, there were no consistent differences when patients were classified according to their socioeconomic status measured by the deprivation index. Although in the initial analysis with five quintiles, the patients in group Q1 (least deprived) received more prescriptions of antipsychotics, the results were not statistically significant in the analysis of subgroups.
According to the model without interactions, which focused on estimating the probability of institutionalization, women and the most deprived groups (Q4, Q5) had a higher risk of living in nursing home. However, when the interactions were incorporated into the analysis, only women with the most advantaged deprivation index (Q1-Q3) were more likely to live in institutions, whereas that characteristic appeared in men with the lowest socioeconomic status (Q4-Q5). The demand for institutionalization arises when the needs of patients and their caregivers are not solved due to the severity of symptoms and the lack of resources at home.22 Despite the development of the Dependency Law in Spain that has boosted social services, most of the care for patients with dementia is delivered by informal caregivers at home.23,24
The finding of more antidepressant prescriptions in women could indicate that they present with more NPS, which determines a more likely institutionalization.4,5 However, we found an inverse association between socioeconomic status and gender in the risk of institutionalization that may be due to the different social roles of women and men in relation to home care. Men at the highest socioeconomic levels (Q1–Q3) can stay at home because they have economic resources. Moreover, as they are more frequently married, their spouses often become the caregivers.25 When the woman is the dependent one, even with the financial resources available, the social environment is less prone to adapt to allow her to stay at home. Consequently, “rich” women may move to nursing homes because they do not receive adequate support at home. If the civil status of the cases had been available, we could have taken into account the percentage of widowed men. In the subgroup of most socioeconomically deprived men (Q4–Q5), their families may have fewer resources to maintain them adequately at home, and social services may have to take responsibility for their admittance to a nursing home.4 We do not have a clear explanation for the lower risk of institutionalization of women in groups Q4-Q5, when compared to men in the same groups.
Non-pharmacological treatments are the first choice for the treatment of dementia-related NPS in most of the clinical guidelines.12,26 Despite this, pharmacological treatment is the most used.11 In Spain, as in many other countries, environmental and behavioral treatments are not easily accessible. Making those programs available would help to reduce the number of prescriptions for antipsychotics, which has been recommended as a goal in dementia policy documents in the United Kingdom and United States.11,12 Different official reports have proposed limiting antipsychotic medication in patients with NPS, underlining the need to take into account, in all cases, the risk-benefit balance.20,26–28 After these warnings, the use of antipsychotics in the UK has decreased from 22.1% in 2005 to 11.4% in 2015, and from 2001 to 2014 the prescription of first-generation antipsychotics was greatly reduced.29 Conversely, the use of the new antipsychotics underwent few changes.12 In the region of Valencia (Spain) olanzapine and risperidone prescriptions were reduced after a safety warning was instituted.28 The goal of adequate use of psychoactive drugs based on the risk-benefit profile is to help patients and families cope with the stress caused by dementia-related NPS. The finding of a statistically significant rise in the risk of institutionalization highlights the meaning of the prescription of psychoactive drugs by confirming at the population level the determinant weight of NPS in family giving up to home informal care and nursing home admission that has already been displayed in clinical samples.1,10 The strong discordance between drug prescription and the percentage of patients formally diagnosed with NPS reinforces the need for a thorough understanding of these indicators. The existence of an increase in nursing-home admissions associated with the prescription of antidepressants and antipsychotics fits well with higher family distress related to psychotic or behavior disorders.30,31
The use of prescriptions as a surrogate indicator of the presence of NPS in patients with dementia is hampered by the existence of other indications and the inappropriate use of such prescriptions.11,12,26 Specific instruments such as the Neuropsychiatric Inventory (NPI) 7 or Behavioral Pathology in Alzheimer’s Disease (BEHAVE-AD)8 would be more valid to measure the presence of NPS, but their use in large clinical databases is not feasible for now. But, as the Organisation for Economic Co-operation and Development has remarked, a big data approach offers new tools to identify in clinical databases (broad data) patterns in cases of dementia requiring specific care.32 The term NPS is conceptually related to challenging behavior30 since these symptoms pose situations that cannot be managed in their environment without resorting to pharmacological treatment. Therefore, in the context of the natural history of dementia characterized by a progression in time, it seems reasonable to use psychoactive medication as a milestone that indicates that, beyond the physical functioning of the patient, NPS present a severe problem that requires intensive social care.33 Although NPS can affect 95% of patients with dementia at some point in the evolution of the disease, the number of those who require the prescription of antipsychotics and antidepressants at a given moment indicates the group that has exceeded the threshold in the level of distress that caregivers can endure.31 The percentage of pharmacologically treated patients seems to be a more useful indicator than the 12% of cases with a registered NPS diagnosis that we found.
Conclusions
The aim of our study was not to analyze the correct use of psychoactive medication, but to examine whether the analysis of its prescription in population-based databases can help lead to a clearer understanding of the burden of NPS in dementia patients. In a vicious cycle, this burden is underestimated because it is not recorded, and consequently, no efforts are made to measure it because the symptoms are not considered relevant. The scant attention observed in the population registries may also be a reflection of a fatalistic approach in which it is understood that NPS are unavoidable and have no effective treatment. To break this vicious cycle, specific tools are needed to monitor social and health care programs targeted to dementia-related NPS from a population perspective. Integrated programs boosting the continuity of care in the follow-up by social workers, primary care physicians and nurses, neurologists and psychiatrists are an objective for which compliance could be measured according to the coding in the electronic health record. Big data offers new tools to identify patterns associated with NPS in dementia patients.32
Access to nursing homes generally is going to be a problem for most deprived people. Moreover, the economic barrier for patients with NPS will expand for two reasons. First, neuropsychiatric patients require more resources, thereby increasing the cost to nursing homes. Second, aging populations foreshadow growing needs. Thus, programs aimed at reducing the family burden of care of dementia patients at home become the key elements in reducing inequalities in these patients’ care. Socioeconomic status is the most important driver of inequality, and gender inequality may simply be hidden within the social environment.
Ethics approval
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human subjects/patients were approved by the Clinical Research Ethics Committee of the Basque Country (PI2018087).
Acknowledgments
We would like to acknowledge the help of Sally Ebeling in improving the use of English in the manuscript. The study was funded by two grants from the Basque Foundation for Health Innovation and Research (Bioef) number BIO12/AL/005 and number BIOD17/ND/015.
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors have no conflicts of interest to declare in this work.
References
1. Backhouse T, Camino J, Mioshi E. What do we know about behavioral crises in dementia? A systematic review. J Alzheimers Dis. 2018;62:99–113. doi:10.3233/JAD-170679
2. Ballard C, Gauthier S, Corbett A, Brayne C, Aarsland D, Jones E. Alzheimer’s disease. Lancet. 2011;377:1019–1031. doi:10.1016/S0140-6736(10)61349-9
3. Cerejeira J, Lagarto L, Mukaetova-Ladinska EB. Behavioral and psychological symptoms of dementia. Front Neurol. 2012;3:73. doi:10.3389/fneur.2012.00073
4. Gilhooly KJ, Gilhooly MLM, Sullivan MP, et al. A meta-review of stress, coping and interventions in dementia and dementia caregiving. BMC Geriatr. 2016;16:106. doi:10.1186/s12877-016-0280-8
5. Katona C, Livingston G, Cooper C, Ames D, Brodaty H, Chiu E. International Psychogeriatric Association consensus statement on defining and measuring treatment benefits in dementia. Int Psychogeriatr. 2007;19:345–354. doi:10.1017/S1041610207005145
6. Weisman de Mamani A, Weintraub MJ, Maura J, Martinez de Andino A, Brown CA. Stigma, expressed emotion, and quality of life in caregivers of individuals with dementia. Fam Process. 2017;57:694–706. doi:10.1111/famp.12325
7. Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J. The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology. 1994;44:2308–2314. doi:10.1212/wnl.44.12.2308
8. Reisberg B, Borenstein J, Salob SP, Ferris SH, Franssen E, Georgotas A. Behavioral symptoms in Alzheimer’s disease: phenomenology and treatment. J Clin Psychiatry. 1987;48 Suppl:9–15.
9. Mar J, Arrospide A, Soto-Gordoa M, et al. Validity of a computerized population registry of dementia based on clinical databases. Neurologia. Epub 2018 May 8.
10. Zhao Q-F, Tan L, Wang H-F, et al. The prevalence of neuropsychiatric symptoms in Alzheimer’s disease: systematic review and meta-analysis. J Affect Disord. 2016;190:264–271. doi:10.1016/j.jad.2015.09.069
11. Olfson M, King M, Schoenbaum M. Antipsychotic treatment of adults in the United States. J Clin Psychiatry. 2015;76(10):1346–1353. doi:10.4088/JCP.15m09863
12. Stocks SJ, Kontopantelis E, Webb RT, Avery AJ, Burns A, Ashcroft DM. Antipsychotic prescribing to patients diagnosed with dementia without a diagnosis of psychosis in the context of national guidance and drug safety warnings: longitudinal study in UK general practice. Drug Saf. 2017;40:679–692. doi:10.1007/s40264-017-0538-x
13. Jaakkimainen RL, Bronskill SE, Tierney MC, et al. Identification of physician-diagnosed Alzheimer’s disease and related dementias in population-based administrative data: a validation study using family physicians’ electronic medical records. J Alzheimers Dis. 2016;54:337–349. doi:10.3233/JAD-160105
14. Stringhini S, Carmeli C, Jokela M, et al. Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1·7 million men and women. Lancet. 2017;389:1229–1237. doi:10.1016/S0140-6736(16)32380-7
15. Crombie IK, Irvine L, Elliott L, Wallace H. Closing the Health Inequalities Gap: An International Perspective. WHO Regional Office for Europe; 2005. Available from: http://www.euro.who.int/__data/assets/pdf_file/0005/124529/E87934.pdf.
16. Cadar D, Lassale C, Davies H, Llewellyn DJ, Batty GD, Steptoe A. Individual and area-based socioeconomic factors associated with dementia incidence in england: evidence from a 12-year follow-up in the english longitudinal study of ageing. JAMA Psychiatry. 2018;75:723–732. doi:10.1001/jamapsychiatry.2018.1012
17. Domínguez-Berjón MF, Borrell C, Cano-Serral G, et al. Constructing a deprivation index based on census data in large Spanish cities (the MEDEA project). Gac Sanit. 2008;22:179–187.
18. Ferri CP, Prince M, Brayne C, et al. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366:2112–2117. doi:10.1016/S0140-6736(05)67889-0
19. Kales HC, Maust DT. Good intentions, but what about unintended consequences? Drug Saf. 2017;40:647–649. doi:10.1007/s40264-017-0554-x
20. Department of Health. Living Well with Dementia: A National Dementia Strategy. London: Department of Health; 2009.
21. Tao Y, Peters ME, Drye LT, et al. Sex differences in the neuropsychiatric symptoms of patients with Alzheimer’s disease. Am J Alzheimers Dis Other Demen. 2018;33:450–457. doi:10.1177/1533317518783278
22. van Bilsen PM, Hamers JP, Don AA, Groot W, Spreeuwenberg C. The use of social services by community-dwelling older persons who are at risk of institutionalization: a survey. Eur J Ageing. 2010;7:101–109. doi:10.1007/s10433-010-0150-8
23. Soto-Gordoa M, Arrospide A, Zapiain A, Aiarza A, Abecia LC, Mar J. The cost of applying the dependency law to Alzheimer disease. Gac Sanit. 2014;28:389–392. doi:10.1016/j.gaceta.2014.04.012
24. Oliva J, Vilaplana C, Osuna R. The social value of informal care provided to elderly dependent people in Spain. Gac Sanit. 2011;25 Suppl 2:108–114. doi:10.1016/j.gaceta.2011.09.005
25. Peña-Longobardo LM, Oliva-Moreno J. Caregiver burden in Alzheimer’s disease patients in Spain. J Alzheimers Dis. 2015;43:1293–12302. doi:10.3233/JAD-141374
26. Agüera-Ortiz L, Moríñigo-Domínguez A, Olivera-Pueyo J, Pla-Vidal J, Azanza JR. Use of antipsychotics in late-life: document of the Spanish Society of Psychogeriatrics. Psicogeriatría. 2017;7(Supl 1):S1–S37.
27. Banerjee S. The Use of Antipsychotic Medication for People with Dementia: Time for Action. London, UK: Department of Health; 2009.
28. Sanfélix-Gimeno G, Cervera-Casino P, Peiró S, López-Valcarcel BG, Blázquez A, Barbera T. Effectiveness of safety warnings in atypical antipsychotic drugs: an interrupted time-series analysis in Spain. Drug Saf. 2009;32:1075–1087. doi:10.2165/11316520-000000000-00000
29. Donegan K, Fox N, Black N, Livingston G, Banerjee S, Burns A. Trends in diagnosis and treatment for people with dementia in the UK from 2005 to 2015: a longitudinal retrospective cohort study. Lancet Public Health. 2017;2:e149–e156. doi:10.1016/S2468-2667(17)30031-2
30. Trivedi DP, Braun A, Dickinson A, et al. Managing behavioural and psychological symptoms in community dwelling older people with dementia: 1. A systematic review of the effectiveness of interventions. Dementia (London). 2018:1471301218762851. doi:10.1177/1471301218762851
31. Krishnamoorthy A, Anderson D. Managing challenging behaviour in older adults with dementia. Prog Neurol Psychiatry. 2011;15:20–27. doi:10.1002/pnp.199
32. Anderson G, Oderkirk J, editors. Dementia Research and Care: Can Big Data Help? Paris: OECD Publishing; 2015.
33. Banaszak-Holl J, Fendrick AM, Foster NL, et al. Predicting nursing home admission: estimates from a 7-year follow-up of a nationally representative sample of older Americans. Alzheimer Dis Assoc Disord. 2004;18:83–89.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

