Back to Journals » Neuropsychiatric Disease and Treatment » Volume 15
Dementia care in the Danube Region. A multi-national expert survey
Authors Mehrabian S, Schwarzkopf L , Auer S, Holmerova I , Kramberger MG, Boban M, Stefanova E , Tudose C , Bachinskaya N, Kovács T , Koranda P , Kunchev T, Traykov L, Diehl-Schmid J , Milecka K, Kurz A
Received 5 January 2018
Accepted for publication 14 May 2019
Published 29 August 2019 Volume 2019:15 Pages 2503—2511
DOI https://doi.org/10.2147/NDT.S161615
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Shima Mehrabian,1 Larissa Schwarzkopf,2 Stefanie Auer,3 Iva Holmerova,4 Milica G Kramberger,5 Marina Boban,6 Elka Stefanova,7 Catalina Tudose,8 Natalia Bachinskaya,9 Tibor Kovács,10 Petr Koranda,11 Todor Kunchev,1 Latchezar Traykov,1 Janine Diehl-Schmid,12 Katrina Milecka,12 Alexander Kurz12
On behalf of the Danubian Network for Dementia Education Care (DANDEC) Consortium
1UH “Alexandrovska”, Department of Neurology, Medical University Sofia, Sofia, Bulgaria; 2Helmholtz-Centre Munich, Deutsches Forschungszentrum für Gesundheit und Umwelt (GmbH), Munich, Germany; 3Department for Clinical Neurosciences and Preventive Medicine, Danube University Krems, Krems, Austria; 4CELLO Faculty of Humanities, Charles University, Prague, the Czech Republic; 5University of Ljubljana, Department of Neurology, Ljubljana, Slovenia; 6University of Zagreb, Department of Cognitive Neurology, Zagreb, Croatia; 7School of Medicine, University of Belgrade, Neurology Clinic, Belgrade, Serbia; 8University of Medicine and Pharmacy Carol Davila, Department of Clinical Neurosciences, Bucharest, Romania; 9Acacdemy of Medical Sciences Kiev, Department of clinical physiology and pathology of the central nervous system, Kiev, the Ukraine; 10Department of Neurology, Semmelweis University, Budapest, Hungary; 11MEDIWARE corp., Prague, the Czech Republic; 12Department of Psychiatry and Psychotherapy, Klinikum rechts der Isar, Technische Universität München, Munich, Germany
Correspondence: Alexander Kurz
Centre for Cognitive Disorders at the Department of Psychiatry and Psychotherapy, Klinikum rechts der Isar; Technische Universität München, Ismaninger Strasse 22 Munich 81675, Germany
Tel +49 894 140 4285
Email [email protected]
Background: Dementia is a particularly severe societal challenge in several countries of the Danube Region due to higher-than-average increment in population longevity, disproportionate increase of the old-age dependency ratio, and selective outward migration of health care professionals. A survey was conducted among dementia experts to obtain a deeper understanding of the dementia care structures and services in this geographical area, and to identify the educational needs of health care professionals, and the availability of assistive technology.
Subjects and methods: A standardized questionnaire was sent out to 15 leading dementia experts/clinicians in 10 Danube Region countries inquiring about professional groups involved in dementia care, availability and reimbursement of services, inclusion of dementia in professional education and training, acceptability of Internet-based education, and availability of assistive technology. The authors are the survey respondents.
Results: The majority of individuals with dementia receive care in the community rather than in institutions. The roles of medical specialties are disparate. General practitioners usually identify dementia symptoms while specialists contribute most to clinical diagnosis and treatment. Health care professionals, particularly those who work closely with patients and carers, have limited access to dementia-specific education and training. The greatest need for dementia-specific education is seen for general practitioners and nurses. An Internet-based education and skill-building program is considered to be equivalent to traditional face-to-face but offer advantages in terms of convenience of access. Assistive technology is available in countries of the Danube Region but is significantly underused.
Conclusion: Dementia care in the Danube Region can be improved by an educational and skill-building program for health care professionals who work in the frontline of dementia care. Such a program should also attempt to enhance interdisciplinary and intersectorial collaboration, to intensify the interaction between primary care and specialists, and to promote the implementation of assistive technology.
Keywords: dementia, Danube Region, expert survey, dementia care structures, education, assistive technology
Introduction
The Danube Region is a functional area defined by its river basin. It extends over 14 states, among them 9 EU-member states (Germany, Austria, the Czech Republic, Slovakia, Hungary, Slovenia, Croatia, Bulgaria, and Romania) and 5 countries which are not presently EU-members (Serbia, Montenegro, Bosnia and Herzegovina, the Ukraine, and Moldova). The Danube Region has a total population of 150 million. In socio-economic regard, the region shows disparity since it includes not only some of the most affluent but also some of the poorest regions in the European Union.1 The prevalence of dementia among people aged 60 years and older is not uniform across the area. Rates of about 5% have been reported in Slovakia and Romania, whereas prevalence is as high as 7% in Austria, Germany, and Bulgaria.2–5 An even higher prevalence of dementia (10%) has been found in the Ukraine, but the validity of this data is questionable.6 Taken together, at least 3 million older adults are affected with dementia in the countries of the Danube Region.7,8 (Table 1).
 |
Table 1 Population size and numbers of people with dementia in the Danube Region |
Due to increasing life expectancy, the number of people affected with dementia is predicted to rise by 50% from 2015 to 2030 in eastern and southern Europe,9 and the dependency ratio (the ratio of people aged 65 or above relative to the working-age population) is expected to increase.10 An additional challenge in the Danube Region is the migration of health workers, predominantly Eastern part („“care drain”)11 and has resulted in a lack of qualified health personnel and reduced family support in the sending countries.12 The improvement and sustainability of dementia care and access to dementia-related knowledge have to be placed high on public and political agendas in the Danube Region. Here, we report the results of a multi-national survey which was carried out by the DANDEC consortium (for Details see Subjects and methods) in order to obtain a deeper understanding of dementia care and dementia-specific education in the Danube Region.
Subjects and methods
In 2013, a consortium of 10 academic centers, 2 patient and carer organizations, and 2 enterprises from 10 countries in the Danube Region formed the Danubian Network for Dementia Education and Care (DANDEC). The DANDEC project was supported by the German Ministry for Education and Research with grant number 01DS13011. The partners are active in dementia research, patient and carer advocacy, medical engineering, and software development. The aim of the group is to contribute to the improvement of dementia care in the Danube Region by providing a web-based education and skill-building program for health care professionals. This aim is consistent with national European action plans for dementia.13
Data collection
The survey was conducted using a standardized questionnaire which was completed by 15 leading experts/clinicians with research activities and outstanding expertise in dementia care in 10 countries of the Danube Region (Austria, Bulgaria, Croatia, the Czech Republic, Germany, Romania, Serbia, Slovenia, Hungary, and the Ukraine) from August 2014 to September 2014. The authors are the survey respondents. All these clinicians/experts are medical doctors or neuropsychologists with specialty in neurology, psychiatry, and clinical psychology. Most of the participants are National Dementia experts and members of European Alzheimer’s Disease Consortium from where they have been selected and contacted. The questionnaire was designed by the experts from Germany and Bulgaria. All authors approved the final version of the questionnaire. Since terminology of health care settings and services varies across countries, definitions were provided.
The clinicians/experts responded to the questionnaire according to their perceptions/claims and at the same time collected information from the main national stakeholders and national research studies.
In its first part, the questionnaire inquired about existing infrastructures of dementia care. It considered 1) care setting (home care vs institutional care), 2) integration of different medical specialties in dementia management, 3) availability of services for people with dementia and their carers, 4) corresponding reimbursement mechanisms, 5) relevance of dementia as a part of vocational education and training, 6) access to dementia-specific postgraduate professional education, and 7) availability and financing of assistive technology.
Information on those infra-structural framework conditions were stratified by country to highlight the heterogeneity of dementia care in the Danube Region.
In the second part, the questionnaire assessed expert opinion on professional groups considered most important for dementia care; professional groups most in need of dementia-specific education and training, and acceptability of an Internet-based educational program. These ratings were pooled across countries by calculating the mean (±SD) of available responses. Items and scoring of the questionnaire are shown in Table 2.
 |
Table 2 Items and scoring of the questionnaire |
Results
Part I
Home care and institutional care
The majority of people with dementia are being looked after in their own homes and not in institutions. However, the share of home care and institutional care varies across countries. The proportion of patients receiving care in their own homes is lowest in Germany (~60%) and highest in Bulgaria (>90%). On average about 80% of the people with dementia are cared for at home.
Contribution of medical specialties to the management of dementia
In all countries, general practitioners (GPs) are the entry point to the medical management of dementia. Their role is to identify older adults with cognitive and functional decline and refer them to specialists. Only in Germany, the medical care of people with dementia is largely in the hands of GPs. In all other countries, GPs play a minor role in dementia diagnosis (Figure 1) and are even less involved in dementia treatment. In all countries, neurologists and psychiatrists play an essential role in dementia diagnosis and treatment with different involvement rates (Figures 1 and 2). Geriatricians are not available as a medical specialty in Austria, Bulgaria, Serbia, Hungary, and Slovenia.
 |
Figure 1 Contribution of medical specialties to dementia diagnosis. |
 |
Figure 2 Contribution of medical specialties to dementia treatment. |
Availability of services for people with dementia and their family carers
Nursing home care and caregiver counseling and support are available in all countries. Day-care facilities and respite care are lacking in Romania, Serbia, and the Ukraine. Respite care is available only in Austria, the Czech Republic, and Germany. Assistance with activities of daily living, eg, by home helpers is not provided in Romania. Other services such as meals on wheels are not available in Romania and Serbia (Figure 3). In almost all countries, there is a considerable gradient regarding the availability of services from urban to rural areas which were defined as geographic areas that are located outside towns and cities.
 |
Figure 3 Availability of services for people with dementia and family carers. |
Financing of dementia-related service utilization
Visits to GPs and medical specialists are free in all countries. Patients are required to make co-payments for neuropsychological evaluations in Bulgaria, Romania, and the Ukraine. Different co-payment systems for in-patient hospital treatment are due in Germany, Austria, Croatia, and the Ukraine. In most countries, patients are required to contribute to the cost of medications and other medical treatments. Exceptions are Romania and Slovenia, where antidementia drugs are available for free. Medical treatment is paid completely out of pocket in the Ukraine. Occupational therapy for people with dementia is not available in Bulgaria, the Czech Republic, Romania, and Serbia. It is free in Croatia, but different patient co-payments are due in Germany, Austria, Slovenia, and the Ukraine. Non-pharmacological interventions such as cognitive training and rehabilitation are free in most countries, but part-payment is required in Austria, Slovenia, Hungary, and the Ukraine, and full payment is required in Bulgaria.
Nursing home care is completely free for people with dementia and their families in Serbia but requires different co-payments in all other countries. The persons with dementia and their carers need to make a financial contribution to day care in Austria, Croatia, the Czech Republic, Hungary, and Slovenia. In Bulgaria, day care needs to be paid completely out of pocket and is only free in Germany.
Dementia in the education for health care and allied professionals
Dementia is part of the education curriculum for specialist physicians (neurologists, psychiatrists, geriatricians) in all countries. However, dementia is not included in education and training for GPs in Austria, Romania, and Slovenia. Whereas dementia is part of the training for nurses in all countries with the exception of Austria, social workers do not learn about dementia in Austria, the Czech Republic, Croatia, and the Ukraine. Dementia is not included in the education of psychologists in Romania.
There is also a lack of dementia-specific education for occupational therapists in Austria and Romania (Figure 4).
 |
Figure 4 Dementia as a topic of education for health care and allied professionals. |
Postgraduate professional education includes dementia for all health care professionals in Austria, the Czech Republic, and Germany. In Slovenia, dementia-specific postgraduate education is only available for GPs, whereas in Romania, it is only provided for medical specialists. In Bulgaria, social workers and allied professionals have no access to this kind of education. Non-medical health care professionals cannot engage in postgraduate dementia-specific training in Croatia, Romania, Serbia, and the Ukraine.
Availability of assistive technology
Technology-based assistive devices are deemed useful in dementia care in most countries of the Danube Region, with sensors (eg, smoke, fire, gas, water) and communication solutions (eg, senior mobile phone, senior phones being fixed lines), are used most frequently, while prompts and reminders (eg, for keys and medication) are less used. Although in most countries people with dementia and their carers have access to a broad variety of devices, utilization rates are generally very low.
Part II
Need for dementia-specific education and training
Across countries, the greatest need for post-graduate dementia-specific education and training was seen for GPs, nurses, allied professionals, social workers, and occupational therapists, ie, for those who are involved in the front-line work with people with dementia and their family members. A lesser need was seen for specialist physicians and psychologists.
Usefulness of an Internet-based educational program
The groups of health care professionals who work in the frontline of dementia care, ie, nurses, social workers, occupational therapists, GPs, and allied professionals, are also those for whom a web-based educational program on dementia is considered to be most beneficial. This educational format is seen less useful for specialist physicians and psychologists (Figure 5).
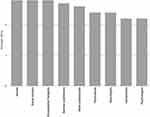 |
Figure 5 Usefulness of a web-based educational program. |
Discussion
The prevalence rates of dementia in the countries of the Danube Region are probably similar to those in western Europe.14 Differences across countries, with some showing prevalence rates below the European average7 of 7% are likely due to methodological difficulty and heterogeneity as the identified studies were characterized by an immense diversity with a considerable degree of clinical and methodological variations.
The Danube Region has higher-than-average increment in population longevity, disproportionate increase of the old-age dependency ratio,10 and selective outward migration of health care professionals.11 For these reasons, dementia is a particularly severe societal challenge in the Danube Region, and appropriate strategies need to be developed and implemented to tackle it.
In Europe, the majority of people with dementia are being cared for in their homes by family members.15 The share of community care is particularly large in some countries of the Danube Region. This may be due to cultural traditions which consider within-family care as a kind of social duty of the younger generation, but also to lack of appropriate long-term care facilities and limited affordability of nursing homes. Hence, strengthening community care and supporting family carers is a logical priority in improving the management of dementia in this geographical area.
According to our survey, there is a discrepancy in most countries of the Danube Region between the key importance that is assigned to general physicians (GPs) for the identification of dementia and as entry points to dementia care and the minor contribution which this group of physicians makes to the diagnosis and management of dementia. We also found that dementia is not included in the education of GPs in several countries. It is known that the management of dementia in primary care is a challenge due to inadequate knowledge, inadequate skills set, fear of making a wrong diagnosis, and lack of coordination between physicians and community services, among other reasons.16
Our survey also showed that nurses, social workers, occupational therapists, and allied health workers are important professional groups involved in the management of dementia. However, dementia is often not included in their regular education curriculum and they have limited access to postgraduate dementia-specific education. Other studies have also found that health care professionals who work closely with people with dementia and their family carers have limited access to specialized education.17
Therefore, we strongly believe that it is important to develop and evaluate educational programs that enhance the knowledge and skills of the professional groups who are active in the frontline of dementia care including educational programs for GPs. Such programs might also increase the collaboration between different groups of health care professionals.18 This has been shown to improve the quality of dementia care.19
Web-based learning has been shown to be an effective and economical format of postgraduate training among health care professionals.20 It may be particularly useful in countries of the Danube Region which are culturally, economically, and geographically highly diverse. Also, such innovative learning formats are particularly needed in rural areas where other forms of postgraduate professional education are difficult to access. The survey demonstrates that an Internet-based educational program is viewed as useful for all health care professionals. Additional face-to-face education and training may be appropriate for health care professionals involved in the frontline of dementia care.
Web-based information and education programs for health care professionals have been found to be as effective as face-to-face interventions in improving knowledge and skills, and can overcome geographical and mobility related barriers.21–23 Assistive technology, defined as any device that supports a person in retaining or improving their independence, safety, security, and dignity, can take many forms. These include safety alarms, monitoring of vital signs, fall detectors, flood sensors, and automated shut-offs for household appliances. For people with mild to moderate dementia, reminders and prompts, communication devices, and person tracking systems may particularly useful.24,25 The use of assistive technology devices might also be a part of such educational efforts, including ethical and data protection aspects. A literature review described frequent ethical dilemmas of which 2 are notable. The first is about privacy and respect for autonomy versus safety and minimizing risks. The more safety a person with dementia wishes to have, the more it may be necessary for them (or others on their behalf) to accept some loss of privacy or autonomy and with various possible negative consequences (eg, safety at the expense of reduced quality of life, some risk but possibility to delay entry into residential care, deterioration of carer’s quality of life or health). The second ethical dilemma is about obtaining informed consent from persons with dementia due to possible difficulties understanding complex technology and loss of awareness over time of the presence or purpose of assistive technology, or that data are being collected on them. The characteristics of home telecare should be made clear so that users have a thorough understanding of the limitations as well as the capabilities involved in this technology. Moreover, it is necessary to develop specific guidelines for the delivery of these services to the cognitively impaired elderly population.26,27
Non-pharmacological interventions such as cognitive training, behavioral management, or occupational therapy are considered an essential part of the management of dementia be European guidelines.28,29 However, the survey shows that access to these forms of treatment is limited in several countries of the Danube region. Another important gap in dementia care in the Danube Region that was identified by the survey is the lack of day care and respite care facilities. These services are important to support family carers and enhance their resilience.30 Given this shortage, education of professionals on which interventions and services are available and information about their indication and effectiveness are even more important for the improvement of dementia care. This could also increase the awareness of people with dementia and their carers for already available health and social services and how to access them.
Conclusion
In conclusion, we suggest that dementia care in the Danube Region can be improved by an educational and skill-building program for health care professionals who work in the frontline of dementia care. Such a program should also attempt to enhance interdisciplinary and intersectorial collaboration, to intensify the interaction between primary care and specialists, and to promote the implementation of assistive technology. Additionally, due to limited services in Danube region, it is essential to develop national plans for funding services for people with dementia and their careers.
Acknowledgments
The DANDEC project was supported by the German Ministry for Education and Research, grant number 01DS13011.
Disclosure
The authors report that they are the survey respondents that this paper is based on. The authors report no other conflicts of interest in this work.
References
1. European-Commission. European Union Strategy for Danube Region. Brussels: European Commission; 2010.
2. Rechel B, Grundy E, Robine JM, et al. Ageing in the European Union. Lancet. 2013;381(9874):1312–1322. doi:10.1016/S0140-6736(12)62087-X
3. Dimitrov I, Tzourio C, Milanov I, Deleva N, Traykov L. Prevalence of dementia and mild cognitive impairment in a Bulgarian urban population. Am J Alzheimers Dis Other Demen. 2012;27(2):131–135. doi:10.1177/1533317512442371
4. Stefanova E, Pekmezovic T, Nalic D, et al. The diagnosis of dementia is unspecified - report of a pilot survey of dementia in Belgrade. Gerontology. 2004;50(4):260–261. doi:10.1159/000078357
5. OECD. Health at a Glance: Europe 2012. OECD Publishing; 2012. doi:10.1787/9789264183896-en
6. Bezrukov VV, Polukhov AM, Bachinskaya NY, et al. Dementia prevalence in Kiev aging population based on screening investigation, 2001-2002. Acta Psychiatrica Pschologica Psychotherapeutica Et Etholologica Tavrica. 2004;8:47–52.
7. Alzheimer-Europe. The Prevalence of Dementia in Europe. Country Comparisons. Luxembourg: Alzheimer Europe; 2014.
8. Hughes L. Lessons learned: alzheime’s disease clinical trials in Eastern Europe. In: Bairu M, Weiner M, editors. Global Clinical Trials for Alzheimer’s Disease. San Diago, London, Waltham: Elsevier; 2014:263–275.
9. Wimo A, Jönsson L, Gustavsson A. Cost of Illness and Burden of Dementia - the Base Option. Luxembourg: A. Europe; 2009.
10. European-Commission. The 2015 Ageing Report. Economic and Budgetary Projections for the 28 EU Member States (2013-2060). Brussels: European Commission; 2015.
11. Gal Z, Lux G, Illes U. Danube Region - Analysis and Long-Term Development Trends of the Macro-Region. Vol. 90. Pécs: Insitute for Regional Studies, Research Centre for Economic and Regional Studies, Hungarian Academy of Sciences; 2013.
12. Siyam A, Dal-Poz MR. Migration of Health Workers: Tbe WHO Code of Practice and the Global Economic Crisis. Geneva: World Health Organization; 2014.
13. Alzheimer-Europe. National Dementia Strategies. Luxembourg: Alzheimer Europe; 2016.
14. Kiejna A, Frydecka D, Adamowski T, et al. Epidemiological studies of cognitive impairment and dementia across Eastern and Middle European countries (Epidemiology of Dementia in Eastern and Middle European Countries). Int J Geriatr Psychiatry. 2010;26(2):111–117. doi:10.1002/gps.2511
15. Alzheimer-Europe. Who Cares? the State of Dementia Care in Europe. Luxembourg: Alzheimer Europe; 2006.
16. Parmar J, Dobbs B, McKay R, et al. Diagnosis and management of dementia in primary care. Explorative study. Can Fam Physician. 2014;60:457–465.
17. Bryans M, Keady J, Turner S, Wilcock J, Downs M, Iliffe S. An exploratory survey into primary care nurses and dementia care. Br J Nurs. 2003;12(17):1029–1037. doi:10.12968/bjon.2003.12.17.11723
18. Valentijn PP, Schepman SM, Opheij W, Bruijnzeels MA. Understanding integrated care: a comprehensive conceptual framework based on the integrative functions of primary care. Int J Integr Care. 2013;13:e010. doi:10.5334/ijic.886
19. Callahan CM, Boustani MA, Unverzagt FW, et al. Effectiveness of collaborative care for older adults with Alzheimer’s disease in primary care. A randomized controlled trial. Jama. 2006;295(18):2148–2157. doi:10.1001/jama.295.18.2148
20. Cobb SC. Internet continuing education for health care professionals: an integrative review. J Contin Educ Health Prof. 2004;24(3):171–180. doi:10.1002/chp.1340240308
21. Wutoh R, Boren SA, Balas EA. eLearning: a review of Internet-based continuing medical education. J Contin Edc Health Prof. 2004;24(1):20–30. doi:10.1002/chp.1340240105
22. Ruiz JG, Mintzer KJ, Leipzig RM. The impact of E-learning in medical education. Acad Med. 2006;81(3):207–212.
23. Hobday JV, Savik S, Smith S, Gaugler JE. Feasibility of internet training for care staff of residents with dementia: the CARES program. J Gerontol Nurs. 2010;36(4):13–21. doi:10.3928/00989134-20100302-01
24. Bharucha AJ, Anand V, Forlizzi J, et al. Intelligent assistive techology applications to dementia care: current capabilities, limitations and future challenges. Am J Geriatr Psychiatry. 2009;17(2):88–104. doi:10.1097/JGP.0b013e318187dde5
25. Bonner A, Idris T. Assistive technology as a means of supporting people with dementia: a review. In: Porteus J, editor. London: Housing Learning & Improvement Network; 2012;1–17. doi:10.1094/PDIS-11-11-0999-PDN
26. Meiland F, Innes A, Mountain G, et al. Technologies to support community-dwelling persons with dementia: a position paper on issues regarding development, usability, effectiveness and cost-effectiveness, deployment, and ethics. JMIR Rehabil Assist Technol. 2017;4(1):e1. doi:10.2196/rehab.6376
27. Mehrabian S, Extra J, Wu YH, Pino M, Traykov L, Rigaud A-S. The perceptions of cognitively impaired patients and their caregivers of a home telecare system. Med Devices (Auckl). 2014;8:21–29. doi:10.2147/MDER.S70520
28. Hort J, O’Brien JT, Gainotti G, et al. EFNS guidelines for the diagnosis and management of Alzheimer’s disease. Eur J Neurol. 2010;17(10):1236–1248. doi:10.1111/j.1468-1331.2010.03040.x
29. Korczak D, Habermann C, Braz S. The effectiveness of occupational therapy for persons with moderate and severe dementia. GMS Health Technol Assess. 2013;9:1–7.
30. Donnellan WJ, Bennett KM, Soulsby LK. What are the factors that facilitate of hinder resilience in older spousal dementia carers? A qualitative study. Aging Ment Health. 2015;19(10):932–939. doi:10.1080/13607863.2014.977771
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
