Back to Journals » Patient Preference and Adherence » Volume 8
Demand and characteristics of a psychiatric 24-hour emergency service performed by mandatory rotation of licensed psychiatrists in Swiss primary care
Authors Chmiel C, Rosemann T , Senn O
Received 4 September 2013
Accepted for publication 6 February 2014
Published 27 March 2014 Volume 2014:8 Pages 383—390
DOI https://doi.org/10.2147/PPA.S53950
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Corinne Chmiel, Thomas Rosemann, Oliver Senn
Institute of General Practice and Health Services Research, University of Zurich, Raemistrasse, Zurich, Switzerland
Background: To investigate characteristics of and satisfaction with psychiatric 24-hour emergency primary care performed by mandatory rotation of licensed psychiatrists as a viable baseline for possible reorganizational measures.
Methods: This was a questionnaire-based cross-sectional study (November 2010–April 2011). The number of patient–psychiatrist encounters, modes of contact, and patient and psychiatrist characteristics were assessed. Diagnoses were coded with ICD-10 (International Classification of Diseases, version 10).
Results: From 167 duty episodes, 74 (44%) were recorded. Of the psychiatrists (n44), 52% were female, and mean age (standard deviation) was 49.9 (5.2) years. The median number of encounters per episode was 4 (interquartile range 0–8), mainly in the evenings. Demand for “face-to-face” (direct) patient visits was significantly more common (64.0%) than practice (1.3%) or telephone consultations (34.7%). In 83.8%, psychiatrists judged the encounter as adequate at the patient’s location. A total of 43 different diagnoses were recorded: mainly schizophrenic disorders (23.9%), suicidal behavior (15.2%), and acute stress reactions (10.3%). Psychiatrists felt burdened by services (62.5%): in 39.2%, they felt threatened; and in 6.8%, violence occurred. In 32.4%, bills were not paid for. If services were optional, 45.2% would participate.
Conclusion: Our findings indicate justified demand for direct mobile patient visits, suggesting that emergency care should be multifaceted, and sole provision of psychiatric care at stationed emergency facilities may not always be appropriate. Reorganization of 24-hour emergency services should carefully evaluate patient and provider’s needs before changing established structures.
Keywords: primary health care, after-hours care, emergencies, satisfaction, psychiatry
Background
Psychiatric emergency services in Western countries are mainly provided by three different kinds of settings: 1) fixed settings, ie, emergency rooms of general hospitals, psychiatric institutions, and outpatient clinics; 2) mobile psychiatric settings, ie, psychiatric services integrated into general practitioners’ 24-hour emergency services and specialized mobile psychiatric emergency care teams; and 3) mobile general practitioners setting, ie, emergency services provided by general practitioners, with no specialized psychiatric service.1 In Zurich, Switzerland, in addition to hospital-based emergency psychiatric care, 24-hour emergency psychiatric care is currently provided by a rota system of licensed psychiatrists, an organizational model which has rarely been described in the literature and which is unique to Switzerland.2
In Switzerland, as in numerous other countries, many efforts are currently undertaken to reorganize primary care 24-hour emergency services with the aim of reducing the burden of overcrowded emergency departments.3–7 Possible solutions, which have partly also been established in the greater area of Zurich, are privately run community-based emergency practices, primary care centers integrated into hospitals’ emergency departments,8 or telephone triage and advice services.9 The ongoing changes in general emergency services, combined with the growing dissatisfaction of psychiatrists with the current emergency service (services are considered as stressful, dangerous, and inadequately paid), resulting in increasing numbers of psychiatrists not willing to perform emergency services, has urged the Zürcher Gesellschaft für Psychiatrie und Psychotherapie (federation of psychiatrists) to rethink the organization of the 24-hour emergency psychiatric service. Since no systematic data on the existing emergency psychiatric service exists, it is unclear whether these new models of general emergency services suit the needs of specialized emergency psychiatric care.
The aim of this study was to provide an overview on the current 24-hour emergency psychiatric service in Zurich performed by mandatory rotation of licensed psychiatrists as a viable baseline for possible reorganizational measures, taking patient demands as well as needs of the psychiatrists into consideration.
Methods
Setting
In Switzerland, patients have mandatory health insurance, which provides unlimited access to the health care system, including specialist care and emergency care at the hospital. Depending on the insurance model chosen, deductibles vary, but access to emergency care is always granted. In the city of Zurich (population 400,000), the primary care 24-hour emergency service for psychiatrists as well as general practitioners is currently organized by an Emergency Medical Service Telephone (EMST) switchboard as a unit of the general emergency medical service.10 The features of this service can be summarized as follows:
- Mandatory rota system provided by psychiatrists from private practice
- Access via single regional telephone number
- EMST switchboard guides patient to psychiatrist on duty
- Access 24/7
- Telephone consultations, home visits, and practice consultations are provided
- Psychiatrist on duty is responsible for the entire city (population approximately 400,000; area approximately 91.88 km2)
- Shifts lasting for 24 hours, from 12 am to 12 am.
The reasons for choosing this psychiatric emergency service instead of the patient’s own psychiatrist vary: either the patient does not have a psychiatrist or does not want to consult his own psychiatrist, the psychiatrist might be absent or occupied, the emergency might occur outside of practice opening hours, or the contact with the service is needed by a bystander who does not know whether the patient has already been under psychiatric care.
Psychiatrists in Zurich as well as general practitioners are obliged by contract to participate in primary care emergency services. Within this contract, reasons for reducing the amount of services needed or reasons for complete exemption from the services are defined, such as frail physical health, pregnancy, and attendance of small children. The minimal annual mandatory amount of services per psychiatrist is currently five in the case of 100% clinical occupation. This number can vary according to fluctuations in the number of registered psychiatrists in the city.
Our study covered all psychiatrist encounters connected via the EMST switchboard during a 24-hour service period.
Subjects and data collection
The data on the 24-hour emergency service were collected between November 1, 2010 and April 15, 2011. Questionnaires were sent by the EMST switchboard via email to all on-duty psychiatrists. Before the beginning of a duty period, the EMST switchboard called the psychiatrist on duty to ensure that he or she had received the questionnaire and was aware of the study. If data were not provided by 2 days after the duty period, a further telephone reminder was conducted by the EMST switchboard.
Variables measured
The survey assessed demographics, professional experience, and satisfaction with the current emergency system of the psychiatrists on duty. To investigate the demand for and characteristics of the 24-hour emergency care, the psychiatrists documented number and mode of encounters (home, practice, or telephone contact) during the duty period. Detailed patient characteristics were documented for the first, second, and third and the last patient encounter.
Medical diagnoses according to the International Classification of Diseases, version 10 (ICD-10), whenever possible, were either coded directly by the psychiatrist on duty or were provided as diagnoses in wording subsequently translated into ICD-10 code by a research assistant of the Institute of General Practice and Health Services Research. All codings were double-checked by two consulting psychiatrists. Therapeutic procedures and the mode of care subsequent to the emergency encounter (eg, final treatment by psychiatrist defined as outpatient care or transferal to hospital) were recorded. The participants were also offered questionnaire space for free reports, remarks, and inputs.
The data was checked for eligibility and completeness and subjected to a set of predefined plausibility tests. These included checks for contradictory data, duplication, and plausibility of time measurements.
Statistics
Continuous variables were summarized as medians/interquartile ranges (IQRs), and categorical data were recorded as frequencies. The level of significance was set at 0.05. We described patient and psychiatrist characteristics using descriptive analyses. Nonparametric tests were used to compare the number of consultations between different modes of contact during on-duty episodes and in cases of non-normally distributed data. Correlation analyses (Spearman’s) were performed between variables related to satisfaction with the current service. The χ2 test was used to compare levels of threats and violence (categorical data) between male and female psychiatrists. In addition, analysis was controlled for clustering with the psychiatrist as cluster level where relevant, thus taking into account that patient observations are not independent, ie, observations in one cluster tend to be more similar to each other than to individuals in the rest of the sample. All analyses were calculated using the STATA (StataCorp, College Station, TX, USA) statistical package, version 11.2.
Ethics approval and consent
Approval of the evaluation of the 24-hour emergency services in Zurich was given by the Ethics Committee of the Canton of Zurich (reference Nr 26/09). Since data collection was performed by the attending psychiatrist and only anonymous data were reported for further analysis, no consent of patients was required.
Results
The evaluation period consisted of 167 24-hour emergency service episodes. Of these, 74 (44%) were documented by a total of 44 psychiatrists.
Patient contact (telephone and direct encounters)
The participating psychiatrists reported on 291 consultations during the study period. The median consultation rate per 24-hour service was 4 (IQR 0–8). Consultations included “face-to-face” (direct) patient contact inside or outside of a private practice as well as telephone contact with patients or their family members/friends. The median of direct patient encounters per 24-hour service (telephone contacts excluded) was 3 (IQR 1–6). From the 291 documented consultations, sociodemographic and clinical information on 189 (64.9%) direct patient encounters was available.
Table 1 shows the inquiry distribution over the EMST switchboard. The most common requests for emergency services were made by the police (15.1%), family members (14.8%), and the patients themselves (11.7%).
  | Table 1 Inquiry distribution over the EMST switchboard |
Considering the number of requests per hour, most requests occurred between 7 pm and 10 pm (24.8%). From 7 am to 7 pm, 70 (49.6%) requests occurred, and from 10 pm to 7 am, 36 (25.5%) requests occurred.
Of all patient contacts, 34.7% could be completely handled by telephone and required no further consultation or personal contact. From all the completed phone consultations (N=85), a bill was issued in 20% of cases. Of the direct patient encounters, 1.3% took place in the private practice of the attending psychiatrists. The vast majority of encounters took place at patients’ private homes (36.4%), at police stations (24.0%), or at other institutions such as prison, clinics, or special care homes (total 38%).
Direct patient encounters (without telephone contact)
The clinical data on the 189 documented direct patient encounters is shown in Table 2. In 49.2%, the problem was solved on location: involuntary hospitalization was necessary in 50.3%. Police presence was requested in 14.3%, and ambulance services were requested in 34.4%.
  | Table 2 Clinical details on direct patient encounters |
The mean time between receiving the call for emergency via the EMST switchboard to the time of consultation was 20.8 minutes (standard deviation [SD] 39.7), the mean travel time (back and forth) was 46.9 minutes (SD 21.7) (n=16), and the mean patient time was 74.9 minutes (SD 37.6). Mean costs were estimated at €386.7 (SD 161.6, 95% confidence interval 169.6–673.3). Bills were issued to the patient in 48.3% of cases, to the health insurance company in 23.3% of cases, to the police in 9.1% of cases, and to other institutions in 19.3% of cases (n=176).
In 83.8% (n=74) of all direct patient encounters, the involved psychiatrist retrospectively judged the meeting as adequate at the patients’ location, only in 16.2% was the encounter estimated to have possibly been manageable in a private practice or other ambulatory setting. These findings did not change when controlled for the psychiatrist as potential cluster effect (83.8% versus 81.4%).
Information on situations with potential for violence was available for 74 direct patient encounters: in 39.7% of contacts, psychiatrists felt threatened by patients; in 6.8%, actual violence occurred. These findings were not changed when additionally controlled for the psychiatrist as potential cluster effect (39.7% versus 39.5% and 6.8 versus 6.9%). No difference between female and male psychiatrists was found concerning feeling threatened (P=0.285) or violence occurring (P=0.392).
A total of 43 different diagnoses were classified according to ICD-10 (average of 1.37 diagnoses/direct patient encounter). In cases where no adequate ICD-10 diagnosis could be applied, the free-text diagnosis was integrated into the analysis. Diagnoses from the chapter “Schizophrenia, schizotypal and delusional disorders” were most commonly reported (23.9%), followed by “suicidal” (15.2%) and “acute stress reaction” (10.2%) (Table 3).
Participating psychiatrists
Of the 44 psychiatrists who participated in the study, 52% were female. The mean age was 49.91 (SD 5.20) years, with men being slightly older (mean 50.51 (SD 6.21) versus 49.35 (SD 4.04), P<0.05). The mean time participants had worked in private practice was 12.7 (SD 5.52) years, with men having had more experience in private practice (mean 14.08 [SD 6.10] versus 11.39 [SD 4.64] years, P<0.05). In total, emergency services were performed in the last 9.89 (SD 6.95) years, with men having had significantly more experience in emergency services than women (12.51 [SD 7.92] years versus 6.79 [SD 3.93] years, P<0.05).
No differences between males and females concerning further analyses could be observed; therefore, all results were pooled for presentation.
Table 4 illustrates the level of pressure psychiatrists felt during the current emergency service system. They were mainly tense (74.36%) and often felt they were encountering dangerous situations (37.50%) or felt burdened by the encounters (62.50%). The majority did not like to provide emergency services (52.50%). There was a positive association between the level of “feeling burdened by the emergency service” and the frequency “dangerous encounters” during the emergency service (Spearman’s rho =0.53, P<0.001), whereas higher levels of “feeling tense” was negatively correlated with “liking to provide emergency service” (Spearman’s rho =−0.56, P<0.001).
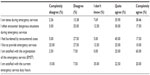  | Table 4 Physicians’ level of pressure during, and satisfaction with, the current emergency service (n=40) |
The preferred length of service was similarly distributed between 12- and 24-hour cycles (44.74% and 55.26%, respectively). Should 12-hour shifts be implemented in future, the preferred time interval was 8 am to 8 pm (85.71%) rather than 7 am to 7 pm or 12 am to 12 pm (both 7.14%). If 24-hour shifts should be implemented in future the preferred time interval was 8 am to 8 pm (55.56%) rather than 7 am to 7 pm or 12 am to 12 pm (11.11% and 33.33%, respectively).
If the provision of emergency services was optional, 45.24% would participate in the service, 33.33% would not participate, and 21.43% were unsure.
Certain issues with the handling of the emergency service are listed in Table 5. The numbers are based on personal estimates and not on observations performed in the study sample: problems with handing over shifts to the successor were reported as “seldom” in 40%. Bills not being paid for were reported as “often” in 32.43%, and almost all psychiatrists closed their private practice during emergency services (95.24%). Psychiatrists mostly performed the service alone without any assistance (85.71%).
  | Table 5 Problems with the emergency service |
No bivariate association was observed between the level of reported unpaid bills and “feeling burdened by the emergency service” or “liking to provide emergency services”.
Discussion
Our survey provides detailed information on frequency, mode of contact, and reasons for 24-hour primary care emergency psychiatric services performed by mandatory rotation of licensed psychiatrists in an urban setting in Switzerland. It also offers an insight into the participating psychiatrists’ degree of satisfaction with the current service.
Demand of the service
The total frequency of patient encounters during a 24-hour emergency-service period (median 4.0, IQR 0–8) was slightly lower compared with previously published data of a general practitioner emergency service in Zurich, where a median of five patient contacts per duty period were recorded.10 This difference in contact rates reflects the lower prevalence of psychiatric compared with somatic emergencies in the general population. When comparing contact rates with those in a very similar system offered to the general population in Israel, the rate was identical,2 even though in Israel a psychiatrist on duty is responsible for a substantially larger population than a psychiatrist in Zurich (population 2.7 million versus 400,000). The Israeli study by Khawaled et al2 described a newly implemented psychiatric service in an urban setting; therefore, it is likely that the general population was not yet aware of this service, resulting in lower contact rates compared with the long-standing service offered in Zurich. The study also does not explicitly mention the exact times during which the service is provided, it remains unclear whether an emergency service period consists of 24 hours or less, thus making direct comparisons difficult. Further comparison concerning contact rates in mobile emergency services of other countries was difficult due to differences in organizational structures of the services.
Interestingly, as already observed in the Swiss study on emergency out-of-hours services provided by general practitioners,10 visits at the patient’s location were significantly more frequent than telephone or practice consultations. According to the psychiatrists on duty, the vast majority of these visits could not have been handled in an outpatient clinic or a private practice, a finding which is also reflected in the hospitalization rate of 50%, being in line with hospitalization rates found in the literature.11
Diagnoses
The psychiatrists in this study documented 43 different diagnoses, of which “schizophrenia, schizotypal and delusional disorders”, “suicidal”, and “acute stress reaction” accounted for almost half of all documented diagnoses. These findings are in line with other studies on psychiatric services2,12,13 and do not come as a surprise since 75% of patients with schizophrenic disorders have relapses and continued disability, and one-third fail to respond to standard treatment.14
Psychiatrists’ satisfaction with the current service
The participating psychiatrists experienced the current emergency service as a burden, with a significant correlation to the feeling of being exposed to dangerous situations. No difference between male and female psychiatrists could be found concerning feeling threatened or the amount of actually occurring dangerous situations. The following findings are possible reason for the large amount of burdened psychiatrists: the majority of psychiatrists provided the service alone; only in half of the consultations at the patients’ location police or ambulance were present; and in a substantial amount of contacts (7%) actual danger situations occurred. This level of burden is consistent with other Swiss studies on satisfaction among general practitioners providing primary care emergency services.10,15 Danger and associated stress situations have been reported to a similar extent in other countries providing psychiatric emergency services.16–18 Also, the fact that the private practice was closed during emergency service periods, combined with a relatively low contact rate of about four consultations in 24 hours (telephone and direct encounters), and inappropriate psychiatrist remuneration due to an estimated one-third of bills being unpaid, could be additional important reasons for dissatisfaction with the current system. The extent to which psychiatrists liked providing the service seemed to have diverse causes and did not depend on the earnings alone. To raise the satisfaction level among the providing psychiatrists, certain changes concerning the organization of the service should be considered besides increased financial compensation, especially when taking into consideration that burden and stress levels among psychiatrists are substantial.
Strengths and limitations
This is the first study on the current psychiatric 24-hour emergency service in the area of Zurich, which represents the largest city in Switzerland with about 400,000 inhabitants. We consider the results being representative due to the following considerations: the participation rate of 44% was high, considering usual participation rates in questionnaire-based studies are about 30%,19 as was the completeness of returned questionnaires; from the documented 291 emergency contacts, clinical information on direct patient encounters was available for the majority of cases (65%). The participating psychiatrists represent a sample of real-life psychiatrists matching the Swiss annual statistics on sex and age distribution20 dealing with real-life cases from primary care. Furthermore, results remained unchanged when additionally controlled for a potential cluster effect. Currently in literature, very little national and international data is available on 24-hour emergency psychiatric services provided by licensed psychiatrists with private practices via rota systems; therefore, systematic comparisons are difficult. This rota system of licensed psychiatrists is unique to Switzerland. In some cantons, psychiatrists are called to emergencies outside of hospitals by general practitioners on duty as second line, if necessary, or the patients are referred to psychiatric institutions. In no other Swiss region do psychiatrists provide their own first-line out-of-hours emergency service. The reasons for differences in cantons are mainly due to the number of available psychiatrists working in private practices. In Zurich currently, we seem to be in a comfortable position concerning the number of psychiatrists in private practice compared with other regions. In most other countries, as in other regions of Switzerland, emergency psychiatric services seem to be provided by general practitioners, psychiatrists in training, multidisciplinary specialized psychiatric emergency teams, or hospitals. Some private organizations also perform emergency services in Zurich. Data from these organizations as well as of different other emergency care services in the city (ie, emergency departments and walk-in centers) were not available for our study. Living situation was not assessed in our study population; therefore, it is not possible to address the issue of providing emergency psychiatric services to a subset of the general population highly burdened with psychiatric issues, namely the homeless population. Nevertheless, our results – especially regarding distribution of diagnoses and hospitalization rates – are similar to previous findings from Switzerland21 and other countries and indicate the validity of our assessment.
Implications
Previous studies have shown a positive effect on general practitioners’ satisfaction, stress levels, general health status, and quality of life after the introduction of a general practitioner out-of-hours cooperative into accident and emergency services.22–24 The question of whether the implementation of a similar system into the emergency psychiatric service is a viable alternative to the existing service is therefore justified. Since the vast majority of psychiatric consultations in our study were carried out by home-visit (or outside of a practice) and could not have been dealt with in an ambulatory setting, the implementation of such a system into the emergency psychiatric service seems not to cover the needs of the majority of emergency psychiatric patients and is therefore not a viable solution for reorganization. The findings from several international studies have suggested that mobile community-based emergency interventions are preferable to hospital-based interventions, since they reduce hospital admission rates, decrease family burden, show higher cost effectiveness, and offer a more satisfactory form of care from the consumer’s perspective.2,11,25–27 It is therefore necessary to optimize the current system in a way which on the one hand takes patients’ needs into consideration, eg, the need for direct psychiatrist visits at the location of the patient, and on the other hand raises the satisfaction level among the providing psychiatrists, especially targeting burden and stress levels, besides increased remuneration. Possible solutions are the implementation of mobile units consisting of specialized nurses, police, and psychiatrists.11 To reduce the level of burden and stress for the psychiatrist, the organization of services in Zurich has been adapted as a result of this study; length of service shifts was reduced from 24 to 12 hours in exchange for an increased number of shifts (from 5 to 10 annually). Further possible structural adaptations are currently under evaluation.
Conclusion
Our findings indicate a justified patients’ demand for direct mobile patient visits in 24-hour primary care emergency psychiatric services, suggesting that emergency care should be multifaceted, and the sole provision of psychiatric care at locally stationed emergency facilities may not be an appropriate approach for all patients. Ongoing reorganization of emergency services should therefore carefully evaluate patient’s and provider’s needs before changing established structures.
Acknowledgments
We would like to thank Dr med Vladis Hliddal and med Pract Michèle Abelovsky, consulting psychiatrists from the “Zürcher Gesellschaft für Psychiatrie und Psychotherapie”, for their substantial contribution in the design of the study and the interpretation of the results. We would like to thank the staff of the EMST switchboard who coordinated the mailing of the survey and motivated the psychiatrists to participate. We would also like to thank the participating psychiatrists for enabling this study.
Financial support
Unconditional financial support of ZGPP (Zürcher Gesellschaft für Psychiatrie und Psychotherapie) and ZüriMed (ärzteverband der Bezirke Zürich und Dietikon).
Disclosure
The authors report no conflicts of interest in this work.
References
Johansen I, Carlsen B, Hunskaar S. Psychiatry out-of-hours: a focus group study of GPs’ experiences in Norwegian casualty clinics. BMC Health Serv Res. 2011;11(1):132. | |
Khawaled R, Bauer A, Rosca P, et al. Community emergency psychiatric service in Israel: a one-year experience. Isr J Psychiatry Relat Sci. 2009;46(3):207–212. | |
Muller U, Winterhalder R, Businger A, Zimmermann H, Exadaktylos AK. Why do walk-in patients prefer a busy urban emergency department during office hours? A pilot survey of 200 consecutive patients from Switzerland. Swiss Med Wkly. 2012;142:w13565. | |
Flaig C, Zehnder K, Zürcher H, et al. Selbsteinweisungen ins Spital. [Admissions to hospital]. PrimaryCare. 2002;10:280–283. German. | |
Huibers L, Giesen P, Wensing M, Grol R. Out-of-hours care in Western countries: assessment of different organizational models. BMC Health Serv Res. 2009;9:105. | |
Grol R, Giesen P, van Uden C. After-hours care in the United Kingdom, Denmark, and the Netherlands: new models. Health Aff (Millwood). 2006;25(6):1733–1737. | |
Salisbury C. The demand for out-of-hours care from GPs: a review. Fam Pract. 2000;17(4):340–347. | |
Chmiel C, Huber C, Rosemann T, et al. Walk-ins seeking treatment at an emergency department or general practitioner out-of-hours service: a cross-sectional comparison. BMC Health Serv Res. 2011;11(1):94. | |
Rau SA, Zwahlen M. Comparison between two caller groups of a medical call centre in Switzerland. Gesundheitswesen. 2008;70(5):295–304. | |
Huber CA, Rosemann T, Zoller M, Eichler K, Senn O. Out-of-hours demand in primary care: frequency, mode of contact and reasons for encounter in Switzerland. J Eval Clin Pract. 2011;17(1):174–179. | |
Scott RL. Evaluation of a mobile crisis program: effectiveness, efficiency, and consumer satisfaction. Psychiatr Serv. 2000;51(9):1153–1156. | |
Fleury M-J, Grenier G, Bamvita J-M, Caron J. Mental health service utilization among patients with severe mental disorders. Community Ment Health J. 2011;47(4):365–377. | |
Cahoon EK, McGinty EE, Ford DE, Daumit GL. Schizophrenia and potentially preventable hospitalizations in the United States: a retrospective cross-sectional study. BMC Psychiatry. 2013;13(1):37. | |
Smith T WC, Lieberman J. Schizophrenia (maintenance treatment). Am Fam Physician. 2010;82(4):338–339. | |
Hugentobler W. Kostenvergleich der ambulanten Notfallversorgung in der hausaerztlichen Praxis mit den Notfallstationen der Spitaeler. [Cost comparison of outpatient emergency services between general practitioners practice and emergency departments of hospitals]. PrimaryCare. 2006;32–33(6):586–589. German. | |
D’Urso P, Hobbs R. Aggression and the general practitioner. BMJ. 1989;298:97–98. | |
Gascon S, Martinez-Jarreta B, Gonzalez-Andrade JF, Santed MA, Casalod Y, Rueda MA. Aggression towards health care workers in Spain: a multi-facility study to evaluate the distribution of growing violence among professionals, health facilities and departments. Int J Occup Environ Health. 2009;15(1):29–35. | |
Ness G, House A, Ness A. Aggression and violent behaviour in general practice: population based survey in the north of England. BMJ. 2000;320:1447–1448. | |
McAvoy BR, Kaner EF. General practice postal surveys: a questionnaire too far? BMJ. 1996;313(7059):732–733; discussion 733–734. | |
FMH Swiss Medical Association [homepage on the Internet]. FMH-Ärztestatistik – Überblick verschaffen. Available from: http://www.fmh.ch/themen/aerztedemographie/aerztestatistik.html. Accessed February 16, 2014. | |
Klein SD, Bischoff C, Schweitzer W. Suicides in the canton of Zurich (Switzerland). Swiss Med Wkly. 2010;140:w13102. | |
Pickin DM, O’Cathain A, Fall M, Morgan AB, Howe A, Nicholl JP. The impact of a general practice co-operative on accident and emergency services, patient satisfaction and GP satisfaction. Fam Pract. 2004;21(2):180–182. | |
van Uden CJ, Nieman FH, Voss GB, Wesseling G, Winkens RA, Crebolder HF. General practitioners’ satisfaction with and attitudes to out-of-hours services. BMC Health Serv Res. 2005;5(1):27. | |
Fletcher J, Pickard D, Rose J, et al. Do out-of-hours co-operatives improve general practitioners’ health? Br J Gen Pract. 2000;50(459):815–816. | |
Burns T, Knapp M, Catty J, et al. Home treatment for mental health problems: a systematic review. Health Technol Assess. 2001;5(15):1–139. | |
Merson S, Tyrer P, Onyett S, et al. Early intervention in psychiatric emergencies: a controlled clinical trial. Lancet. 1992;339(8805):1311–1314. | |
Flannery F, Adams D, O’Connor N. A community mental health service delivery model: integrating the evidence base within existing clinical models. Australas Psychiatry. 2011;19(1):49–55. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

