Back to Journals » International Journal of General Medicine » Volume 15
Dapagliflozin and Empagliflozin in Heart Failure with Reduced Ejection Fraction: A Retrospective Study
Received 23 March 2022
Accepted for publication 19 May 2022
Published 1 July 2022 Volume 2022:15 Pages 5915—5918
DOI https://doi.org/10.2147/IJGM.S366943
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Zhengyang Hao, Yanzhou Zhang
Department of Cardiology, the First Affiliated Hospital of Zhengzhou University, Zhengzhou, 450052, People’s Republic of China
Correspondence: Yanzhou Zhang, Department of Cardiology, the First Affiliated Hospital of Zhengzhou University, Zhengzhou, 450052, People’s Republic of China, Email [email protected]
Objective: Dapagliflozin 10 mg and empagliflozin 10 mg have been recommended to treat heart failure with reduced ejection fraction (HFrEF), and the purpose of this study was to compare the efficacy and safety of them in HFrEF.
Methods: Two hundred and thirty-three patients with HFrEF admitted to a tertiary hospital of Zhengzhou and commenced to take dapagliflozin 10 mg/d or empagliflozin 10 mg/d were retrospectively included and separated into the dapagliflozin group (n=105) and the empagliflozin group (n=128). Their cardiac function indices before and after therapy were compared, together with the ratios of adverse events during therapy.
Results: After 6 months of therapy, left ventricular ejection fraction was higher, and the ratio of New York Heart Association functional class III or IV, left ventricular end-diastolic diameter, and N-terminal pro-B-type natriuretic peptide were lower in the empagliflozin group than the dapagliflozin group (P< 0.05). During 6 months of therapy, there were no statistically significant differences for the ratios of hypotension, deteriorating kidney function, and genitourinary infections between the dapagliflozin and empagliflozin groups (P> 0.05).
Conclusion: Despite its many limitations, this study suggested that different SGLT2 inhibitors might have differences regarding efficacy in HFrEF. We look forward to future studies to verify our conjectures.
Keywords: dapagliflozin, empagliflozin, heart failure with reduced ejection fraction
Introduction
Sodium-glucose cotransporter-2 (SGLT2) inhibitors, including dapagliflozin and empagliflozin, are a new type of oral glucose-lowering drugs that can control blood glucose by inhibiting SGLT2 in the kidney. The DAPA-HF trial1 and the EMPEROR-Reduced trial2 suggested that dapagliflozin and empagliflozin, respectively, could lower the incidences of cardiovascular adverse events in patients suffering from heart failure with reduced ejection fraction (HFrEF).
Dapagliflozin 10 mg and empagliflozin 10 mg are recommended to treat HFrEF, but it is undetermined whether or not they are different in terms of efficacy and safety in HFrEF. This study was performed to compare the efficacy and safety of dapagliflozin 10 mg and empagliflozin 10 mg in HFrEF.
Methods
Study Patients
A total of 233 patients with HFrEF admitted to a tertiary hospital of Zhengzhou and commenced to take dapagliflozin 10 mg/d or empagliflozin 10 mg/d were included in this single-center retrospective study. Patients in this study were in New York Heart Association (NYHA) functional class II or III, had a left ventricular ejection fraction (LVEF) of less than 40% measured by transthoracic echocardiography, and had been treated with dapagliflozin 10 mg/d or empagliflozin 10 mg/d for more than 6 months.
The study was approved by the ethics committee of the hospital, and all included patients were informed and consented.
Study Design
Data of these patients were acquired by the electronic medical record system. Basic data contained demographic characteristics, vital signs, laboratory indicators, diseases, and medications.
Cardiac function indices, containing NYHA functional class, transthoracic echocardiographic indicators [containing LVEF and left ventricular end-diastolic diameter (LVEDD)], and N-terminal pro-B-type natriuretic peptide (NT-proBNP), before and after 6 months of therapy were recorded.
Adverse events, containing hypotension, deteriorating kidney function, and genitourinary infections, during 6 months of therapy were also recorded. Patients would be diagnosed with hypotension if their systolic blood pressure was below 90 mmHg, and when their serum creatinine increased by more than 25% or 0.3 mg/dL compared to before therapy, they would be diagnosed with deteriorating kidney function.
Statistical Analysis
Continuous variables and categorical variables were reported as means ± standard deviations and frequencies (percentages), respectively. Comparisons of the variables between the dapagliflozin and empagliflozin groups were made using independent sample t-test, Pearson’s chi-square test, or Fisher’s exact test. P<0.05 was considered to indicate a statistically significant difference.
Results
Basic Data
Among the 233 patients, 105 were on dapagliflozin and 128 were on empagliflozin. The age of the dapagliflozin group was 68.6±12.9 years, 62 were males and 43 were females, and the age of the empagliflozin group was 67.5±13.1 years, 71 were males and 57 were females. There were no statistically significant differences regarding demographic characteristics, vital signs, laboratory indicators, diseases, and medications between the dapagliflozin and empagliflozin groups (P>0.05). Table 1.
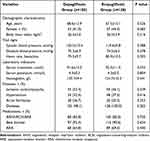 |
Table 1 Basic Data |
Cardiac Function Indices
After 6 months of therapy, LVEF was higher, and the ratio of NYHA functional class III or IV, LVEDD, and NT-proBNP were lower in the empagliflozin group when compared with the dapagliflozin group (P<0.05). Table 2.
 |
Table 2 Cardiac Function Indices |
Adverse Events
During 6 months of therapy, there were no statistically significant differences for the ratios of hypotension, deteriorating kidney function, and genitourinary infections between the dapagliflozin and empagliflozin groups (P>0.05). Table 3.
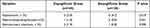 |
Table 3 Adverse Events |
Discussion
This study showed that after 6 months of therapy, LVEF was higher, and the ratio of NYHA functional class III or IV, LVEDD, and NT-proBNP were lower in the empagliflozin group compared with the dapagliflozin group. Meanwhile, during 6 months of therapy, the differences in the ratios of hypotension, deteriorating kidney function, and genitourinary infections between the dapagliflozin and empagliflozin groups were not statistically significant. These results suggested that different SGLT2 inhibitors might have differences in efficacy when treating HFrEF.
SGLT2 inhibitors can bring multiple benefits to patients suffering from HFrEF. The literatures3,4 suggested that they could not only reduce the volumes of left atrium and left ventricle, but also benefit life quality. A study5 suggested that SGLT2 inhibitors could shift utilization of myocardial fuel away from glucose to branched-chain amino acid, free fatty acid, and ketone bodies, and this is perhaps one of the mechanisms by which LVEF increases among some patients. In addition to these, SGLT2 inhibitors may ameliorate interstitial myocardial fibrosis, inflammatory markers, as well as aortic stiffness.6
The glucose-lowering effects of different SGLT2 inhibitors may be different.7 In this study, after 6 months of therapy, LVEF was higher, and the ratio of NYHA functional class III or IV, LVEDD, and NT-proBNP were lower in the empagliflozin group than the dapagliflozin group, suggesting that empagliflozin 10 mg might ameliorate heart function more significantly among HFrEF patients compared with dapagliflozin 10 mg. On the other hand, this study also found that the ratios of hypotension, deteriorating kidney function, and genitourinary infections during 6 months of therapy between the two groups were statistically insignificant, suggesting that dapagliflozin 10 mg and empagliflozin 10 mg might have similar safety profiles when treating HFrEF.
Limitations
This study has many limitations, for instance: 1. Echocardiography examinations were performed by different sonographers, which might have influenced the results. 2. The doses of other drugs, including sacubitril/valsartan, metoprolol, and spironolactone, were not recorded, which might not be conducive to the comparison of these two SGLT2 inhibitors. 3. The effects of dapagliflozin and empagliflozin on the prognosis of HFrEF patients were not compared.
Conclusion
Because of the limitations of this study, we could not conclude that 10 mg of empagliflozin is superior to 10 mg of dapagliflozin when treating HFrEF. After 6 months of therapy, the differences in several cardiac function indices between the two groups were statistically significant, therefore, we speculated that the efficacies of different SGLT2 inhibitors in HFrEF might be different. We look forward to future studies to verify our conjectures.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381(21):1995–2008. doi:10.1056/NEJMoa1911303
2. Packer M, Anker SD, Butler J, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020;383(15):1413–1424. doi:10.1056/NEJMoa2022190
3. Omar M, Jensen J, Ali M, et al. Associations of empagliflozin with left ventricular volumes, mass, and function in patients with heart failure and reduced ejection fraction: a substudy of the empire HF randomized clinical trial. JAMA Cardiol. 2021;6(7):836–840. doi:10.1001/jamacardio.2020.6827
4. Requena-Ibáñez JA, Santos-Gallego CG, Rodriguez-Cordero A, et al. Empagliflozin improves quality of life in nondiabetic HFrEF patients. Sub-analysis of the EMPATROPISM trial. Diabetes Metab Syndr. 2022;16(2):102417. doi:10.1016/j.dsx.2022.102417
5. Santos-Gallego CG, Requena-Ibanez JA, San Antonio R, et al. Empagliflozin ameliorates adverse left ventricular remodeling in nondiabetic heart failure by enhancing myocardial energetics. J Am Coll Cardiol. 2019;73(15):1931–1944. doi:10.1016/j.jacc.2019.01.056
6. Requena-Ibáñez JA, Santos-Gallego CG, Rodriguez-Cordero A, et al. Mechanistic insights of empagliflozin in nondiabetic patients with HFrEF: from the EMPA-TROPISM Study. JACC Heart Fail. 2021;9(8):578–589. doi:10.1016/j.jchf.2021.04.014
7. Blonde L, Patel C, Wu B, et al. Real-world comparative effectiveness of canagliflozin versus empagliflozin and dapagliflozin in patients with type 2 diabetes in the United States. Adv Ther. 2021;38(1):594–606. doi:10.1007/s12325-020-01549-x
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
