Back to Journals » OncoTargets and Therapy » Volume 7
Cytologic surveillance versus immediate colposcopy for women with a cervical smear diagnosis of low-grade squamous intraepithelial lesion in a poor setting in Nigeria
Authors Ajah LO , Chigbu CO, Onah HE, Iyoke CA , Lawani OL, Ezeonu PO
Received 10 July 2014
Accepted for publication 17 October 2014
Published 27 November 2014 Volume 2014:7 Pages 2169—2173
DOI https://doi.org/10.2147/OTT.S70930
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Faris Farassati
LO Ajah,1,2 CO Chigbu,1 HE Onah,1 CA Iyoke,1 OL Lawani,2 PO Ezeonu2
1Department of Obstetrics and Gynaecology, University of Nigeria Teaching Hospital, Enugu, 2Department of Obstetrics and Gynaecology, Federal Teaching Hospital, Abakaliki, Nigeria
Background: Ideally, all patients with abnormal Papanicolaou smear cytology results should undergo colposcopic examination of the cervix, but low-grade squamous intraepithelial lesions (LSILs) can also be followed up with further Papanicolaou smear surveillance. The aim of this study was to evaluate the outcome of cytologic surveillance versus immediate colposcopy in women with a cervical smear diagnosis of LSIL.
Methods: This was a prospective comparative study of 240 eligible consenting women consecutively grouped into cervical surveillance for 6 months versus immediate colposcopy at a ratio of 1:1. Free cervical smear cytology, colposcopy, and biopsy, as well as histology, were provided for all study participants.
Results: The regression, persistence, and progression rates with 6 months of cytologic surveillance of LSIL were 46.1%, 43.4%, and 3.9%, respectively. The difference between the proportions of women who had an eventual histologic diagnosis of cervical intraepithelial neoplasia 2+ in both groups was not statistically significant (4.9% versus 8.7%; P=0.68). The default rates among women on cytologic surveillance and immediate colposcopy were 37% and 12.5%, respectively (P=0.0002).
Conclusion: Although the progression rate of LSIL is low, a high persistence rate and higher default rate from cytologic surveillance highlight the need to consider immediate referral for colposcopy, where available, for all women with a Papanicolaou smear diagnosis of LSIL in this environment.
Keywords: cytologic surveillance, immediate colposcopy, low-grade squamous intraepithelial lesions, Enugu
Introduction
Papanicolaou smear cytology has remained a important tool in the screening for cervical cancer.1 Ideally, all patients with abnormal Papanicolaou smear cytology results should undergo colposcopic examination.2 The current evidence prefers reflex human papillomavirus (HPV) testing for women with atypical squamous cells of undetermined significance (ASCUS) cytology test results. However, for women with HPV-positive ASCUS, whether from reflex HPV testing or cotesting, and women with low-grade squamous intraepithelial lesion (LSIL) cytology test results and no HPV test or a positive HPV test result, colposcopy is recommended.3 Further, in women with a histologic diagnosis of cervical intraepithelial neoplasia (CIN) 2, CIN 3, or CIN 2/3 and adequate colposcopic examination, both excision and ablation are acceptable treatment modalities, except in pregnant women and young women.3
A good proportion of LSILs regress spontaneously to normal,4 hence a policy of cytologic surveillance helps to reduce the workload pressure on colposcopy services. Further, workload pressure on colposcopy services appears to be more of a problem in developed countries.5 In Africa and other developing regions, workload pressure on colposcopy services appears not to be a problem because uptake of colposcopy services is poor.6
However, it has recently been observed that cytologic regression occurs in only 25% of cases, thus questioning the rationale for cytologic surveillance instead of immediate colposcopy. Cytologic surveillance is also associated with significant psychological morbidity for women, who have to wait for 6 months for the next cytology test results.7 Default of a cytologic surveillance appointment is yet another issue that might adversely affect implementation of a cytologic surveillance policy in developing countries. While a report from the UK, with its organized cervical cancer screening program, indicated a default rate of 21%,8 this may be worse in a poor setting like ours in Nigeria where there is no such organized program. This suggests that a policy of cytologic surveillance may face significant challenges in implementation in Nigeria and possibly other developing countries. On the other hand, a policy of immediate referral for colposcopy has raised concerns about possible overtreatment, complications, anxiety, lack of resources, and delays.9–13 Patient default from colposcopy is also a reported problem, but to a lesser degree than from cytologic surveillance.6
Management by cytologic surveillance has raised concern that some cases of high-grade disease might escape detection because of loss to follow-up or limited sensitivity.14 Even at the best centers in the world, an estimated 65%–75% of women with LSIL will eventually be referred for colposcopy.7,15–17 In our environment, more proportion of women with LSIL may be referred for colposcopy and besides, we may not have a dedicated follow-up obtainable in the developed world. The ALTS (ASCUS/LSIL Triage) trial in the USA revealed that women whose index cytology showed LSIL would be best managed by immediate colposcopy.16
A study that compared the cost of colposcopy with that of multiple repeated smears suggested that immediate colposcopy would be cheaper.17 Although the Papanicolaou smear has become the accepted method of screening for cervical neoplasia all over the world, with significant reductions in the incidence of cervical cancer and the associated death rate in areas where mass screening is organized, widespread, and prolonged, the major drawback of this technique has been its limited sensitivity, with reports of false negative rates ranging from as low as 1.5% to as high as 80%.18,19 This is largely attributed to errors of sampling and interpretation.20 Eventually, the complementary use of cytology and colposcopy for identification and evaluation of women at risk of CIN and its precursors is thought to secure the highest yield of detection of cervical neoplasia.21 A Medline literature search did not yield any previous studies that compared cytologic surveillance with immediate colposcopy in Nigeria or other developing countries.
There is currently no organized cervical cancer screening program in Nigeria. Therefore, there is no formal guideline for the management of women with a cervical smear diagnosis of LSIL. Even though colposcopy services are very limited in Nigeria, uptake of these services is very poor in our environment.6 This may be due to lack of awareness among women regarding colposcopy services or part of poor uptake of cervical cancer screening in not only Nigeria but also other sub-Saharan African countries. Hence, from the foregoing, the noted differences in the practice environment between developed and developing countries require that the outcome of cytologic surveillance versus immediate colposcopy in women with a cervical smear diagnosis of LSIL be evaluated in a poor setting like ours. This study may help to provide evidence of a better management protocol for LSIL in our environment. It may also help to provide patients for the training of residents on cervical cancer screening and treatment at our center.
Materials and methods
This study was carried out at the cervical cancer screening unit of the University of Nigeria Teaching Hospital (UNTH), Enugu, between July 1, 2011 and May 31, 2013. The study population included all women who had a Papanicolaou smear at the UNTH during the study period. The study sample included women with a smear diagnosis of LSIL. It was a prospective comparative study in which all eligible consenting women with a smear diagnosis of LSIL were consecutively recruited into one of two groups, ie, A or B. All participants with odd numbers were assigned to group A for cytologic surveillance and those with even numbers were assigned to group B for immediate colposcopy. Group A women underwent repeat Papanicolaou smear cytology at 6 months after their initial cytology. Telephone calls and even home visits (for women who had no telephones or inactive telephone numbers) were made to remind the women about their appointment dates. Those with ASCUS and persistent LSIL or worse at 6 months underwent colposcopic examination of the cervix and colposcopically directed cervical biopsies as appropriate. Those with cytologic regression to normal were integrated into routine cervical cancer screening for the normal general population at UNTH. Group B women had immediate colposcopy and colposcopically directed cervical biopsy as appropriate. Pregnant women, those with abnormal vaginal bleeding or obvious cervical lesions, and women who refused to give consent were excluded from the study.
The minimal sample size in each group for cytologic surveillance and immediate colposcopy was calculated to be 87, but 120 was used in this study. Ethical clearance for the study was obtained from the ethics committee of UNTH, Enugu. The statistical analysis was done using Statistical Package for Social Sciences version 16 software (SPSS Inc., Chicago, IL, USA). The chi-square test was used for discrete variables and P-values <0.05 were considered to be statistically significant.
Results
A total of 240 women who met the inclusion criteria participated in the study. One hundred and twenty women were allocated to each study group. The age distribution of the women was 21–70 years, with a mean age of 45.01±12.55 years. Table 1 summarizes the sociodemographic characteristics of the study participants. There was no statistical significant difference between the two groups of participants on the sociodemographic characteristics.
  | Table 1 Sociodemographic data of study participants |
Table 2 summarizes the repeat Papanicolaou smear results for participants on cytologic surveillance and the outcome of colposcopy and biopsy for participants on cytologic surveillance and immediate colposcopy. For women in the cytologic surveillance group, 63.3% (76/120) came for a repeat cervical smear 6 months after the initial cytology, while 44 (37%) defaulted. Cytologic regression, persistence, and progression of LSIL after 6 months were 46.1%, 43.4%, and 3.9%, respectively. A total of 15 (12.5%) women defaulted, while 105 (87.5%) underwent colposcopy and biopsy.
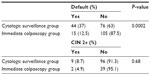
Table 3 shows a comparison of the default rate and histologic diagnosis of CIN 2+ between women who had cytologic surveillance and those who had immediate colposcopy. Significantly more women defaulted from repeat Papanicolaou smear at 6 months than from immediate colposcopy (37% versus 12.5%; P=0.0002). The difference between the proportions of women who had an eventual histologic diagnosis of CIN 2+ in the two groups was not statistically significant (4.9% versus 8.7%; P=0.68).
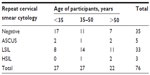
Table 4 summarizes the age distribution of participants on cytologic surveillance with repeat cervical smear cytology. It shows that the regression of LSIL to normal cytology after 6 months was higher among participants younger than 35 years of age.
Discussion
The regression rate of LSIL among women who had cytologic surveillance was higher in our study than that reported in the USA (46.1% versus 25%, respectively),7 but was lower than the 61% and 91% recorded among young females over 12 and 24 months, respectively, in France.22 The majority of the women enrolled into this study were aged 41–60 years, whereas women in the French study22 were considerably younger (13–22 years). Repeat Papanicolaou smear cytology in women allocated to the cytologic surveillance group at 6 months revealed a 43.4% persistence of LSIL and 3.4% progression to HSIL. Our persistence rate was higher than the 15% reported in South Carolina, USA, but our progression rate was less than the 17% reported at the same center.7
On comparison of cytologic surveillance and immediate colposcopy with regard to the outcome of a diagnosis of CIN 2+, there was no statistically significant difference between the two groups. This finding was similar to that in a study by the TOMBOLA (Trial Of Management of Borderline and Other Low-grade Abnormal smears) group.23 While there was only worse cases of CIN 2 among the women in the cytologic surveillance group, there were worse cases of CIN 2, CIN 3, and squamous cell carcinoma of the cervix among the women in the immediate colposcopy group. These worse cases, especially CIN 3 and squamous cell carcinoma, would have been missed and probably deteriorated further if not for immediate colposcopy. The 37% default rate reported for the cytologic surveillance group in this study was higher than the 21% previously reported in the UK,8 but similar to the 42% reported in the USA.7 The default rates recorded in this study were despite the free Papanicolaou smear screening, colposcopy, biopsy, and treatment services that were implemented. There were also repeated telephone calls and even home visits (for women who did not have a telephone or had misplaced it) aimed at reminding and encouraging the women to attend their appointment. The default rate from immediate colposcopy of 12.5% recorded in this study was similar to the 9% reported in the UK.24
Conclusion
Even though the progression rate of LSIL is low, a high persistence rate of LSIL and a high default rate from cytologic surveillance at 6 months’ follow-up highlight the need to consider immediate referral to colposcopy, where available, for all women with a Papanicolaou smear diagnosis of LSIL in this environment. Free cervical cancer screening and referral for immediate colposcopy of women with a smear diagnosis of LSIL should be implemented by all stakeholders to help stem the tide of cervical cancer in our setting. Further research is needed to explore ways of improving patient compliance with follow-up procedures after a positive Papanicolaou smear diagnosis. This study was limited by the intraobserver and interobserver errors associated with cervical smear cytology, colposcopy, and biopsy, and histology results, and by its lack of a randomized design.
Acknowledgment
We wish to thank Mrs Onyeonu and Mrs Eze, nurses at UNTH, for their invaluable assistance with data collection in this study.
Author contributions
LOA conceived and designed the study, carried out the procedures, collated, analyzed, and interpreted the data, drafted the manuscript, and contributed to the study funding. COC helped in modifying the topic to make it more meaningful. He also participated in the design of the project, execution of the procedures, collation and interpretation of the data, and drafting of the manuscript. HEO helped in modifying the topic to make it more meaningful, participated in the design of the project, interpretation of the data, and drafting of the manuscript. CAI, OLL, and POE participated in the design of the project, collation and interpretation of data, and drafting of the manuscript. All the authors helped to fund this study.
Disclosure
The authors report no conflicts of interest in this work.
References
Ugboma HAA, Aburoma HLS. Pap smear: an important screening technique for preventing and detecting cervical cancer. Continental Journal of Medical Research. 2010;4:13–17. | |
Shafi MI. Premalignant and malignant lesions of the cervix. In: Edmonds DK, editor. Dewhurst’s Textbook of Obstetrics and Gynaecology. 7th ed. Oxford, UK: Blackwell Publishing; 2007. | |
Massad LS, Einstein MH, Huh WK, Katki HA, Kinney WK, Schiffman M, et al. 2012 Updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. Obstet Gynecol. 2013;121:829–846. | |
Bansal N, Wright JD, Cohen CJ, Herzog TJ. Natural history of established cervical intraepithelial neoplasia (CIN) 1 lesions. Anticancer Res. 2008;28:1763–1766. | |
Eggington S, Hadwin R, Brennan A, Walker P. Modelling the impact of referral guideline changes for mild dyskaryosis on colposcopy services in England Sheffield: NHS Cancer Screening Programmes, 2006. NHSCSP Publication No 24. Available from: http://www.cancerscreening.nhs.uk/cervical/publications/nhscsp24.html. Accessed October 30, 2014. | |
Chigbu CO, Aniebue UU. Non-uptake of colposcopy in a resource-poor setting. Int J Gynaecol Obstet. 2011;113:100–102. | |
Yoost JL, Goetzi L, Hoda R, Sopa DE, Barry A. Management of the low grade squamous intraepithelial lesion Pap smear in a cross-sectional, observational cohort. J Reprod Med. 2009;54:421–424. | |
Shafi MI, Luesley DM, Jordan JA, Dunn JA, Rollason TP, Yates M. Randomised trial of immediate versus deferred treatment strategies for the management of minor cervical cytological abnormalities. Br J Obstet Gynaecol. 1997;104:590–594. | |
Ferlay J, Bray F, Pisani P, Parkin DM. GLOBOCAN 2002 Cancer Incidence, Mortality and Prevalence Worldwide. Lyon, France: IARC Cancer Base; 2004. | |
Chokunonga E, Levy LM, Bassett MT, Mauchaza BG. Zimbabwe cancer registry. In: Parkin DM, Whelan SL, Ferlay J, Storm HH, editors. Cancer Incidence in Five Continents. Volume VIII. Lyon, France: IARC Press; 2002. | |
Sankaranarayanan R, Ferlay J. Worldwide burden of gynaecological cancer: the size of the problem. Best Pract Res Clin Obstet Gynaecol. 2006;20:207–225. | |
Anorlu RI, Orakwue CO, Oyeneyin L, Abudu OO. Late presentation of cervical cancer in Lagos: what is responsible? Eur J Gynaecol Oncol. 2004;25:729–732. | |
Cronje HS. Screening for cervical cancer in developing countries. Int J Gynaecol Obstet. 2004;84:101–108. | |
Taylor RJ, Morrell SL, Mamoon HA, Wain GV. Effects of screening on cervical cancer incidence and mortality in New South Wales implied by influences of period of diagnosis and birth cohort. J Epidemiol Community Health. 2001;55:782–788. | |
Kyrgiou M, Koliopoulos G, Martin-Hirsch P, et al. Management of minor cervical cytological abnormalities: a systematic review and a meta-analysis of the literature. Cancer Treat Rev. 2007;33:514–520. | |
ASCUS-LSIL Traige Study (ALTS) Group. A randomized trial on the management of low-grade squamous intraepithelial lesion cytology interpretations. Am J Obstet Gynecol. 2003;188(6):1393–1400. | |
Johnson N, Sutton J, Thornton JG, Lilford RJ, Johnson VA, Peel KR. Decision analysis for best management of mildly dyskaryotic smear. Lancet. 1993;342:91–96. | |
Pairwuti S. False negative Papanicolaou smears from women with cancerous and precancerous lesions of the uterine cervix. Acta Cytol. 1991;35:40–46. | |
Wain GV, Farnsworth A, Hacker NF. The Papanicolaou smear histories of 237 patients with cervical cancer. Med J Aust. 1992;157:14–16. | |
Joste NE, Crum CP, Cibas ES. Cytologic/histologic correlation for quality control in cervicovaginal cytology: Experience with 1,582 paired cases. Am J Clin Pathol. 1995;103:32–34. | |
Dodd LG, Sneige N, Villarreal Y, et al. Quality-assurance study of simultaneously sampled, non-correlating cervical cytology and biopsies. Diagn Cytopathol. 1993;9(2):138–144. | |
Moscicki AB, Shiboski S, Hills NK, et al. Regression of low-grade squamous intra-epithelial lesions in young women. Lancet. 2004;364(9446):1678–1683. | |
TOMBOLA Group. Cytological surveillance compared with immediate referral for colposcopy in management of women with low grade cervical abnormalities: multicentre randomised controlled trial. BMJ. 2009;339:b2546. | |
Balasubramani L, Orbell S, Hager M, Brown V, Tidy J. Can default rates in colposcopy really be reduced? BJOG. 2008;115:403–408. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.