Back to Journals » Drug Design, Development and Therapy » Volume 16
Cyclosporine A (0.05%) Ophthalmic Gel in the Treatment of Dry Eye Disease: A Multicenter, Randomized, Double-Masked, Phase III, COSMO Trial
Authors Peng W, Jiang X, Zhu L, Li X, Zhou Q, Jie Y , You Z, Wu M, Jin X, Li X , Zhou S
Received 10 May 2022
Accepted for publication 30 August 2022
Published 20 September 2022 Volume 2022:16 Pages 3183—3194
DOI https://doi.org/10.2147/DDDT.S370559
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Tuo Deng
Wenyan Peng,1,* Xiuying Jiang,1,* Lei Zhu,2,* Xiaofeng Li,3,* Qizhi Zhou,4,* Ying Jie,5 Zhipeng You,6 Miaoqin Wu,7 Xiuming Jin,8 Xiaoyi Li,9 Shiyou Zhou1
1State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangzhou, 510060, People’s Republic of China; 2Henan Provincial People’s Hospital, Henan Eye Institute, Henan Eye Hospital, People’s Hospital of Zhengzhou University, Zhengzhou University, Zhengzhou, 450003, People’s Republic of China; 3Department of Ophthalmology, Chengdu Aier Eye Hospital, Sichuan, People’s Republic of China; 4Department of Ophthalmology, Chongqing Aier Eye Hospital, Chongqing, People’s Republic of China; 5Department of Ophthalmology, Beijing Tongren Eye Center, Beijing Tongren Hospital, Capital Medical University, Beijing, People’s Republic of China; 6Department of Ophthalmology, The Second Affiliated Hospital of Nanchang University, Nanchang, People’s Republic of China; 7Department of Ophthalmology, Zhejiang Provincial People’s Hospital, People’s Hospital of Hangzhou Medical College, Hangzhou, Zhejiang, People’s Republic of China; 8Department of Ophthalmology, The Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, Zhejiang, People’s Republic of China; 9Zhaoke Ophthalmology Ltd, Guangzhou, 511458, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Shiyou Zhou, State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangzhou, 510060, People’s Republic of China, Tel +8620-6661-5460 ; +86-13829709097, Fax +8620-87333271, Email [email protected]
Purpose: To confirm the efficacy and safety of a novel ophthalmic cyclosporine A gel (CyclAGel, 0.05% CsA) in treating patients with moderate-to-severe dry eye disease (DED).
Patients and Methods: The COSMO trial was a randomized, multicenter, double-masked, vehicle-controlled, phase III trial. Patients with moderate-to-severe DED were enrolled in 37 hospitals in China between November 2020 and April 2021. Eligible patients were randomized 1:1 to receive CyclAGel 0.05% or vehicle eye drops once nightly (QD). The primary endpoint was the proportion of subjects with at least a 1-point improvement in ICSS at day 84. Treatment-emergent adverse events (TEAEs) were recorded.
Results: The full analysis set (FAS) included 315 and 312 participants in the CyclAGel and vehicle groups, respectively. The primary efficacy endpoint was achieved. The proportion of subjects with at least a 1-point improvement in ICSS from baseline to day 84 was significantly higher in the CyclAGel group than in the vehicle group (73.7% [232/315] vs 53.2% [166/312], P< 0.0001). Significant improvements relative to the vehicle were also observed in the ICSS and Oxford scale scoring of corneal and conjunctival fluorescein staining at day 14, 42, and 84. The Schirmer tear test results were significantly higher in the CyclAGel group than in the vehicle group on days 14 and 84 (all P< 0.05). The CyclAGel 0.05% was well tolerated, and the TEAEs were mostly mild. The most frequent treatment-related TEAE was eye pain (6.9% vs 1.6% in the CyclAGel and vehicle groups, respectively). No serious treatment-related TEAEs were reported.
Conclusion: Clinically and statistically significant improvements in ICSS, tear production, and symptoms were observed in participants administered CyclAGel 0.05% QD for moderate-to-severe DED. CyclAGel 0.05% QD is a new effective, safe, and well-tolerated therapeutic option that might bring additional benefits of convenience and compliance as a once-A-day treatment for DED.
Keywords: dry eye disease, cyclosporine, ophthalmic gel, corneal staining, dryness score
Introduction
Dry eye disease (DED) is a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film and is accompanied by ocular symptoms.1 Tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiological roles in DED.1
Common symptoms of DED include ocular dryness, foreign body sensation, burning sensation, eye itching, pain, redness, visual fatigue, blurred vision, and fluctuating visual acuity.2–4 DED is the second most common ophthalmic disease to affect vision and quality of life, behind refractive errors.4,5 The prevalence of DED based on the WHS criteria is 23% in China,2,3,5 and patients with DED account for approximately 30% of all patients in ophthalmology clinics in China.2
The etiology of DED is multifactorial and can be attributed to aqueous deficient dry eye, evaporative dry eye, or a combination of both.5 The pathogenesis of DED is related to immune-related inflammatory mediators, environmental stress, reduction in androgen levels, and the increasing use of visual display terminals. Inflammation is a major factor in the development and progression of DED but is also an outcome of DED, resulting in a vicious cycle.6 Drying stress induces Th1-related inflammatory cytokines on the ocular surface.7 Severe DED often has an accompanying inflammatory response at the ocular surface, and these patients have increased levels of pro-inflammatory cytokines in their tears.7 Inflammation is one of the key features of DED,7 and the Dry Eye Workshop (DEWS) definition emphasizes the role of inflammation in the pathophysiology of DED.8
Cyclosporine A (CsA) is a selective immunomodulator that decreases T-cell activation and T-lymphocyte infiltration of the lacrimal glands, inhibits the apoptosis of ocular surface epithelial cells, and is effective in treating DED.9–12 The mechanisms of action of CsA mainly include increasing tear production, reducing the release of inflammatory cytokines, and protecting conjunctival epithelial cells.13 The Chinese expert consensus on DED (2020) recommends using CsA ophthalmic formulations in the treatment of moderate-to-severe DED with ocular inflammation.14 The Dry Eye Syndrome Preferred Practice Pattern by the American Academy of Ophthalmology suggests that topical cyclosporine can lead to long-term treatment-free remission of DED symptoms and signs.15 The CsA ophthalmic emulsion 0.05% (twice-daily, Restasis®; Allergan, Irvine, California, USA) and CsA ophthalmic solution 0.09% (twice-daily, Cequa; Sun Pharmaceutical Industries, Cranbury, NJ) have been approved by the FDA for the treatment of DED.16 There is only one generic CsA formulation 0.05% (twice-daily, Shenyang Xingqi Pharmaceutical Co. Ltd.) approved for DED treatment in China. The most common side effect of ocular CsA treatment is an ocular burning sensation,16 and other side effects include blurred vision, ocular itching, conjunctival hyperemia, discharge, foreign body sensation, and stinging.17,18
Due to the above-mentioned side effects and low bioavailability of the available ophthalmic CsA formulations,19 a novel CsA ophthalmic gel formulation (CyclAGel) was developed, which is expected to result in fewer side effects due to increased comfort and reduced frequency of use (only once every night). The Phase II study showed that CyclAGel has a better efficacy against DED signs and symptoms than Restasis, with excellent safety, tolerability, and comfort profiles in moderate-to-severe DED.20 The safety and efficacy of CyclAGel were initially evaluated through a phase II dose-ranging (0.05% and 0.1%) study, and the lowest drug concentration in the phase II study (0.05%) that showed the most significant improvement was selected for this phase III trial in CyclAGel group.20 Here we present the results of a phase III study evaluating the safety and efficacy of CyclAGel 0.05% (once daily [QD]) compared with the vehicle for treating patients with moderate-to-severe DED.
Methods
Study Design and Patients
The COSMO trial was a multicenter, randomized, double-masked, vehicle-controlled phase III clinical trial. Patients with moderate-to-severe DED treated in the Department of Ophthalmology of 37 hospitals in China between November 2020 and April 2021 were enrolled. This study was registered with ClinicalTrials.gov (identifier, NCT04541888). The study protocol was approved by the ethics committees of all participating centers and adhered to the tenets of the Declaration of Helsinki. All participants provided written informed consent before enrollment.
The inclusion criteria were 1) 18–80 years of age and 2) diagnosis of moderate-to-severe DED with all four signs or symptoms: a. eye dryness score (EDS) ≥40 (ranges 0–100 by the visual analog scale [VAS] method); b. tear film break-up time (BUT) <10 s; c. Schirmer tear test without anesthesia <10 mm/5 min; d. inferior corneal staining score (ICSS) ≥2 (ranges 0–4; 0 = none, 4 = coalescent, 1-point increments).
The exclusion criteria were 1) severe DED requiring surgical treatment, 2) intraocular eye surgery within 12 months prior to screening or during the study, 3) permanent punctual occlusion or temporary lacrimal plug treatment within 6 months prior to screening, 4) surgery-induced dry eye, 5) diagnosis of glaucoma, 6) inability or unwillingness to avoid contact lens use during the study, 7) history of viral keratitis, 8) diagnosis of ocular mucous membrane pemphigoid, obvious conjunctival scar, ocular chemical burn, or neurotrophic keratoconjunctivitis, 9) menopausal women using hormone replacement therapy, 10) severe cardiopulmonary disease or impaired liver or kidney function, 11) inability or unwillingness to stop using other eye preparations after receiving eluting drugs, 12) participation in other clinical trials within 1 month prior to screening, 13) use of systemic or topical CsA within 1 month prior to screening, 14) known hypersensitivity to CsA, fluorescein, or any component of the study drug, or 15) any participant considered inappropriate for participation in the study by the investigators, including those who were unable to or unwilling to comply with the study protocol. If both eyes met the enrollment requirements, the more severe eye was selected as the study eye.
Randomization and Masking
This study used block randomization. A statistician independent to the study (not masked) used the SAS statistical software to generate the randomization table. The participants were assigned 1:1 to the CyclAGel group or vehicle group. The investigators and participants were masked to grouping. Unmasking of the participants was permitted at the investigators’ discretion only in the case of an emergency requiring medical intervention.
Treatment
A run-in period was conducted prior to randomization (from day −14 to day −1), during which all participants received the assigned artificial tear and the CyclAGel vehicle for at least 14 days. The assigned artificial tear was hypromellose methylcellulose eye drops (Shanghai Sine-Jinzhu Pharmaceutical Co., Ltd.), one or two drops, three times a day. The vehicle (Zhaoke [Guangzhou] Ophthalmology Pharmaceutical Limited, Guangzhou, China) was used once every night, one drop each time (at least 5 min apart from using the artificial tear).
After randomization (ie, from day 0), the participants in the CyclAGel group used the 0.05% CsA gel (Zhaoke [Guangzhou] Ophthalmology Pharmaceutical Limited) once every night, one drop each time. The participants in the vehicle group continued to use the vehicle once every night, one drop each time (at least 5 min apart from using the artificial tear). Both groups used the concomitant hypromellose methylcellulose eye drops three times a day, one or two drops each time, according to the Chinese expert consensus on DED (2020)14 and requirement of the Ethics Committee of the leading center. All the drug packages in this study were provided uniformly by Zhaoke [Guangzhou] Ophthalmology Pharmaceutical Limited. They were packed by personnel not involved in this study in accordance with the randomization table.
Clinical Assessments
Follow-up was conducted at days 0, 14±2, 42±4, and 84±6. ICSS and the Oxford scale scoring of corneal and conjunctival fluorescein staining (ranges 0–15) were evaluated. ICSS instead of central or complete corneal staining score was used because the inferior zone most commonly exhibited the most severe corneal staining in symptomatic DED.21 ICSS was used for primary efficacy assessment in the OPUS-1/2 trials as well.22,23 Anesthetized Schirmer tear test, BUT test, and slit-lamp examination were performed. The VAS scores for dry eye symptoms (burning/stinging sensation, itching, foreign body sensation, discomfort, photophobia, and pain) were reported by the patients.
Efficacy Endpoints
The primary efficacy endpoint was defined as the proportion of subjects with a reduction of ICSS ≥ 1 from baseline to day 84. Subgroup analyses were performed based on age (≥65 vs <65 years), sex, and baseline ICSS. The secondary efficacy endpoints were the changes in indicators from baseline on days 14, 42, and 84, including 1) EDS of both eyes, 2) VAS scores (0–100 points) of the six symptoms of both eyes, including burning/stinging sensation, itching, foreign body sensation, discomfort, photophobia, and pain, 3) ICSS of the study eye, 4) Oxford scale scoring of corneal and conjunctival staining scores of the study eye, 5) BUT of the study eye, and 6) anesthetized Schirmer tear test of the study eye.
Safety and Compliance Assessment
Treatment-emergent adverse events (TEAEs) were recorded according to the Medical Dictionary for Regulatory Activities (MedDRA) and listed as overall TEAEs, ocular TEAEs, and non-ocular TEAEs at each visit. Serious adverse events (SAEs) were defined as new or prolonged hospitalization, disability, inability to work, life-threatening medical events, death, or congenital malformation. Compliance (%) = actual number of doses / number of planned doses × 100%. A calculated value within 80–120% was defined as good compliance, while <80% or >120% was defined as poor compliance.
Sample Size Calculation
The primary endpoint was the proportion of participants with at least a 1-point improvement in ICSS from baseline to day 84. The estimated values of the primary endpoint in the CyclAGel and vehicle groups were 30.7% and 18.5%, respectively, based on preliminary data. A superiority trial design was used. The power analysis was performed a priori. Unilateral α was set at 0.025, and β was set at 0.1. A total of 514 cases were required for the two groups. Considering a lost-to-follow-up rate of 20%, 644 cases were enrolled in this study, 322 in each group.
Statistical Analysis
The full analysis set (FAS) included all participants who used the drug at least once after randomization and had at least one measure of the primary efficacy indicator after enrollment. If participants withdrew from the study early due to poor efficacy or ocular TEAEs, they were considered to have not met the primary endpoint. If the participants withdrew from the study early for other reasons, the last observation carried forward (LOCF) method was used to fill in the primary efficacy indicator. The safety set (SS) included all participants who used the drug at least once after randomization and had at least one safety assessment.
The continuous variables that conformed to a normal distribution were expressed as mean ± standard deviation, and the two groups were compared using Student’s t-test. Continuous variables that did not conform to a normal distribution were presented as median (min, max), and the two groups were compared using the Mann–Whitney U-test. Categorical variables were expressed as n (%), and the two groups were compared using the chi-square test or Fisher’s exact test. Repeated measures were compared using repeated-measure ANOVA. Forest plots were drawn for the subgroup analyses. Statistical analysis was performed using SAS 9.4 (SAS Institute, Cary, NY, USA). The primary endpoint was evaluated using a one-sided test, and P<0.025 was considered statistically significant. The other statistical analyses were performed using a two-sided test, and P<0.05 was considered statistically significant.
Results
Patient Enrollment and Baseline Characteristics
Figure 1 presents the participant flowchart. During the study period, 804 participants were enrolled; 644 participants entered the 14-day run-in period. The participants were randomized 1:1 to the CyclAGel 0.05%/QD (n=322) or vehicle/QD (n=322) group. Finally, 298 and 301 participants in the CyclAGel and vehicle groups completed the trial. The dropout rate was 7%. The SS included 321 and 314 patients in the CyclAGel and vehicle groups, respectively. The FAS included 315 and 312 patients in the CyclAGel and vehicle groups, respectively. There were no statistically significant differences in the baseline characteristics between the two groups in terms of age (45.0±13.7 vs 44.5±14.2 years), sex (male: 18.1% vs 16.3%), body mass index (22.9±3.4 vs 22.5±2.9 kg/m2), DED duration (median: 4.3 vs 5.9 months, Mann–Whitney U-test, P=0.3586), DED affected side, and study eye (all P>0.05) (Table 1).
 |
Table 1 Baseline Characteristics of the Participants |
 |
Figure 1 Study flowchart. Abbreviations: SS, safety set; FAS, full analysis set. |
Efficacy Evaluation
Primary Endpoint
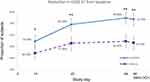
The proportion of subjects with at least a 1-point improvement in ICSS from baseline to day 84 was 73.7% (232/315) in the CyclAGel group vs 53.2% (166/312) in the vehicle group (P<0.0001), achieving the study primary endpoint. On days 14 and 42, the proportions of subjects with at least a 1-point improvement in ICSS from baseline were also significantly higher in the CyclAGel group compared with the vehicle group (54.5% vs 44.2%, P=0.0052; 69.2% vs 52.8%, P<0.0001; Figure 2). According to the subgroup analyses, females <65 years were more likely to benefit from CyclAGel (Figure 3).
Secondary Endpoints
The secondary endpoints are presented in Figure 4, Tables 2 and 3. The mean changes from baseline in ICSS and Oxford scale scoring of corneal and conjunctival fluorescein staining on days 14, 42, and 84 were significantly higher in the CyclAGel group than in the vehicle group (all P<0.05). The mean changes from baseline in the Schirmer tear test on days 14 and 84 were higher in the CyclAGel group than in the vehicle group (both P<0.05), but the difference was not significant on day 42. No statistically significant differences between groups regarding the mean changes of BUT from baseline to days 14, 42, and 84 were observed (all P>0.05). Concerning symptoms, the EDS on day 84 was significantly decreased from baseline in both groups (mean value, −29 in the CyclAGel group vs −31 in the vehicle group, P=0.346). Other symptoms, including itching, foreign body sensation, photophobia, burning/stinging sensation, discomfort, and pain, were significantly decreased at day 84 compared to baseline in both groups. No superiority of CyclAGel over the vehicle regarding binocular symptom scores was observed at any visit.
 |
Table 2 Changes from Baseline in DED Signs of the Study Eye at Days 14, 42, and 84 |
 |
Table 3 Changes in Binocular Symptom Scores from Baseline at Days 14, 42, and 84 |
Safety and Compliance
In the SS, 127 (39.6%) participants in the CyclAGel group reported 224 TEAEs, including 44 (13.7%) participants reporting 71 TEAEs related to the study drug. In addition, 96 (30.6%) participants in the vehicle group reported 162 TEAEs, including 20 (6.4%) participants reporting 37 TEAEs related to the study drug. The most common TEAEs in all participants were eye pain, eye foreign body sensation, vision loss, and urinary tract infection (Table 4). Drug discontinuation due to TEAEs in the two groups was observed in five (1.6%) and three (1.0%) participants, respectively. The incidences of SAE were six (1.9%) and two (0.6%), respectively. All SAEs were non-ocular and irrelevant to the study drugs. During the study period, the average compliance was 98.9% and 99.0% in the CyclAGel and vehicle groups, respectively.
 |
Table 4 Incidence of Treatment-Emergent Adverse Events (TEAEs) |
Discussion
The COSMO phase III clinical trial aimed to confirm the efficacy and safety of CyclAGel in treating patients with moderate-to-severe DED. More subjects in the CyclAGel group (73.7%) than in the vehicle group (53.2%) had at least a 1-point improvement in ICSS from baseline to day 84 (end of the study), achieving the primary efficacy endpoint. Moreover, the changes from baseline to day 84 in ICSS, Oxford scale scoring of corneal and conjunctival fluorescein staining, and Schirmer tear test in the CyclAGel group were all significantly better than in the vehicle group. These results suggest that CyclAGel improves the DED signs and symptoms in patients with moderate-to-severe DED. In addition, it has good safety and patient tolerance.
Previous studies reported that the efficacy of CsA ophthalmic preparations was superior to vehicles in patients with DED, which was consistent with the main findings of this study.24–28
One of the challenges for topical administration of cyclosporine to the eyes is the high hydrophobicity, which impedes the use of common aqueous ophthalmic vehicles. Therefore, cyclosporine is usually dissolved in olive oil or oil-based emulsions, which are poorly tolerated and result in low ocular availability because of the short retention time on the ocular surface.13 CyclAGel dissolves cyclosporine to form a transparent stable hydrogel so that it is directly available to the ocular surface, which is in contrast to emulsions requiring liberation from micelles. The CyclAGel in the present study is the first hydrogel preparation of CsA. Carbomer in the vehicle acts as a stabilizing agent, has good adherence to the ocular surface, and does not induce ocular irritation.13 In addition, CyclAGel in cornea, conjunctiva, and tears showed superior Cmax and area under the concentration-time curve than Restasis. Thus, the effective concentration of CyclAGel in conjunctiva and cornea could be maintained over a long time. High bioavailability and long effective concentration maintenance time enable CyclAGel to achieve good efficacy.
Notably, the baseline ICSS in the present study was 3.0, indicating moderate-to-severe corneal epithelial defect. On day 84, the mean ICSS improved to 1.7 (mild corneal epithelial defect) in the CyclAGel group. A severe corneal epithelial defect is difficult to recover from, while CyclAGel 0.05% accelerate severe corneal epithelial defects healing and can shift moderate-to-severe to mild corneal epithelial defects within 12 weeks. Lifitegrast®, a small molecule LFA-1 antagonist, was approved by the FDA for treating patients with DED in July 2016. The proportion of patients with at least a 1-point improvement in ICSS from baseline to day 84 was 22.2% in the Lifitegrast group (mean baseline ICSS of 1.84) in the OPUS-1 study,22 compared with 73.7% in the CyclAGel group and 69.7% in the subgroup with a baseline ICSS of 2 in the present study. In other words, CyclAGel 0.05% once every night showed promising efficacy for corneal epithelial defects healing in moderate-to-severe DED. Furthermore, real-world experience showed that improvements in DED signs and symptoms were evident at 3 months and up to 12 months after Lifitegrast initiation,29 and 0.1% CsA cationic emulsion usually take 3–6 months to show efficacy against DED signs and symptoms,30 while the onset time of CyclAGel 0.05% was within 2 weeks. Nevertheless, formal comparisons among different drugs for DED require head-to-head trials.
Regarding the relief of DED symptoms, both groups showed improvements compared with baseline. The vehicle also contained lubricants that might help alleviate the symptoms, which might be why the CyclAGel group showed no statistically significant difference over the vehicle group for some symptoms. Meanwhile, symptoms are quite variable and subjective indicators, especially in severe DED patients.31 Subjects in the present study had moderate-to-severe corneal epithelial defects, which might increase the variability of symptoms. Modification to collecting data on symptoms is needed in future studies to increase the accuracy. EDS, at least, improved significantly from baseline (approximately 40%). The phase II study of 0.05% CyclAGel once daily showed that the change from baseline in EDS scores after 84 days of treatment was −29.17±23.77,20 consistent with a mean value of −31 (range, −94 to 23) in the present phase III trial.
According to the subgroup analyses, female <65 years were more likely to benefit from CyclAGel (Figure 3). The major risk factors for DED are age, sex, androgen deficiency, and menopause.4,5 As the proportion of menopausal females and males with decreased androgen levels will be higher in the participants >65 years group than in the participants <65 years age group, there is probably a higher likelihood of intractable DED in older participants, especially in menopausal females.
Regarding safety, the rates of overall TEAEs and TEAEs related to the study drug were lower than those of the phase II study. The most common TEAEs were eye pain (8.1%), eye foreign body sensation (2.2%), and eye irritation (2.2%) in the CyclAGel group. Most of the TEAEs were mild/moderate. Eight subjects reported SAEs, which were all ruled to be unrelated to the study drug. The overall safety characteristics were consistent with the phase II trial of CyclAGel20 and clinical trials of other CsA ophthalmic formulations.24–28 No new safety signals were observed. In addition, instillation site pain was reported in 24.2% of patients receiving OTX-101 0.09% solution23 and in 22% of patients receiving Lifitegrast.25 In contrast, no instillation site pain was reported in the CyclAGel group, indicating better patient comfort. The average patient compliance during the study period was above 98%, which might be related to less frequent medication use (only once every night) and better patient comfort. Still, the safety profile should be compared with other topical medications for DED in the future. In addition, DED is a chronic condition requiring long-term treatment. The stable, homogeneous, and clear nature of CyclAGel, along with its frequency of use of only once a day, makes it an easy-to-use ophthalmic formulation that ensures better long-term adherence, thus helping patients improve their quality of life.
This trial has limitations. First, DED is a long-term condition, but the follow-up duration was short, and the efficacy and safety need to be confirmed by a longer follow-up. Second, patients with surgery-related DED, drug-related DED, contact lenses wear, or DED secondary to systemic diseases were not included in this study, and it is not clear whether the results are consistent in such patients.
Conclusion
In conclusion, CyclAGel 0.05% QD significantly reduced corneal and conjunctival staining and improved tear secretion compared with the control group in moderate-to-severe DED. It also significantly alleviated the symptoms. CyclAGel 0.05% QD is a new effective, safe, and well-tolerated therapeutic option that might bring additional benefits of convenience and compliance as a once-A-day treatment for moderate-to-severe DED.
Ethics Approval and Informed Consent
The study protocol was approved by the ethics committees of all participating centers (Table S2) and adhered to the tenets of the Declaration of Helsinki. All patients provided written informed consent before enrollment.
Acknowledgments
The authors thank the members of the Study Group (Table S1) for providing patient data.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was partly supported by the Fundamental Research Funds of the State Key Laboratory of Ophthalmology (Grant number: 303060202400201119) and the Guangzhou Science and Technology Fund in China.
Disclosure
Xiaoyi Li is affiliated with Zhaoke Ophthalmology Ltd. The authors report no other conflicts of interest in this work.
References
1. Shimazaki J. Definition and diagnostic criteria of dry eye disease: historical overview and future directions. Invest Ophthalmol Vis Sci. 2018;59:DES7–DES12.
2. Chinese Branch of the Asian Dry Eye Society, Ocular Surface and Tear Film Diseases Group of Ophthalmology Committee of Cross-Straits Medicine Exchange Association, Ocular Surface and Dry Eye Group of Chinese Ophthalmologist Association. Chinese expert consensus on dry eye: definition and classification (2020). Zhonghua Yan Ke Za Zhi. 2020;56:418–422.
3. American Academy of Ophthalmology. Preferred Practice Pattern (PPP) Guideline. Dry eye syndrome. San Francisco: American Academy of Ophthalmology; 2018. Available from: https://www.aao.org/preferred-practice-pattern/dry-eye-syndrome-ppp-2018.
4. Clayton JA. Dry eye. N Engl J Med. 2018;378(23):2212–2223. doi:10.1056/NEJMra1407936
5. Craig JP, Nelson JD, Azar DT, et al. TFOS DEWS II report executive summary. Ocul Surf. 2017;15(4):802–812. doi:10.1016/j.jtos.2017.08.003
6. Rhee MK, Mah FS. Inflammation in dry eye disease: how do we break the cycle? Ophthalmology. 2017;124(11):S14–S9. doi:10.1016/j.ophtha.2017.08.029
7. Bron AJ, de Paiva CS, Chauhan SK, et al. TFOS DEWS II pathophysiology report. Ocul Surf. 2017;15(3):438–510. doi:10.1016/j.jtos.2017.05.011
8. Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15(3):276–283. doi:10.1016/j.jtos.2017.05.008
9. Schultz C. Safety and efficacy of cyclosporine in the treatment of chronic dry eye. Ophthalmol Eye Dis. 2014;6:37–42. doi:10.4137/OED.S16067
10. Kymionis GD, Bouzoukis DI, Diakonis VF, Siganos C. Treatment of chronic dry eye: focus on cyclosporine. Clin Ophthalmol. 2008;2:829–836. doi:10.2147/OPTH.S1409
11. Perry HD, Solomon R, Donnenfeld ED, et al. Evaluation of topical cyclosporine for the treatment of dry eye disease. Arch Ophthalmol. 2008;126(8):1046–1050. doi:10.1001/archopht.126.8.1046
12. de Paiva CS, Pflugfelder SC, Ng SM, Akpek EK. Topical cyclosporine A therapy for dry eye syndrome. Cochrane Database Syst Rev. 2019;9:CD010051. doi:10.1002/14651858.CD010051.pub2
13. Periman LM, Mah FS, Karpecki PM. A review of the mechanism of action of cyclosporine A: the role of cyclosporine A in dry eye disease and recent formulation developments. Clin Ophthalmol. 2020;14:4187–4200. doi:10.2147/OPTH.S279051
14. Society CBotADE, Association OSaTFDGoOCoC-SME, Association OSaDEGoCO. Chinese expert consensus on dry eye: treatment (2020). Zhonghua Yan Ke Za Zhi. 2020;56:907–913.
15. Akpek EK, Amescua G, Farid M, et al. Dry eye syndrome preferred practice pattern®. Ophthalmology. 2019;126(1):P286–P334. doi:10.1016/j.ophtha.2018.10.023
16. Periman LM, Perez VL, Saban DR, Lin MC, Neri P. The immunological basis of dry eye disease and current topical treatment options. J Ocul Pharmacol Ther. 2020;36(3):137–146. doi:10.1089/jop.2019.0060
17. Mah F, Milner M, Yiu S, Donnenfeld E, Conway TM, Hollander DA. PERSIST: physician’s evaluation of Restasis(®) satisfaction in second trial of topical cyclosporine ophthalmic emulsion 0.05% for dry eye: a retrospective review. Clin Ophthalmol. 2012;6:1971–1976. doi:10.2147/OPTH.S30261
18. Allergan Inc. Product monograph. restasis multidose, cyclosporine ophthalmic emulsion, 0.05% w/v; 2018. Available from: https://allergan-web-cdn-prod.azureedge.net/allergancanadaspecialty/allergancanadaspecialty/media/actavis-canada-specialty/en/products/pms/9054xmd-2018jun01-en-restasis-multidose.pdf.
19. de Oliveira RC, Wilson SE. Practical guidance for the use of cyclosporine ophthalmic solutions in the management of dry eye disease. Clin Ophthalmol. 2019;13:1115–1122. doi:10.2147/OPTH.S184412
20. Peng W-Y, Chen R-X, Dai H, et al. Efficacy, safety, and tolerability of a novel cyclosporine, a formulation for dry eye disease: a multicenter phase II clinical study. Clin Ther. 2021;43(3):613–628. doi:10.1016/j.clinthera.2020.12.023
21. Woods J, Hutchings N, Srinivasan S, Jones L. Geographic distribution of corneal staining in symptomatic dry eye. Ocul Surf. 2020;18(2):258–266. doi:10.1016/j.jtos.2019.07.009
22. Sheppard JD, Torkildsen GL, Lonsdale JD, et al. Lifitegrast ophthalmic solution 5.0% for treatment of dry eye disease: results of the OPUS-1 Phase 3 study. Ophthalmology. 2014;121(2):475–483. doi:10.1016/j.ophtha.2013.09.015
23. Tauber J, Karpecki P, Latkany R, et al. Lifitegrast ophthalmic solution 5.0% versus placebo for treatment of dry eye disease: results of the randomized phase III OPUS-2 study. Ophthalmology. 2015;122(12):2423–2431. doi:10.1016/j.ophtha.2015.08.001
24. Sall K, Stevenson OD, Mundorf TK, Reis BL. Two multicenter, randomized studies of the efficacy and safety of cyclosporine ophthalmic emulsion in moderate to severe dry eye disease. CsA Phase 3 study group. Ophthalmology. 2000;107(4):631–639. doi:10.1016/S0161-6420(99)00176-1
25. Leonardi A, Messmer EM, Labetoulle M, et al. Efficacy and safety of 0.1% ciclosporin A cationic emulsion in dry eye disease: a pooled analysis of two double-masked, randomised, vehicle-controlled phase III clinical studies. Br J Ophthalmol. 2019;103(1):125–131. doi:10.1136/bjophthalmol-2017-311801
26. Sheppard JD, Wirta DL, McLaurin E, et al. A water-free 0.1% cyclosporine A solution for treatment of dry eye disease: results of the randomized phase 2B/3 ESSENCE study. Cornea. 2021;40(10):1290–1297. doi:10.1097/ICO.0000000000002633
27. Goldberg DF, Malhotra RP, Schechter BA, Justice A, Weiss SL, Sheppard JD. A phase 3, randomized, double-masked study of OTX-101 ophthalmic solution 0.09% in the treatment of dry eye disease. Ophthalmology. 2019;126(9):1230–1237. doi:10.1016/j.ophtha.2019.03.050
28. Kang M-J, Kim Y-H, Chou M, et al. Evaluation of the efficacy and safety of A novel 0.05% cyclosporin A topical nanoemulsion in primary Sjögren’s syndrome dry eye. Ocul Immunol Inflamm. 2020;28(3):370–378. doi:10.1080/09273948.2019.1587470
29. Hovanesian JA, Nichols KK, Jackson M, et al. Real-world experience with lifitegrast ophthalmic solution (Xiidra) in the US and Canada: retrospective study of patient characteristics, treatment patterns, and clinical effectiveness in 600 patients with dry eye disease. Clin Ophthalmol. 2021;15:1041–1054. doi:10.2147/OPTH.S296510
30. Baudouin C, de la Maza MS, Amrane M, et al. One-year efficacy and safety of 0.1% cyclosporine a cationic emulsion in the treatment of severe dry eye disease. Eur J Ophthalmol. 2017;27(6):678–685. doi:10.5301/ejo.5001002
31. Thulasi P, Djalilian AR. update in current diagnostics and therapeutics of dry eye disease. Ophthalmology. 2017;124(11):S27–S33. doi:10.1016/j.ophtha.2017.07.022
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.