Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 11 » Issue 1
Cut-off value of FEV1/FEV6 as a surrogate for FEV1/FVC for detecting airway obstruction in a Korean population
Authors Chung KS , Jung JY , Park MS , Kim YS , Kim SK, Chang J , Song JH
Received 2 June 2016
Accepted for publication 2 July 2016
Published 19 August 2016 Volume 2016:11(1) Pages 1957—1963
DOI https://doi.org/10.2147/COPD.S113568
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Kyung Soo Chung,1,2 Ji Ye Jung,1,2 Moo Suk Park,1,2 Young Sam Kim,1,2 Se Kyu Kim,1,2 Joon Chang,1,2 Joo Han Song1,2
1Division of Pulmonology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Republic of Korea; 2Institute of Chest Disease, Severance Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea
Background: Forced expiratory volume in 1 second (FEV1)/forced expiratory volume in 6 seconds (FEV6) has been proposed as an alternative to FEV1/forced vital capacity (FVC) for detecting airway obstruction. A fixed cut-off value for FEV1/FEV6 in a Korean population is lacking. We investigated a fixed cut-off for FEV1/FEV6 as a surrogate for FEV1/FVC for detecting airway obstruction.
Materials and methods: We used data obtained in the 5 years of the Fifth and Sixth Korean National Health and Nutrition Examination Survey. A total of 14,978 participants aged ≥40 years who underwent spirometry adequately were the study cohort. “Airway obstruction” was a fixed cut-off FEV1/FVC <70% according to the Global Initiative for Chronic Obstructive Lung Disease guidelines. We also used European Respiratory Society/Global Lung Initiative 2012 equations for the FEV1/FVC lower limit of normal.
Results: Among the 14,978 participants (43.5% male, 56.5% female; mean age: 56.9 years for men and 57.0 years for women), 14.0% had obstructive lung function according to a fixed cut-off FEV1/FVC <70%. Optimal FEV1/FEV6 cut-off for predicting FEV1/FVC <70% was 75% using receiver operating characteristic curve analyses (area under receiver operating characteristic curve =0.989, 95% confidence interval 0.987–0.990). This fixed cut-off of FEV1/FEV6 showed 93.8% sensitivity, 94.8% specificity, 74.7% positive predictive value, 98.9% negative predictive value, and 0.8 Cohen’s kappa coefficient. When compared with FEV1/FVC < lower limit of normal, FEV1/FEV6 <75% tended to over-diagnose airflow limitation (just like a fixed cut-off of FEV1/FVC <70%). When grouped according to age and FEV1 (%), FEV1/FEV6 <75% diagnosed more airway obstruction in older participants and mild–moderate stages compared with FEV1/FVC <70%.
Conclusion: A valid fixed cut-off for detecting airway obstruction in a Korean population is FEV1/FEV6 of 75%, but should be used with caution in older individuals and those with mild–moderate airway obstruction.
Keywords: chronic obstructive pulmonary disease, forced expiratory volume in 6 seconds, pulmonary function test, airway obstruction
Introduction
COPD is the fourth leading cause of death worldwide. However, the World Health Organization predicts that it will become the third leading cause of death by 2030. According to a recent report,1 the priority of screening spirometry in asymptomatic patients has been reduced. However, a diagnostic pulmonary function test in symptomatic patients with wheezing, dyspnea, productive cough, or cough is needed (especially in primary care clinics).2 Until now, expensive, labor-intensive, and inconvenient spirometry has been an obstacle in COPD diagnosis. In the United States, only 32% of COPD patients undergo spirometry within 2 years before, or 6 months after, the diagnosis has been made.3 Previously, we showed that only 27.5% of Korean patients with airway obstruction who used COPD-related health care facilities underwent spirometry.4
Several studies5–18 have demonstrated that forced expiratory volume in 6 seconds of exhalation (FEV6), and forced expiratory volume in 1 second (FEV1) of exhalation ratio with FEV6, can be used as convenient and accurate surrogates for forced vital capacity (FVC) and FEV1/FVC, respectively. Owing to its use of a 6-second expiratory maneuver, FEV6 makes spirometry in the office easier, faster, and safer19 than FVC measurement. This theoretical basis enables primary care physicians to use hand-held spirometric devices such as PiKo-6® (nSpire Health, Inc. Longmont, CO, USA) or COPD-6™ (Vitalograph Ltd, Ennis, Co., Clare, Ireland) without having to employ expensive spirometry tests for the screening or diagnosis of COPD, and by easily providing the values of FEV at 1 and 6 seconds of exhalation.
However, an identical cut-off value between FEV1/FEV6 and FEV1/FVC cannot be used for detecting airway obstruction because FEV6 cannot be greater than FVC. Despite this controversy, some reports have argued that FEV1/FEV6 can reduce the sensitivity of detecting airway obstruction, especially in elderly patients with mild airway obstruction.20,21 Therefore, other studies6 have submitted increased cut-off values (73%–76%) of FEV1/FEV6 for detecting airway obstruction to overcome these limitations.
Spirometry indices are influenced by age, height, sex, and ethnicity.22 Therefore, discovering the cut-off value of FEV1/FEV6 for detecting airway obstruction in a nationwide, representative population sample in Korea is worthwhile. The purpose of the present study was to ascertain the cut-off value of FEV1/FEV6 in place of FEV1/FVC for detecting airway obstruction in a Korean population.
Materials and methods
Study population
Data for the present study were obtained from 5 years of the Fifth and Sixth Korean National Health and Nutrition Examination Survey (KNHANES V–VI), which was conducted between January 2010 and December 2014. KNHANES V–VI employed a stratified, multiple-stage, clustered-probability design to select a representative sample of non-institutionalized civilians among a Korean population. These data comprised information on age, ethnicity, sex, height, weight, and pre-bronchodilator spirometry values. A Vmax 2130 Dry Rolling-seal Spirometer (SensorMedics, Yorba Linda, CA, USA) was employed. Spirometry was undertaken by specially trained technicians according to recommendations set by the American Thoracic Society (ATS)/European Respiratory Society (ERS) in 2005.23 Data from a total of 14,978 individuals aged >40 years who underwent complete pulmonary-function tests from KNHANES V–VI were selected for the present study. We analyzed data on FEV1, FEV6, and FVC from subjects with two or more acceptable spirometric performances. The study protocol was approved by the institutional review board of Severance Hospital (approval number: 4-2006-0101). Written informed consent was obtained from patients or their next of kin.
Definition of airway obstruction
All spirometric values came from pre-bronchodilator results in this study. “Airway obstruction” was defined as FEV1/FVC <70% as a fixed cut-off point according to guidelines set by the Global Initiative for Chronic Obstructive Lung Disease (GOLD).24 Severity of airway obstruction was classified as: “mild” (FEV1 ≥80% predicted, GOLD stage I), “moderate” (50%≤ FEV1 <80% predicted, GOLD stage II), “severe” (30%≤ FEV1 <50% predicted, GOLD stage III), and “very severe” (30%≤ FEV1 predicted, GOLD stage IV). In addition, “normal” lung function was defined as FEV1/FVC ≥70% and FVC ≥80% predicted. A “restrictive spirometric pattern” was defined as FEV1/FVC ≥70% and FVC <80% predicted.
ATS/ERS guidelines recommend use of reference equations derived from a representative sample of healthy individuals to determine the lower limit of normal (LLN), taking into account that spirometry indices are influenced by age, height, sex, and ethnicity. However, an officially recognized equation to use as a reference for pulmonary function in Korea is lacking. Hence, we used equations for FEV1/FVC LLN set by the ESR/Global Lung Initiative (GLI) in 2012. These equations were announced by an ERS/GLI taskforce, and were derived from data collected from healthy nonsmokers 3 to 95 years old from 33 countries (including Korea). ERS/GLI 2012 equations provided multiple-ethnicity values and the LLN for spirometry.25 “Airway obstruction” by FEV1/FVC LLN was defined as being below its LLN in the presence of a normal FEV1/FVC.
Statistical analyses
Data were analyzed using SAS v9.2 (SAS Institute Inc., Cary, NC, USA). Baseline characteristics were summarized using numbers and percentages to describe categorical variables, and compared using the chi-squared test. Continuous variables were compared using the Student’s t-test and are presented as the mean ± standard deviation (SD). FEV1/FEV6 was determined for the highest collective sensitivity and specificity using a receiver operating characteristic (ROC) curve for detecting airway obstruction. Cohen’s kappa coefficient (CKC) was used to evaluate agreement between FEV1/FEV6 and FEV1/FVC. Positive predictive value (PPV) and negative predictive value (NPV) were calculated for the most suitable FEV1/FEV6 threshold for the diagnosis of FEV1/FVC <70%.
Results
Study populations
Among the 14,978 participants, 6,515 (43.5%) were male and 2,104 (14.0%) had airway obstruction. A total of 1,018 (6.8%) participants were classified as having mild obstruction, 996 (6.6%) with moderate obstruction, 80 (0.5%) with severe obstruction, and ten (0.1%) with very severe obstruction according to spirometry values. Airway obstruction was more prevalent in male than in female participants (Table 1).
Spirometric diagnosis of airway obstruction
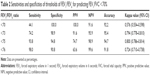
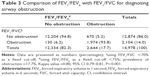
According to the airway obstruction with FEV1/FVC <70%, an ROC curve was used to determine the best corresponding cut-off for FEV1/FEV6 (Figure 1). The area under the ROC curve was 0.989 (95% confidence interval [CI]: 0.987–0.990). The FEV1/FEV6 cut-off corresponding to the greatest sum of sensitivity and specificity was 75%. Table 2 shows the sensitivities and specificities of different thresholds of FEV1/FEV6 for prediction of FEV1/FVC <70%. When choosing an FEV1/FEV6 cut-off of 70%, specificity reached 100% but the sensitivity dropped to 44.1%. A fixed cut-off of FEV1/FEV6 <76% showed high sensitivity (98.0%) and specificity (90.8%) but a low PPV (63.6%). When using a fixed cut-off FEV1/FEV6 of 75%, sensitivity of 93.8%, specificity of 94.8%, PPV of 74.7%, NPV of 98.9%, accuracy of 94.7%, and CKC of 0.8, (95% CI: 0.786–0.814) were obtained, suggesting very good agreement between FEV1/FEV6 and FEV1/FVC. When using a fixed cut-off of FEV1/FEV6 <75%, the number of false-positive cases was 670 (5.2%) and false-negative cases was 130 (6.2%) (Table 3). In particular, false-negative cases were included in mild (n=102) and moderate (n=28) airway-obstruction groups (Table 4).
Comparison of FEV1/FVC < LLN with FEV1/FVC <70% or FEV1/FEV6 <75%
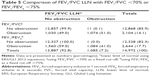
To detect airway obstruction, we compared FEV1/FVC LLN with a fixed cut-off of FEV1/FVC <70% or FEV1/FEV6 <75%. When using FEV1/FVC LLN, the prevalence of obstruction was 7.2%. However, when choosing a fixed cut-off of FEV1/FVC <70% and FEV1/FEV6 <75%, the prevalence of obstruction was 14.1% and 17.7%, respectively. Compared with FEV1/FVC LLN, a fixed cut-off of FEV1/FVC <70% showed 99.0% sensitivity, 92.6% specificity, 93.1% accuracy, 51.1% PPV, and 99.9% NPV. A fixed cut-off of FEV1/FEV6 <75% showed 99.9% sensitivity, 88.8% specificity, 89.6% accuracy, 41.0% PPV, and 99.9% NPV (Table 5). When grouped together according to age and FEV1 (%), a fixed cut-off of FEV1/FEV6 <75% was used to diagnose more airway obstruction in older individuals and those with mild–moderate stages (Table 6). With increasing age and severity of obstruction, the mean difference between FEV1/FEV6 and FEV1/FVC was increasingly larger because FEV6 was increasingly smaller than FVC.
However, with increasing age, the mean difference between FEV1/FVC LLN and FEV1/FVC or FEV1/FEV6 showed only a slight difference. With increasing severity of obstruction, the mean difference between FEV1/FVC LLN and FEV1/FEV6 was larger than the mean difference between FEV1/FVC LLN and FEV1/FVC at mild–moderate stages of airway obstruction, but that was smaller than that at severe and very severe stages (Figures 2 and 3).
Discussion
FEV1/FEV6 and FEV6 are reliable surrogates for FEV1/FVC and FVC to identify obstruction and restriction using spirometry. However, in previous studies, the cut-off values of FEV1/FEV6 for detecting airway obstruction were different among LLN or fixed ratios (70%–76%).6 LLN for FEV1/FEV6 is the most accurate for detecting airway obstruction, but many countries do not have pulmonary function reference equations of LLN for FEV1/FEV6 for local ethnic groups. Nevertheless, primary care clinicians have used handheld spirometric devices such as PiKo-6® or COPD-6™ without proper reference values for FEV1/FEV6. These two devices are inexpensive, and require less quality control of equipment, and no experienced personnel to carry out tests and analyses. The main purpose of the present study was to determine a fixed cut-off value for FEV1/FEV6 as a surrogate for FEV1/FVC for detecting airway obstruction in a Korean population.
The present study elicited two main findings. First, a fixed cut-off for FEV1/FEV6 as a good surrogate for FEV1/FVC for detecting airway obstruction in a Korean population was 75% with 93.8% sensitivity, 94.8% specificity, 74.7% PPV, 98.9 NPV, and good CKC (0.8). Second, a raised fixed cut-off value of FEV1/FEV6 <75% to improve sensitivity showed the tendency to over-diagnosis in the mild–moderate airflow limitation group compared with FEV1/FVC<70% were observed in the mild–moderate airflow limitation group compared with FEV1/FVC. Therefore, a raised and fixed cut-off value of FEV1/FEV6 <75% should be used with caution in older individuals or those with mild–moderate airflow limitation because this cut-off value can lead to over-diagnosis rather than under-diagnosis for airway obstruction screening. A fixed ratio of cut-off led to greater over-diagnosis in patients with mild airflow limitation than LLN, but it was less-time consuming, easier, and safer for patients. Additionally, recording FEV6 was more reproducible than FVC, less physically demanding for patients, and the results were more clear at the end of the test.22
In a study in Belgium, a fixed cut-off of FEV1/FEV6 of <73% showed 94.4% sensitivity, 93.3% specificity, 92.2% PPV, and 95.2% NPV.11 Jing et al showed, in a meta-analysis, that the efficacy of FEV1/FEV6 is not affected adversely by the choice of cut-off point,6 but an appropriate clinical guideline for using FEV1/FEV6 in place of FEV1/FVC is needed. According to one study,26 the cut-off value of pre-bronchodilator FEV1/FEV6 <70% had 91.4% sensitivity, 100% specificity but a 91.4% PPV and 87.4% NPV in 353 Koreans aged >65 years. However, this cut-off value of pre-bronchodilator FEV1/FEV6 <70% cannot be relied upon because the data were from a small study cohort with only older participants; thus the results were not applicable to a general population. Further, a cut-off value of a fixed ratio of FEV1/FVC <70% cannot be applied because FEV6 cannot be greater than FVC – otherwise, airway obstruction may be underestimated. Because an appropriate study on the cut-off of FEV1/FEV6 for airway obstruction in a Korean population had not been carried out, a revised clinical guideline27 for COPD in Korea published in 2014 recommended a cut-off of FEV1/FEV6 of 73% for detecting airway obstruction based on studies undertaken outside Korea.24,27
Our study showed that 75% as a fixed value of FEV1/FEV6 in analyses of ROC curves was the cut-off point with the best combination of sensitivity and specificity and a good surrogate for FEV1/FVC <70%. Prevalence of airway obstruction was 17.7% when using FEV1/FEV6 <75% and 14.1% with FEV1/FVC <70%. Rosa et al found that FEV1/FEV6 <75% showed 89.0% sensitivity, 95.4% specificity, 85.2% PPV, and 96.7% NPV in pre-bronchodilator curves, results that were similar to our research.28
A total of 620 (5.2%) false-positive values and 130 (6.2%) false-negative values were observed (Table 3). In the subgroup analysis, 130 false-negative cases showed a mean difference of FEV1/FVC and FEV1/FEV6, with a respective LLN of 4.4% (SD =2.0) and 11.4% (SD =2.1). They were classified as GOLD stages I and II because reduced end-expiratory flow and expiratory time >6 seconds might have occurred in the initial stage of airflow limitation (Table 4). A total of 620 false-positive cases showed a mean difference of FEV1/FVC and FEV1/FEV6 with a respective LLN of 4.8% (SD =2.9) and 6.8% (SD =2.8). This finding might have been due to different fixed cut-off values between FEV1/FVC <70% and FEV1/FEV6 <75%.
The main strength of our study was that we obtained results from a representative sample of noninstitutionalized civilians among a Korean population using a stratified, multiple-stage, clustered-probability design. However, our study also had several limitations. First, lung function data from prebronchodilator spirometric values might have inadvertently included asthma patients, and hence be skewed. Carrying out postbronchodilator spirometry in a large, nationwide sample from the Korean National Health and Nutritional Examination Survey is difficult. Second, the absence of data on smoking history, previously diagnosed diseases (eg, COPD, asthma, tuberculosis, and bronchiectasis) in our study could have resulted in abnormal values for airway obstruction. So our results for detecting of airway obstruction were not limited to COPD, asthma, or other obstructive disease. Third, there were no available data on FEV1/FEV6 LLN because a pulmonary reference equation for FEV6 for a Korean population is lacking. Hence, we could not obtain a cut-off value of FEV6 in place of FVC for detecting restrictive pulmonary patterns. Finally, the fixed cut-off value of FEV1/FEV6 <75% should be verified with handheld spirometric devices with good repeatability, as in other studies,18 and not only with office spirometry.
Conclusion
A fixed cut-off for FEV1/FEV6 as a good surrogate for FEV1/FVC for detecting airway obstruction was 75% in a Korean population. However, a fixed cut-off value of FEV1/FEV6 <75% should be used with caution in older individuals and in those with mild–moderate airflow obstruction.
Author contributions
Kyung Soo Chung contributed to the study design, analysis and interpretation of data, and writing of the manuscript. Ji Ye Jung, Moo Suk Park, Young Sam Kim, Se Kyu Kim, and Joon Chang contributed to the study design, analyses and interpretation of data, and critically revised the manuscript. Joo Han Song, contributed to the study design, analyses and interpretation of data, and writing of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Guirguis-Blake JM, Senger CA, Webber EM, Mularski RA, Whitlock EP. Screening for Chronic Obstructive Pulmonary Disease: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2016;315(13):1378–1393. | ||
Ferguson GT, Enright PL, Buist AS, Higgins MW. Office spirometry for lung health assessment in adults: a consensus statement from the National Lung Health Education Program. Respir Care. 2000;45(5):513–530. | ||
Han MK, Kim MG, Mardon R, et al. Spirometry utilization for COPD: how do we measure up? Chest. 2007;132(2):403–409. | ||
Chung K, Kim K, Jung J, et al. Patterns and determinants of COPD-related healthcare utilization by severity of airway obstruction in Korea. BMC Pulm Med. 2014;14:27. | ||
Bellia V, Sorino C, Catalano F, et al. Validation of FEV6 in the elderly: correlates of performance and repeatability. Thorax. 2008;63(1):60–66. | ||
Jing JY, Huang TC, Cui W, Xu F, Shen HH. Should FEV1/FEV6 replace FEV1/FVC ratio to detect airway obstruction? A metaanalysis. Chest. 2009;135(4):991–998. | ||
Crapo RO. The role of FEV6 in the detection of airway obstruction. Respir Med. 2005;99(11):1467. | ||
Demir T. Response: Utilization of FEV6 in place of FVC may lead to underestimation of mild airway obstruction. Respir Med. 2005;99(12):1617. | ||
Perez-Padilla R, Wehrmeister FC, Celli BR, et al. Reliability of FEV1/FEV6 to diagnose airflow obstruction compared with FEV1/FVC: the PLATINO longitudinal study. PLoS One. 2013;8(8):e67960. | ||
Onishi K, Yoshimoto D, Hagan GW, Jones PW. Prevalence of airflow limitation in outpatients with cardiovascular diseases in Japan. Int J Chron Obstruct Pulmon Dis. 2014;9:563–568. | ||
Vandevoorde J, Verbanck S, Schuermans D, Kartounian J, Vincken W. Obstructive and restrictive spirometric patterns: fixed cut-offs for FEV1/FEV6 and FEV6. Eur Respir J. 2006;27(2):378–383. | ||
Aghili R, Kia M, Meysamie A, Aghili SM, Paknejad O. Fixed Cut-Off for FEV1/FEV6 and FEV6 in Detection of Obstructive and Restrictive Patterns. Iran Red Crescent Med J. 2013;15(2):152–156. | ||
Bhatt SP, Kim YI, Wells JM, et al. FEV(1)/FEV(6) to diagnose airflow obstruction. Comparisons with computed tomography and morbidity indices. Ann Am Thorac Soc. 2014;11(3):335–341. | ||
Pedersen OF. FEV6: a shortcut in spirometry? Eur Respir J. 2006;27(2):245–247. | ||
Akpinar-Elci M, Fedan KB, Enright PL. FEV6 as a surrogate for FVC in detecting airways obstruction and restriction in the workplace. Eur Respir J. 2006;27(2):374–377. | ||
Melbye H, Medbo A, Crockett A. The FEV1/FEV6 ratio is a good substitute for the FEV1/FVC ratio in the elderly. Prim Care Respir J. 2006;15(5):294–298. | ||
Vandevoorde J, Verbanck S, Schuermans D, Kartounian J, Vincken W. FEV1/FEV6 and FEV6 as an alternative for FEV1/FVC and FVC in the spirometric detection of airway obstruction and restriction. Chest. 2005;127(5):1560–1564. | ||
van den Bemt L, Wouters BC, Grootens J, Denis J, Poels PJ, Schermer TR. Diagnostic accuracy of pre-bronchodilator FEV1/FEV6 from microspirometry to detect airflow obstruction in primary care: a randomised cross-sectional study. NPJ Prim Care Respir Med. 2014;24:14033. | ||
Ferguson GT, Enright PL, Buist AS, Higgins MW. Office spirometry for lung health assessment in adults: A consensus statement from the National Lung Health Education Program. Chest. 2000;117(4):1146–1161. | ||
Soares AL, Rodrigues SC, Pereira CA. Limitação ao fluxo aéreo em brasileiros daraça branca: VEF1/VEF6 vs. VEF1/CVF*. [Airflow limitation in Brazilian Caucasians: FEV1/FEV6 vs. FEV1/FVC]. J Bras Pneumol. 2008;34(7):468–472. Portuguese. | ||
Morris ZQ, Huda N, Burke RR. The diagnostic importance of a reduced FEV1/FEV6. COPD. 2012;9(1):22–28. | ||
Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. | ||
Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948–968. | ||
Vestbo J, Hurd SS, Agusti AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365. | ||
Quanjer PH, Stanojevic S, Cole TJ, et al. Multi-ethnic reference values for spirometry for the 3-96-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40(6):1324–1343. | ||
Kim SH, Lee YD, Lee JY, Cho Y, Na DJ, Han MS. The Role of FEV6 in the Diagnosis of Obstructive Airway Disease for the Old Age. J Korean Geriatr Soc. 2006;10(3):167–171. | ||
COPD guideline revised 2012. Korean Academy of Tuberculosis and Respiratory Diseases. Available from: https://www.lungkorea.org/thesis/file/chronic_obstructive_pulmonary_disease_2014.pdf. Accessed August 5, 2016. | ||
Rosa FW, Perez-Padilla R, Camelier A, et al. Efficacy of the FEV1/FEV6 ratio compared to the FEV1/FVC ratio for the diagnosis of airway obstruction in subjects aged 40 years or over. Braz J Med Biol Res. 2007;40(12):1615–1621. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.