Back to Journals » Journal of Pain Research » Volume 11
Cryoneurolysis for the treatment of cervical facet joint syndrome: a technical note
Authors Wolter T, Kleinmann B, Knoeller S
Received 29 December 2017
Accepted for publication 3 April 2018
Published 19 June 2018 Volume 2018:11 Pages 1165—1169
DOI https://doi.org/10.2147/JPR.S161053
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Katherine Hanlon
Tilman Wolter,1 Barbara Kleinmann,1 Stefan Knoeller2,3
1Interdisciplinary Pain Center, 2Department of Orthopedics and Trauma Surgery, Medical Center–University of Freiburg, Faculty of Medicine, University of Freiburg, Freiburg, Germany; 3Department of Spine Surgery, Helios Klinik Breisach, Breisach, Germany
Objective: Neck pain has an annual prevalence of 30%. A frequent cause of neck pain is cervical facet joint pain. In cases of refractory cervical facet joint pain, radiofrequency can be employed, but the grade of evidence attested in systematic reviews is fair. Cryoneurolysis has been reported to induce favorable outcomes in lumbar facet joint pain. We sought to examine the feasibility of cervical facet joint cryoneurolysis.
Setting: Tertiary academic pain center.
Patients and methods: We report here the operative technique of cervical facet joint cryoneurolysis for patients with cervical facet joint pain. The procedure is performed under CT-guidance. The lesion points are defined with the help of sensory stimulation.
Results: Six cervical facet joint denervations were carried out in five patients. All patients had an uneventful course with adequate pain relief. Apart from soreness of the paravertebral muscles no severe side effects were encountered.
Conclusion: This is the first report of cryoneurolysis for the treatment of cervical facet joint pain. The technique is feasible and warrants further studies.
Keywords: neck pain, facet joint pain, cervical spine, cryoneurolysis
Introduction
Neck pain has an annual prevalence of 30%.1 It is a very common pain syndrome with 50% of patients proceeding to chronic pain.1 Neck pain can be insidious in onset or traumatic. A frequent cause of neck pain is cervical facet joint pain, accounting for approximately 55% of cases.2 The diagnosis of cervical facet joint pain is usually based on the clinical analysis and the outcome of diagnostic cervical facet joint blocks.3 One might try to augment the pain relieving effect of cervical facet joint blocks by the additional application of steroids, but there is no scientific evidence that steroids provide long-term pain relief compared to local anesthetic only.4
Lord et al introduced radiofrequency for neurotomy of the cervical facet joint nerves.5 The rationale of neurotomy of the facet joints is to disrupt the nerval supply of the facet joint in order to achieve pain relief. This technique had been used previously in the treatment of lumbar facet joint syndromes. Since Lord et al’s study, the outcome of radiofrequency for cervical facet joint pain has been described in several observational papers. A recent systematic review quoted one randomized controlled trial (RCT)5 and five observational studies6–10 on cervical radiofrequency treatment11 and found level II evidence. In another systematic review the grade of evidence attested was fair,4 while another systematic review found evidence of effectiveness of high quality according to the GRADE system.12
In lumbar facet joint syndromes, radiofrequency has been studied in a large number of observational studies and nine RCTs.13–21 Regarding the studies on lumbar radiofrequency, a considerable inconsistency is stated. While an early prospective study found that after 12 months 87% of the patients had at least 60% pain relief,22 one RCT found that radiofrequency was not better than placebo.14 Apart from differences in patient selection, differences in application of the technique have also been discussed.23,24
In lumbar facet joint syndromes, cryoneurolysis has been described as an alternative to radio-frequency in several observational studies but not yet in RCTs.25–30 The technical advantages of cryoneurolysis are the bigger size and the spherical shape of the lesion which increases the probability that the target nerve is struck and which makes a tangential approach to the nerve unnecessary. Strikingly, the results of the studies on cryoneurolysis are relatively uniform. All studies showed an average decrease of the pain intensity of approximately 50%, which lasted for more than 1 year. We sought to examine whether the cryoneurolysis technique is also feasible for cervical facet joint treatment. We describe here the technique of cervical cryoneurolysis under CT-guidance.
Patients and methods
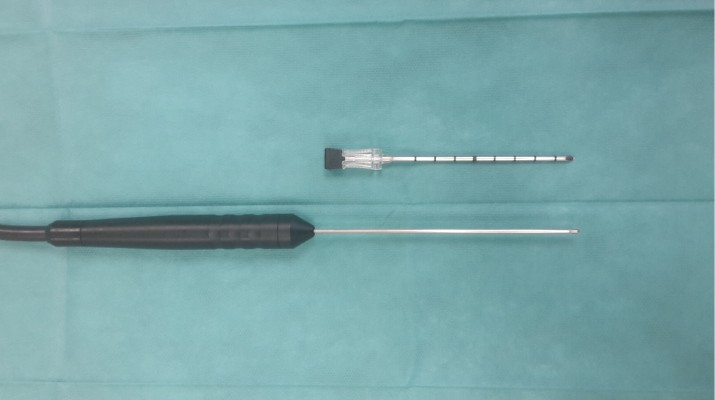
Cryoneurolysis for facet joint pain aims at producing a second degree nerve injury (axonotmesis) to the nerves supplying the facet joint by applying a temperature of –60°C up to –70°C. The target joint is determined clinically according to the clinical presentation.3,31 Patients undergo at least two diagnostic blocks with positive results before cryoneurolysis is indicated. In the present study intraarticular blocks were performed, but future studies should use controlled medial branch blocks for patient selection. Cryoneurolysis is performed with the C3 Cryoneurolysis device (Inomed®, Emmendingen, Germany) which operates with CO2. Patients are placed in the prone position. With CT, a target point is identified which is located at the superior margins of the facet joint capsule. A trajectory is then calculated (Figure 1). The entry point is marked on the skin. After placement of sterile drapes and skin disinfection with disinfectant scrubs, local anesthesia is performed with up to 5 mL mepivacaine 2% (AstraZeneca GmbH, Wedel, Germany) at the calculated entry point. A little skin incision is made with a 11-blade scalpel. Then, the 12 g needle (Figure 2) is advanced along the calculated trajectory toward the target point. The target point is chosen at the lower margins of the upper portion of the facet joint. A CT scan is performed to verify the correct position of the needle (Figure 3). To minimize tissue damage, the needle is not advanced directly to the bony surface but only up to a distance of 1 cm from the bone (Figure 3). If the needle position is correct on the dorsal lateral portion of the facet joint, the cryoprobe is advanced into the needle and the needle is drawn back for 1 cm. If the needle position is not correct, the direction of the needle is changed and the new position of the needle is verified by a second CT scan. When the correct position of the needle is assured, the cryoprobe is introduced. The cryoprobe is held by hand throughout the whole procedure which is easily possible as the cryoneurolysis device can be operated by means of a foot pedal. At this stage it is important to have bony contact with the cryoprobe. From the first target point, the cryoprobe is slowly directed approximately 5 mm cranially. Once the cryoprobe is in this position, sensory stimulation with slowly increasing voltages is performed. When the patient feels the typical pain, motor stimulation is performed. If this does not lead to a motoric response, cryoneurolysis is started. The duration of freezing is 2.5 minutes at each target point (Figure 4). After freezing, stimulation is performed to see if the point is entirely denervated. If the patient can still feel pain another freezing cycle is performed for 2.5 minutes and the patient retested (Figures 4 and 5). The tip of the needle is then moved caudally to a point approximately 5 mm caudal from the initial target point (blue dot in Figure 4) and a further stimulation is performed. If the patient is able to feel the stimulation, cryoneurolysis is performed once again as described above. In this manner usually two points are cryoneurolyzed until no more pain can be elicited by stimulation. Usually patients report an increasing pain during the first minute of the freezing cycle which then abruptly stops.
  | Figure 1 Assignment of the target point of the probe under CT-guidance. |
  | Figure 2 A 12 g needle and cryoprobe. |
  | Figure 3 CT scan of the 12 g needle prior to manual introduction of the cryoprobe. |
  | Figure 4 Target points for first needle positioning and lesion points. Note: Blue dot, target point in CT; red dot, point of lesioning after sensory stimulation. |
  | Figure 5 Schematic lateral view of first probe position (continuous line) and final probe position after stimulation (dotted lines). |
After the procedure, tape dressings are used which can be removed after two days. The patients usually remain under observation for 2 to 3 hours. For post procedural soreness we recommend nonsteroidal anti-inflammatory drugs (NSAIDs). Physiotherapy should be started after 1 or 2 weeks.
All patients gave a written informed consent prior to the procedure. The present study was approved by the Ethics Committee of the University Hospital Freiburg (institutional review board [IRB] no.: 47/18).
Results
Up till now we have used the technique described above six times in five patients. In one case of bilateral pain in the same segment (C6/7) we cryolyzed the two facets on different days. All other patients had monolateral and monosegmental cryoneurolysis. Treated levels were C3/4, C4/5, C5/6 and C6/7. We encountered no severe side effects apart from soreness of the paravertebral muscles, which could last for a couple of days.
Discussion
The present report describes the application of the cryoneurolysis technique for cervical facet joint pain. The method described here has been employed in five patients without any significant adverse events. All patients have had an uneventful clinical course after the procedure and reported a distinct pain reduction. Thus, the feasibility of the method is demonstrated in this study.
To our best knowledge there are no previous reports about cryoneurolysis for the treatment of cervical facet joint pain. Cryoneurolysis for facet joint pain has been described in a number of studies regarding the lumbar spine.25–27,30 A recent study showed good efficacy of cryoneurolysis in the treatment of occipital neuralgia.32 Moreover, cryoneurolysis has been described for chest wall pain33,34 and several peripheral nerve pain syndromes.35
For both cervical as well as lumbar facet joints, radiofrequency has been employed with comparably good success. While to date lumbar cryoneurolysis has only been studied in observational studies, for radiofrequency of lumbar facet joints there are nine RCTs available.11 While some of these RCTs are controlled for the number of diagnostic blocks,18 additional steroid application,15 facet joint blocks19 or for the technique of needle-placement,20 four of these RCTs are placebo-controlled.13,14,16,17 These RCTs, however, display contradicting results. While some see radiofrequency treatment only as effective as placebo14 others have shown good13,16 or intermediate results.17 A recent study showed no significant difference 6 months following a lumbar radiofrequency or intraarticular steroid injection.21
The published results for lumbar cryoneurolysis, however, show a more uniform picture: in realistically selected clinical samples a bisection of the pain intensity lasting for at least 1 year on average was demonstrated.25–27,30
Cryoneurolysis has yielded favorable results in the treatment of lumbar facet joint pain in a number of observational studies.25–27,30 As there is still some inconsistency in the results of radiofrequency of the cervical facet joint syndrome, it is of interest to elucidate whether cryoneurolysis may be an alternative treatment.
Performing nerve lesions by means of freezing may eventually reduce the risk of neuroma formation. The risk of neuropathic pain secondary to the lesioning procedure might also be reduced. In a recent study on 64 patients who had undergone third occipital nerve radiofrequency, 12 patients (19%) recorded new pain secondary to the procedure, with seven of the 12 patients showing persistent symptoms for an average of 2.6 months.36 There are no studies to date reporting on the occurrence of neuropathic pain secondary to cryoneurolysis.
Some technical aspects need to be discussed. Performing cryoneurolysis in the way described in the “Patients and methods” section seems to be technically less challenging than radiofrequency, particularly in degenerated facets. The size of the lesion in cryoneurolysis is considerably bigger than in radiofrequency.37 Thus, the probability that the target nerve is struck by the lesion is increased. Moreover, due to the spherical shape of the lesion, a tangential approach to the nerve is not necessary. On the other hand, the probe and the needle in cryoneurolysis are considerably bigger than in radiofrequency (12 g vs 21 g), inducing more tissue damage in the paraspinal musculature. Our first experience with this technique, however, showed that the muscle tenderness induced by the procedure resolves within a couple of days. We do not expect that the tissue damage in the paraspinal musculature has a big impact on the patients in the long run. The direction of movement of the tissue probe during the procedure is along the fiber direction of the muscles. The amount of tissue damage, moreover, is a lot less than that caused by a dorsal cervical foraminotomy (Frykholm operation) for example, which is usually tolerated very well by patients. In our opinion, for the choice of the lesion method, the practical feasibility and the probability of accomplishing the objective of the procedure, thus lesioning the target nerve, are more important than the amount of reversible tissue damage.
Further studies are necessary to define whether cryoneurolysis will have a place in the treatment of cervical facet joint pain in the future. These studies should be performed based on patient and joint selection through controlled diagnostic medial branch blocks. They should also imply acquisition of data on the radiation dose and, if applicable, on the amount of tissue damage. We plan to perform a prospective study on this technique and, depending on the results of this study, a non-inferiority study comparing the cryoneurolysis technique with cervical medial branch radiofrequency neurotomy will be performed.
Acknowledgment
The article processing charge was funded by the German Research Foundation (Deutsche Forschungsgemeinschaft [DFG]) and the University of Freiburg in the funding program “Open Access Publishing”.
Disclosure
The authors report no conflicts of interest in this work.
References
Cohen SP. Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin Proc. 2015;90(2):284–299. | ||
Yin W, Bogduk N. The nature of neck pain in a private pain clinic in the United States. Pain Med. 2008;9(2):196–203. | ||
Dwyer A, Aprill C, Bogduk N. Cervical zygapophyseal joint pain patterns. I: A study in normal volunteers. Spine (Phila Pa 1976). 1990;15(6):453–457. | ||
Falco FJ, Manchikanti L, Datta S, et al. Systematic review of the therapeutic effectiveness of cervical facet joint interventions: an update. Pain Physician. 2012;15(6):E839–E868. | ||
Lord SM, Barnsley L, Wallis BJ, McDonald GJ, Bogduk N. Percutaneous radio-frequency neurotomy for chronic cervical zygapophyseal-joint pain. N Engl J Med. 1996;335(23):1721–1726. | ||
Sapir DA, Gorup JM. Radiofrequency medial branch neurotomy in litigant and nonlitigant patients with cervical whiplash: a prospective study. Spine (Phila Pa 1976). 2001;26(12):E268–E273. | ||
Govind J, King W, Bailey B, Bogduk N. Radiofrequency neurotomy for the treatment of third occipital headache. J Neurol Neurosurg Psychiatry. 2003;74(1):88–93. | ||
Cohen SP, Bajwa ZH, Kraemer JJ, et al. Factors predicting success and failure for cervical facet radiofrequency denervation: a multi-center analysis. Reg Anesth Pain Med. 2007;32(6):495–503. | ||
Speldewinde GC. Outcomes of percutaneous zygapophysial and sacroiliac joint neurotomy in a community setting. Pain Med. 2011;12(2):209–218. | ||
MacVicar J, Borowczyk JM, MacVicar AM, Loughnan BM, Bogduk N. Cervical medial branch radiofrequency neurotomy in New Zealand. Pain Med. 2012;13(5):647–654. | ||
Manchikanti L, Kaye AD, Boswell MV, et al. A systematic review and best evidence synthesis of the effectiveness of therapeutic facet joint interventions in managing chronic spinal pain. Pain Physician. 2015;18(4):E535–E582. | ||
Engel A, Rappard G, King W, Kennedy DJ. Standards Division of the International Spine Intervention Society. The effectiveness and risks of fluoroscopically-guided cervical medial branch thermal radiofrequency neurotomy: A systematic review with comprehensive analysis of the published data. Pain Med. 2016;17(4):658–669. | ||
van Kleef M, Barendse GA, Kessels A, Voets HM, Weber WE, de Lange S. Randomized trial of radiofrequency lumbar facet denervation for chronic low back pain. Spine (Phila Pa 1976). 1999;24(18):1937–1942. | ||
van Wijk RM, Geurts JW, Wynne HJ, et al. Radiofrequency denervation of lumbar facet joints in the treatment of chronic low back pain: a randomized, double-blind, sham lesion-controlled trial. Clin J Pain. 2005;21(4):335–344. | ||
Dobrogowski J, Wrzosek A, Wordliczek J. Radiofrequency denervation with or without addition of pentoxifylline or methylprednisolone for chronic lumbar zygapophysial joint pain. Pharmacol Rep. 2005;57(4):475–480. | ||
Tekin I, Mirzai H, Ok G, Erbuyun K, Vatansever D. A comparison of conventional and pulsed radiofrequency denervation in the treatment of chronic facet joint pain. Clin J Pain. 2007;23(6):524–529. | ||
Nath S, Nath CA, Pettersson K. Percutaneous lumbar zygapophysial (Facet) joint neurotomy using radiofrequency current, in the management of chronic low back pain: a randomized double-blind trial. Spine (Phila Pa 1976). 2008;33(12):1291–1297; discussion 1298. | ||
Cohen SP, Williams KA, Kurihara C, et al. Multicenter, randomized, comparative cost-effectiveness study comparing 0, 1, and 2 diagnostic medial branch (facet joint nerve) block treatment paradigms before lumbar facet radiofrequency denervation. Anesthesiology. 2010;113(2):395–405. | ||
Civelek E, Cansever T, Kabatas S, et al. Comparison of effectiveness of facet joint injection and radiofrequency denervation in chronic low back pain. Turk Neurosurg. 2012;22(2):200–206. | ||
Moon JY, Lee PB, Kim YC, Choi SP, Sim WS. An alternative distal approach for the lumbar medial branch radiofrequency denervation: a prospective randomized comparative study. Anesth Analg. 2013;116(5):1133–1140. | ||
Lakemeier S, Lind M, Schultz W, et al. A comparison of intraarticular lumbar facet joint steroid injections and lumbar facet joint radiofrequency denervation in the treatment of low back pain: a randomized, controlled, double-blind trial. Anesth Analg. 2013;117(1):228–235. | ||
Dreyfuss P, Halbrook B, Pauza K, Joshi A, McLarty J, Bogduk N. Efficacy and validity of radiofrequency neurotomy for chronic lumbar zygapophysial joint pain. Spine (Phila Pa 1976). 2000;25(10):1270–1277. | ||
Bogduk N. Lumbar radiofrequency neurotomy. Clin J Pain. 2006;22(4):409. | ||
Datta S, Lee M, Falco FJ, Bryce DA, Hayek SM. Systematic assessment of diagnostic accuracy and therapeutic utility of lumbar facet joint interventions. Pain Physician. 2009;12(2):437–460. | ||
Barlocher CB, Krauss JK, Seiler RW. Kryorhizotomy: an alternative technique for lumbar medial branch rhizotomy in lumbar facet syndrome. J Neurosurg. 2003;98(1 Suppl):14–20. | ||
Staender M, Maerz U, Tonn JC, Steude U. Computerized tomography-guided kryorhizotomy in 76 patients with lumbar facet joint syndrome. J Neurosurg Spine. 2005;3(6):444–449. | ||
Birkenmaier C, Veihelmann A, Trouillier H, et al. Percutaneous cryodenervation of lumbar facet joints: a prospective clinical trial. Int Orthop. 2007;31(4):525–530. | ||
Birkenmaier C, Veihelmann A, Trouillier HH, Hausdorf J, von Schulze Pellengahr C. Medial branch blocks versus pericapsular blocks in selecting patients for percutaneous cryodenervation of lumbar facet joints. Reg Anesth Pain Med. 2007;32(1):27–33. | ||
Andres RH, Graupner T, Barlocher CB, Augsburger A, Fandino J. Laser-guided lumbar medial branch kryorhizotomy. J Neurosurg Spine. 2010;13(3):341–345. | ||
Wolter T, Deininger M, Hubbe U, Mohadjer M, Knoeller S. Cryoneurolysis for zygapophyseal joint pain: a retrospective analysis of 117 interventions. Acta Neurochir (Wien). 2011;153(5):1011–1019. | ||
Aprill C, Dwyer A, Bogduk N. Cervical zygapophyseal joint pain patterns. II: A clinical evaluation. Spine (Phila Pa 1976). 1990;15(6):458–461. | ||
Kastler A, Attye A, Maindet C, et al. Greater occipital nerve cryoneurolysis in the management of intractable occipital neuralgia. J Neuroradiol. Epub 2017 Dec 19. | ||
Green CR, de Rosayro AM, Tait AR. The role of cryoanalgesia for chronic thoracic pain: results of a long-term follow up. J Natl Med Assoc. 2002;94(8):716–720. | ||
Moore W, Kolnick D, Tan J, Yu HS. CT guided percutaneous cryoneurolysis for post thoracotomy pain syndrome: early experience and effectiveness. Acad Radiol. 2010;17(5):603–606. | ||
Trescot AM. Cryoanalgesia in interventional pain management. Pain Physician. 2003;6(3):345–360. | ||
Gazelka HM, Knievel S, Mauck WD, et al. Incidence of neuropathic pain after radiofrequency denervation of the third occipital nerve. J Pain Res. 2014;7:195–198. | ||
Mattmüller R. Radiofrequenzläsion und Kryoläsion [Radiofrequency lesion and cryolysis]. In: Hankemeier U, Hildebrandt J, eds. Neurodestruktive Verfahren in der Schmerztherapie [Neuro Procedures in Pain Therapy]. 2nd ed. Berlin Heidelberg New York: Springer; 2002:19–32. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
