Back to Journals » Journal of Pain Research » Volume 10
Cross-cultural adaptation of the German Pain Solutions Questionnaire: an instrument to measure assimilative and accommodative coping in response to chronic pain
Authors Sielski R, Glombiewski JA, Rief W , Crombez G, Barke A
Received 12 December 2016
Accepted for publication 22 February 2017
Published 19 June 2017 Volume 2017:10 Pages 1437—1446
DOI https://doi.org/10.2147/JPR.S130016
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor E Alfonso Romero-Sandoval
Robert Sielski,1 Julia Anna Glombiewski,1 Winfried Rief,1 Geert Crombez,2 Antonia Barke1
1Department for Clinical Psychology and Psychotherapy, Philipps-University of Marburg, Marburg, Germany; 2Faculty of Psychology and Educational Sciences, Ghent University, Ghent, Belgium
Abstract: According to the dual process model of coping, assimilative or accommodative strategies can be applied to deal with aversive life situations. In people with chronic pain, the tenacious focus on achieving analgesia is often referred to as assimilative coping and associated with more disability and catastrophic thinking. In contrast, accommodative coping (accepting one’s pain and setting new goals) appears to have beneficial effects. To assess how people with chronic pain use these different coping strategies, questionnaires measuring these concepts are needed. Following international guidelines, a German version of the Pain Solutions Questionnaire (PaSol) was prepared. A sample of 165 participants with chronic low back pain (CLBP; 60% women; age 53 ± 8.4 years) filled in the questionnaire and measures for pain-related disability, affective distress, catastrophic thinking, and attention to pain. Item analyses, an exploratory factor analysis, and correlations with pain-related measures were calculated. In addition, data from 98 participants who received psychological treatment were examined to investigate the PaSol’s sensitivity to change. The exploratory factor analysis reproduced the original questionnaire’s four-factor structure. Internal consistencies for the subscales ranged from Cronbach’s α=0.72 to α=0.84. Mean item difficulties for the subscales ranged from pi=0.62 to pi=0.79. The highest correlations were found for Meaningfulness with catastrophic thinking (r=−0.58) and affective distress (r=−0.36). The PaSol subscale Meaningfulness predicted pain-related disability; the subscales Meaningfulness and Solving Pain predicted affective distress. Furthermore, the PaSol was found to be sensitive to detect changes over time. The German version of the PaSol is a reliable and valid instrument in the measurement of assimilative and accommodative coping strategies in people suffering from CLBP. It may provide a useful tool when examining temporal dynamics of the changing coping strategies in the transition from acute to chronic pain as well as during pain treatments.
Keywords: acceptance, back pain, coping, problem-solving, German, validation
Background
Coping with chronic pain is a challenge for patients and health care providers. Patients suffering from chronic low back pain (CLBP) often express the wish for pain relief when beginning a new treatment. Most CLBP patients have tried several interventions to cure their pain or get more control over it.1 The search for full recovery can involve great effort; despite this effort, the majority of attempts remain unsuccessful.2–4 Repeated failures in controlling pain can lead to less pain tolerance, more worry, and fear or catastrophic thinking, thus opening up new areas of concern.5–7
A very useful model in this context is the dual process model of coping by Brandtstädter and Renner.8 In this model, the authors distinguish two coping processes that can be activated when people are confronted with adverse life situations such as persistent pain. They call the tenacious search for a solution “assimilative coping”. Assimilative coping is often the first way of dealing with problems and can be successful if goal attainment is realistic and controllable. Regarding chronic pain, assimilative coping can mean focusing on achieving analgesia, such as through bed rest or taking (more) medication.9 If repeated attempts at achieving pain relief fail, patients with chronic pain tend to intensify their efforts: often, they narrow their focus on, and increase the importance of, the goal of pain relief, rather than accepting the pain. As the probability of reaching the goal of a pain-free life is very low and achievement of this goal is not in the person’s control, the tenacity invested in further attempts can lead to adverse consequences in the long term.10–12 Therefore, it may be more advantageous to change the coping strategy from assimilative to accommodative coping. “Accommodative coping” means flexibly adjusting the goal when the initial goal cannot be reached, possibly aiming at a new goal. For patients with chronic pain, this can mean relinquishing the goal of pain relief and setting new and realistic goals for a more satisfying life despite the pain. Acceptance of the insolubility of chronic pain has been found to be associated with lower reports of pain, less depression, and less disability.13,14 However, the disengagement from pain is difficult, especially in the presence of catastrophic thinking and hypervigilance, which are often consequences of unsuccessful assimilative coping.15–17
On the basis of the dual process model, the Pain Solutions Questionnaire (PaSol)18 was developed to assess how people construct problems and seek solutions with regard to pain. In contrast to other instruments, the PaSol captures both the assimilative and accommodative ways of coping from an action-oriented and goal-dependent perspective. The PaSol is a 14-item instrument that aims at measuring different attitudes to solving the problem of pain by using four subscales. The subscales Problem-Solving (ie, I try everything to get rid of my pain) and Belief in a Solution (ie, I am convinced that there is a treatment for my pain) represent the assimilative approach to deal with pain, whereas the subscales Acceptance of the Insolubility of Pain (ie, I can accept that I can’t control my pain) and Meaningfulness of Life Despite Pain (ie, I try to live with my pain) target accommodative coping. The item construction aimed at ensuring that the problem-solving attitudes were particularly related to pain, both acute and chronic situations, were presented, and potential outcome and process measures (ie, disability and attention) were kept separate. To create the items, items from the Tenacious Goal Pursuit and Flexible Goal Adjustment scale,8 the Dutch version of the Chronic Pain Acceptance Questionnaire (CPAQ),19 and the Illness Cognition Questionnaire (ICQ)20 were inspected and, if they appeared useful within the context of the dual process model, adapted for the purpose at hand. The resulting scale was shown to have good reliability and validity. Cronbach’s a coefficients for the subscales of the original scale range from a=0.77 to a=0.86.7,18 According to a content analysis of instruments that measure the construct of acceptance, Lauwerier et al21 found the PaSol to be the only questionnaire besides the CPAQ that includes items on all relevant scales of acceptance (ie, disengagement from pain control, pain willingness, and engagement in activities other than pain control). Furthermore, assimilative coping as measured with the PaSol was shown to be related to disability, affective distress, attention to pain, and catastrophic thinking, and it explained unique variance in the prediction of medication overuse headache.7,18,22 To date, there is little research about assimilative and accommodative coping and its consequences for the specific group of patients suffering from CLBP.
To sum up, despite indications that accommodative coping may have beneficial effects, research in this area and validated instruments for the assessment of these coping strategies are sparse. The purpose of the current study was to investigate the psychometric properties of the German adaptation of the PaSol in a CLBP sample and to provide further information about the factor structure and concurrent validity. In addition, we aimed at assessing whether the PaSol is sensitive to changes through a psychotherapeutic intervention.
Methods
Translation and cross-cultural adaptation
Permission to translate and validate the PaSol (English version of the study by De Vlieger et al18) was obtained from the original authors. The translation and cross-cultural adaptation process followed the guidelines of Beaton et al.23 Prior to assessment, the pre-final version was given to a group of five CLBP patients. They filled in this version of the PaSol and provided general feedback about the questionnaire. Furthermore, they were interviewed about potential difficulties in understanding the items. Their remarks indicated that all items were clear and understandable and no further changes to the translation were made as a result. The pre-final German and the back-translated versions of the questionnaire were also sent to the original authors of the PaSol, who approved the changes that were made. The German version can be downloaded here: (https://doi.org/10.5281/zenodo.801502).
Participants
The study sample consisted of 165 patients suffering from CLBP (defined as back pain persisting for more than 3 months).24 The patients were recruited from an outpatient clinic (Psychotherapy Outpatient Clinic Marburg, Germany) as well as from an inpatient rehabilitation center (MediClin Klinik am Hahnberg, Germany). All patients (n=98) from the outpatient clinic received a psychotherapeutic treatment (exposure treatment or cognitive-behavioral therapy [CBT]) for 10–15 sessions. The CBT consisted of psychoeducation regarding pain, graded activity, relaxation training, and different cognitive interventions such as attention shifting. The exposure treatment consisted of psychoeducation regarding pain, a fear hierarchy, and several exposure sessions.25 For these patients, data before therapy and upon its completion are available, allowing the assessment of the questionnaire’s sensitivity to change. All participants provided informed consent to participate, and the study was approved by the Ethics Committee of the Department of Psychology, Philipps-University Marburg, Germany.
Instruments
Attitudes to solving the problem of pain
The PaSol consists of 14 items rated on a 7-point Likert scale, ranging from 0 (not at all applicable) to 6 (highly applicable). In the original, the items are subdivided into four interrelated scales: 1) Solving Pain Scale (four items), 2) Meaningfulness of Life Despite Pain Scale (five items), 3) Acceptance of the Insolubility of Pain Scale (three items), and 4) Belief in a Solution Scale (two items). The subscales (2) Meaningfulness of Life Despite Pain and (3) Acceptance of the Insolubility of Pain assess an accommodative way of coping with pain, whereas the subscales (1) Solving Pain and (4) Belief in a Solution capture assimilative coping.
Pain intensity
Average pain intensity over the last 4 weeks was assessed using an 11-point Numeric Rating Scale (NRS) from 0 (no pain) to 10 (pain at its worst) from the German Pain Questionnaire (German Pain Questionnaire [Deutscher Schmerzfragebogen], DSF).26
Pain-related disability
The German version of the Pain Disability Index (PDI)27,28 was used to measure pain-related disability. The PDI is a seven-item scale assessing the degree to which people experience interference in seven areas of daily life (family/home responsibilities, recreation, social activity, occupation, sexual behavior, self-care, basic life activities) caused by their pain. Each area of activity is rated on an 11-point scale ranging from 0 (no disability) to 10 (total disability), with higher scores indicating higher pain-related disability. The PDI has very good reliability and validity.29
Attention to pain
The Pain Vigilance and Awareness Questionnaire (PVAQ)30 was used to measure attention to pain. The PVAQ consists of 16 items ranging from 0 (never) to 5 (always) and assesses. awareness, consciousness, and vigilance regarding pain over the last 2 weeks. The PVAQ has shown to be a reliable and valid instrument.31
Affective distress
The German version of the Hospital Anxiety and Depression Scale (HADS)32,33 was used for identifying affective distress. The scale assesses depressive and anxious symptoms in the last 7 days. The HADS consists of two subscales (Depression, Anxiety) with seven items each. Items are answered on a 4-point scale with item-specific response categories. Both scales have a scoring range of 0–21. The total score of the HADS can also be used as an index of general affective distress. The reliability and validity have shown to be acceptable.34
Catastrophic thinking
The German version of the Pain Catastrophizing Scale (PCS)35,36 was used for the assessment of catastrophic thinking about pain. The PCS is a 13-item self-report instrument measuring pain-related catastrophizing on three subscales: Rumination, Magnification, and Helplessness. Items are answered on a 5-point Likert scale from 0 (not at all) to 4 (all the time). The total score ranges from 0 to 52, with higher scores indicating higher levels of catastrophic thinking. Psychometric properties for the PCS have shown to be excellent.37
Statistical analysis
First, item analyses were performed to calculate mean item scores and standard deviation (SD), item difficulties,38 and corrected item–total correlations for each item. Furthermore, mean inter-item correlations, mean item difficulty, and internal consistency (standardized Cronbach’s a) were determined for each subscale separately.
To analyze the factor structure of the PaSol, we decided to conduct an exploratory factor analysis. The Kaiser–Meyer–Olkin test of sampling adequacy and Bartlett’s test of sphericity were conducted to determine whether the data were appropriate for factor analysis. On theoretical grounds (to keep in line with the original questionnaire), we decided to extract four factors. For the extraction, we used the maximum likelihood method and rotated the extracted factors orthogonally (varimax).
To analyze the concurrent validity, Pearson correlations between the scores of the PaSol subscales and related constructs (pain-related disability, attention to pain, affective distress, catastrophic thinking) were calculated. For sex and PaSol subscales, point biserial correlation coefficients were computed. Sex differences for age, average pain intensity, average pain quality, pain duration, PDI, and PaSol subscales were analyzed with independent t-tests.
To test for the unique contribution of the PaSol subscales in accounting for the variability in disability (PDI, criterion) and affective distress (HADS, criterion), hierarchical multiple regression analyses with blockwise forced entry were computed. In the first block, age, sex, and pain measures, ie, pain intensity, pain quality, and pain duration, were entered as predictor variables; in the second block, the subscales of the PaSol were entered to assess whether they explain an additional increment. Multicollinearity was assessed according to the recommendations of Menard39 suggesting that tolerance values below 0.20 should be of concern.
To test whether the questionnaire is sensitive to changes following a psychotherapeutic intervention, patients who had received treatment were divided into two groups: patients whose PDI scores had improved by at least 30% after the treatment and patients whose scores had not performed so.40 With the resulting groups, 2×2 mixed design analyses of variance with the between-subjects factor improvement (yes/no) and the within-subject factor time (pre-/post-treatment) and the PaSol subscales as dependent variables were conducted. Honest significant difference (HSD) post hoc tests for unequal group size were used to analyze interaction effects further. As measures of effect size, Cohen’s d and h2 were reported.41 The data were analyzed using Statistica version 10 (Statsoft Inc., Tulsa, OK, USA) and SPSS Statistics 22.42
Results
Study sample
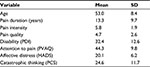
Data from a total of 165 patients (inpatient and outpatient sample; 60% female) were used to analyze the factor structure, construct validity, internal consistency, and item properties. Descriptive statistics for the samples are shown in Table 1. Regarding demographic and pain-related variables, ie, age, duration of pain, disability, and pain intensity, the current study sample is comparable to other populations of CLBP patients as well as to the study sample of the original validation of the PaSol.18,43
Missing data and normality of score distribution
Regarding the PaSol, 0.04% of values were missing. The maximum of missing answers was one (item 3: I try to live with my pain). According to the Kolmogorov–Smirnov test, all items were non-normally distributed (all p-values <0.05); however, no item exceeded the critical values for kurtosis (>2) or skewness (>7), and no participant obtained the minimum (0) or maximum (84) possible scores.
Item analyses and internal consistency
Standard item analyses were performed. The item difficulties, which in the context of attitude measurement show the extent to which the items are endorsed by the respondents (lower values indicate less agreement with the item), lay between pi=0.35 (item 9) and pi=0.83 (item 12). For the subscales, mean item difficulties were as follows: Solving Pain: pi=0.79; Meaningfulness of Life Despite Pain: pi=0.64; Acceptance of the Insolubility of Pain: pi=0.40; Belief in a Solution: pi=0.62. In the context of attitude measurement, item difficulties between 0.20 and 0.80 are considered desirable, as medium difficulties better differentiate between respondents and are of higher diagnostic value.44
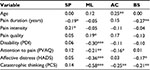
The internal consistencies for the subscales showed Cronbach’s a values of 0.72 (Problem-Solving), 0.75 (Belief in a Solution), 0.81 (Meaningfulness), and 0.84 (Acceptance). Removing any items did not substantially improve the internal consistency of the subscales. The item–total correlations ranged from ritc=0.02 (item 12) to ritc=0.62 (item 2). The subscale correlations ranged between r=−0.10 and r=0.36 (Table 2).
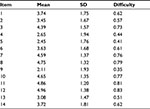  | Table 2 Item mean, SD, and item difficulties |
Validity
Factor structure
Bartlett’s test of sphericity was significant (c2=957.41, df=91, p<0.001), and the value of Kaiser–Meyer–Olkin measure was 0.75, indicating that the sample was adequate and the data were appropriate for factor analysis.
The exploratory factor analysis with the decision to extract four factors on theoretical grounds revealed a solution that reflected the original factors perfectly. The eigenvalues ranged between 1.45 and 2.50, accounting for 56.30% of the total variance, with a mean item communality of 0.56 (SD = 0.18). As items loaded on the same factors as reported in the original article, factor labels remained the same (Table 3).
Correlations with pain parameters and pain-related constructs
The highest correlations with pain-related outcomes and pain quality at baseline were found for the subscale Meaningfulness of Life Despite Pain and catastrophic thinking (r=−0.58, p<0.01): experiencing life as meaningful despite the pain is associated with lower levels of catastrophizing. The subscale Solving Pain only showed (small) significant correlations with pain parameters such as intensity (r=0.21, p<0.05) and pain duration (r=0.19, p<0.05): higher intensity and longer duration were linked to searching for a solution to the pain. The subscale Acceptance of the Insolubility of Pain correlated negatively with catastrophic thinking (r=−0.25, p<0.01) and attention to pain (r=−0.16, p<0.05): persons accepting the pain as unsolvable reported lower levels of catastrophizing thoughts and less attention to the pain. This was also the only PaSol subscale that seemed related to age (r=0.25, p<0.01). The subscale Belief in a Solution showed negative correlations with pain duration (r=−0.27, p<0.01), affective distress (r=−0.17, p<0.05), and catastrophic thinking (r=−0.21, p<0.01; Table 4).
Regression analyses for disability and distress
Two multiple hierarchical regression analyses with the criterion pain-related disability (PDI) and distress (HADS), respectively, were calculated to examine whether the PaSol subscales contributed uniquely to explaining their variance when controlling for age, sex, and pain characteristics. Assessment of multicollinearity revealed tolerances >0.85 and variance inflation factors (VIFs) <1.2, indicating that multicollinearity did not present a problem.
The analysis with pain-related disability as a dependent variable showed that no subscale of the PaSol was related to disability when controlling for demographic and pain characteristics (Table 5). Further analyses revealed that the subscale Meaningfulness was only related to less disability when pain duration was excluded from the analyses, and only age, sex, pain intensity, and pain quality were controlled for, indicating shared variance between pain duration and Meaningfulness (Table 6).
The analysis with distress as a criterion revealed that the subscale Meaningfulness was associated with less distress, and the subscale Solving Pain with more distress, even after controlling for demographic and pain characteristics (Table 7).
Sensitivity to change
To assess whether the PaSol subscales were sensitive with regard to change (eg, improvements through treatment), we calculated 2×2 mixed design ANOVAs with the factors of improvement (yes/no) and time (pre/post) and the PaSol subscales as dependent variables. For the subscales Solving Pain (F[1,64] =0.73, p=0.396) and Belief (F[1,64] =0.75, p=0.749), no effects were observed. The subscale Acceptance showed a main effect for time (F[1,64] =7.95, p=0.006, h2=0.031) and tendencies regarding a main effect for improvement (F[1,64] =2.74, p=0.102, h2=0.029) and the interaction (F[1,64] =2.87, p=0.095, h2=0.011). For the subscale Meaningfulness, the ANOVA revealed significant main effects for improvement (F[1,64] =10.51, p=0.002, h2=0.093) and time (F[1,64] =10.40, p=0.002, h2=0.045) and a significant interaction improvement × time (F[1,64] =5.49, p=0.022, h2=0.024). The results of the post hoc tests are shown in Figure 1.
Discussion
This is the first study developing and validating a German translation of the PaSol and investigating it in a sample of patients suffering from CLBP. The psychometric properties were satisfactory, and the exploratory factor analysis reflected the same four-factor structure and factor loadings comparable to those of the original version. The reliability and validity analyses demonstrated acceptable to good results, and the scale was sensitive to detect changes over time.
Item analysis and reliability
The internal consistencies for the subscales ranged from Cronbach’s a =0.71 to 0.84, which is in line with other results (a=0.72–0.84; a=0.77–0.86).7,18 Taking into account that the PaSol is a very short instrument, consisting of 14 items in total with subscales of two to five items, these values are no reason for concern, since the brevity limits the internal consistency for statistical reasons. This is supported by the fact that excluding particular items does not result in a substantial improvement of the internal consistency.
Mean item difficulties for the subscales ranged from pi=0.62 for the subscale Belief in a Solution to pi=0.79 for the subscale Solving Pain as desired in the context of attitude measurement.44
To analyze the validity of the PaSol, an exploratory factor analysis was preferred, since only the original study provided information regarding the factor structure and its subscales. The analysis revealed an identical item–subscale classification within a four-factor solution for the German version of the PaSol compared to the original version of the questionnaire, indicating that the factor structure was reproduced in patients suffering from CLBP and in a German population.
One aim in the development of the PaSol was to identify factors beyond pain-related parameters that influence outcome and process measures. Therefore, items were constructed to separate potential outcome and process measures. The small-to-moderate correlations between the subscales of the PaSol and pain characteristics, pain-related disability, attention to pain, and affective distress indicate that the PaSol has good discriminant validity and does indeed measure aspects of adjusting to living with CLBP that go beyond those captured simply by the pain parameters. The strongest correlations were found for catastrophic thinking and the PaSol subscales Meaningfulness of Life Despite Pain and Acceptance of the Insolubility of Pain. The correlative results of our study support findings that the tenacious use of assimilative coping strategies is associated with higher levels of catastrophizing and worry, whereas accommodative coping, such as accepting pain and disengaging from the goal of analgesia, has been found to be beneficial regarding pain-related outcomes.11,16,45,46 Yet, there are little data on the course of which coping styles are being used by patients with chronic pain and this should be further examined. For clinicians, it can be of interest to differentiate which way of coping a patient uses since different ways of coping may require different therapeutic strategies.
In a further step, we investigated the unique contribution of the PaSol subscales in explaining pain-related disability and affective distress, which are both important outcomes in the field of chronic pain recommended for investigation by the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT).40 The results for affective distress showed that the subscales Meaningfulness and Solving Pain had a unique contribution in explaining variance, even when controlling for age and sex as demographic variables and pain intensity, pain quality, and pain duration as pain characteristics. Less affective distress was reported when patients valued their lives as more meaningful despite having chronic pain. The opposite was found for the subscale Solving Pain. This pattern is in line with the results of the original PaSol study as well as other studies investigating different coping styles.7,18 However, none of the PaSol subscales explained variance for pain-related disability uniquely when also accounting for demographic and all pain characteristics. This contrasts with the original study, in which the subscale Meaningfulness was found to explain unique variance with regard to disability (although at 3%, this was not much). However, we further investigated the prediction of pain-related disability and found the subscale Meaningfulness to provide a unique contribution only when pain duration was excluded from the analyses. In the literature, the influence of pain duration on the use of pain coping strategies was found to be more complex than first expected. Assimilative coping strategies tended to be used more by patients with acute pain and accommodative coping strategies by patients who had experienced pain for a long time.7 Our study sample showed a large range regarding pain duration. Although all patients suffered from chronic – not acute – pain (defined as pain for more than 3 months), the pain duration differed strongly between patients (6 months to 50 years). The rather complex relationship between pain duration and the used coping strategy might explain our finding to some extent, even though pain duration did not influence the unique contribution for affective distress. Additional studies are needed to examine the temporal aspects of the use and change of coping strategies.
A first step in this direction was the analysis of the relationship between treatment improvements and coping strategies as measured by the PaSol. Our results indicated that patients who improved during the treatment scored more highly on the subscale Meaningfulness compared to patients who did not improve during treatment and compared to pretreatment. The same relationship (albeit only a tendency) was found for the subscale Acceptance. These results indicate that treatment improvements can lead to a higher use of accommodative coping strategies such as accepting rather than “fighting” pain, and experiencing a meaningful life. These results agree with findings showing that acceptance-based therapies might lead to reductions in pain intensity and depression.14 Furthermore, the results also suggest that the PaSol is a useful and sensitive instrument to detect such changes during a therapeutic process, even though at this point this can only be said for accommodative coping. Assimilative coping was not affected by treatment improvements in this study.
The current study has some limitations. First, we did not conduct a confirmatory factor analysis because the study sample was too small. In a further study, the factor structure should be investigated to examine the model fit with confirmatory methods. Several relevant pain-related outcomes were assessed, but due to the already large number of questionnaires, a specific acceptance-based questionnaire, eg, the CPAQ,19 could not be included and should be used in a further validation study. Further, chronicity was defined as persisting pain for more than 3 months and does not account for other potentially relevant outcomes related to pain duration, such as treatments received or health care system utilization.47 A closer examination of chronicity could give more insight into temporal dynamics of coping strategies as measured by the PaSol. In addition, only self-reported measures were employed; for future studies, it would be desirable to assess behavior directly, eg, with the Behavioral Avoidance Test – Back Pain for CLBP patients,48 and to further examine the validity and sensitivity of the PaSol.
Conclusion
This study supports the use of the translated German version of the PaSol as a reliable and valid instrument for the assessment of accommodative and assimilative coping strategies in a sample of CLBP patients. The reported four-factor solution in the original version of the PaSol was also found in this German version. First analyses showed the unique contribution of the PaSol in the prediction of pain-related disability and affective distress. In addition, our results support the PaSol – especially the subscales for accommodative coping – to be sensitive to detect changes following psychotherapeutic interventions. This may be of particular interest, because to date there is little knowledge on the temporal dynamics of coping strategy change and how assimilative and adaptive coping affect the development from acute to chronic pain.
Acknowledgments
This study was supported by a grant from the German Research Foundation “Deutsche Forschungsgemeinschaft” (DFG; Grant No. DFG-GL 607) to Julia Anna Glombiewski. The DFG did not play any role in the design of the study and the collection, analysis, and interpretation of the data. They did not participate in the writing of the manuscript or the decision to submit it for publication.
Disclosure
The authors report no conflicts of interest in this work.
References
Gore M, Sadosky A, Stacey BR, Tai K-S, Leslie D. The burden of chronic low back pain. Spine (Phila Pa 1976). 2012;37(11):E668–E677. | ||
van Tulder MW, Koes BW, Metsemakers JF, Bouter LM. Chronic low back pain in primary care: a prospective study on the management and course. Fam Pract. 1998;15(2):126–132. | ||
Costa CM, Maher CG, Hancock MJ, Mcauley JH, Herbert RD, Costa LOP. The prognosis of acute and persistent low-back pain: a meta-analysis. CMAJ. 2012;184(11):613–624. | ||
Sanderson KB, Roditi D, George SZ, Atchison JW, Banou E, Robinson ME. Investigating patient expectations and treatment outcome in a chronic low back pain population. J Pain Res. 2012;5:15–22. | ||
Hayes SC, Bisset RT, Korn Z, et al. The impact of acceptance versus control rationales on pain tolerance. Psychol Rec. 1999;49:33–47. | ||
Gutiérrez O, Luciano C, Rodríguez M, Fink BC. Comparison between an acceptance-based and a cognitive-control-based protocol for coping with pain. Behav Ther. 2004;35(4):767–783. | ||
Crombez G, Eccleston C, Van Hamme G, De Vlieger P. Attempting to solve the problem of pain: a questionnaire study in acute and chronic pain patients. Pain. 2008;137(3):556–563. | ||
Brandtstädter J, Renner G. Tenacious goal pursuit and flexible goal adjustment: explication and age-related analysis of assimilative and accommodative strategies of coping. Psychol Aging. 1990;5(1):58–67. | ||
Van Damme S, Crombez G, Eccleston C. Coping with pain: a motivational perspective. Pain. 2008;139(1):1–4. | ||
Rusu AC, Hasenbring M. Multidimensional Pain Inventory derived classifications of chronic pain: evidence for maladaptive pain-related coping within the dysfunctional group. Pain. 2008;134:80–90. | ||
Aldrich S, Eccleston C, Crombez G. Worrying about chronic pain: vigilance to threat and misdirected problem solving. Behav Res Ther. 2000;38:457–470. | ||
Eccleston C, Crombez G. Worry and chronic pain: a misdirected problem solving model. Pain. 2007;132(3):233–236. | ||
McCracken LM, Carson JW, Eccleston C, Keefe FJ. Acceptance and change in the context of chronic pain. Pain. 2004;109(1–2):4–7. | ||
Veehof MM, Oskam MJ, Schreurs KMG, Bohlmeijer ET. Acceptance-based interventions for the treatment of chronic pain: a systematic review and meta-analysis. Pain. 2011;152(3):533–542. | ||
Crombez G, Van Damme S, Eccleston C. Hypervigilance to pain: an experimental and clinical analysis. Pain. 2005;116:4–7. | ||
Van Damme S, Crombez G, Eccleston C. Retarded disengagement from pain cues : the effects of pain catastrophizing and pain expectancy. Pain. 2002;100:111–118. | ||
Crombez G, Lauwerier E, Goubert L, Van Damme S. Goal pursuit in individuals with chronic pain: a personal project analysis. Front Psychol. 2016;7:1–9. | ||
De Vlieger P, Bussche EV, Eccleston C, Crombez G. Finding a solution to the problem of pain: conceptual formulation and the development of the Pain Solutions Questionnaire (PaSol). Pain. 2006;123(3):285–293. | ||
McCracken L, Vowles K, Eccleston C. Acceptance of chronic pain: component analysis and a revised assessment method. Pain. 2004;107(1–2):159–166. | ||
Evers AWM, Kraaimaat FW, van Lankveld W, Jongen PJH, Jacobs JWG, Bijlsma JWJ. Beyond unfavorable thinking: the illness cognition questionnaire for chronic diseases. J Consult Clin Psychol. 2001;69(6):1026–1036. | ||
Lauwerier E, Caes L, Van Damme S, Goubert L, Rosseel Y, Crombez G. Acceptance: what’s in a name? A content analysis of acceptance instruments in individuals with chronic pain. J Pain. 2015;16(4):306–317. | ||
Lauwerier E, Paemeleire K, Van Damme S, Goubert L, Crombez G. Medication use in patients with migraine and medication-overuse headache: the role of problem-solving and attitudes about pain medication. Pain. 2011;152(6):1334–1339. | ||
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000;25(24):3186–3191. | ||
Treede R, Rief W, Barke A, et al. A classification of chronic pain for ICD-11. Pain. 2015;156(6):1003–1007. | ||
Riecke J, Holzapfel S, Rief W, Glombiewski JA. Evaluation and implementation of graded in vivo exposure for chronic low back pain in a German outpatient setting: a study protocol of a randomized controlled trial. Trials. 2013;14:203. | ||
Casser HR, Hüppe M, Kohlmann T, et al. Deutscher Schmerzfragebogen (DSF) und standardisierte Dokumentation mit KEDOQ-Schmerz – Auf dem Weg zur gemeinsamen Qualitätsentwicklung der Schmerztherapie [German pain questionnaire and standardized documentation with the KEDOQ-Schmerz. A way for qual]. Schmerz. 2012;2:168–175. | ||
Pollard C. Preliminary validity study of the pain disability index. Percept Mot Ski. 1984;59:974. | ||
Dillmann U, Nilges P, Saile H, et al. Behinderungseinschätzung bei chronischen Schmerzpatienten [Assessing disability in chronic pain patients]. Schmerz. 1994;8:100–110. | ||
Tait R, Chibnall J, Krause S. The Pain Disability Index: psychometric properties. Pain. 1990;40(2):171–182. | ||
McCracken LM. “Attention” to pain in persons with chronic pain: a behavioural approach. Behav Ther. 1997;28:271–284. | ||
Roelofs J, Peters ML, McCracken L, Vlaeyen JWS. The pain vigilance and awareness questionnaire (PVAQ): further psychometric evaluation in fibromyalgia and other chronic pain syndromes. Pain. 2003;101(3):299–306. | ||
Zigmond A, Snaith R. The hospital anxiety and depression scale. Br Med J. 1986;292:344. | ||
Hinz A, Schwarz R, Herrmann C, Buss U, Snaith R. Hospital anxiety and depression scale – Deutsche Version (HADS-D). Diagnostica. 2002;48:112–113. | ||
Bjelland I, Dahl A, Haug T, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. | ||
Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1995;7(4):524–532. | ||
Meyer K, Sprotta H, Mannion AF. Cross-cultural adaptation, reliability, and validity of the German version of the Pain Catastrophizing Scale. J Psychosom Res. 2008;64(5):469–478. | ||
Osman A, Barrios F, Gutierrez P, Kopper B, Merrifield T, Grittmann L. The Pain Catastrophizing Scale: further psychometric evaluation with adult samples. J Behav Med. 2000;23(4):351–365. | ||
Bortz J, Döring N. Forschungsmethoden und Evaluation. [Research Methods and Evaluation]. 3rd ed. Berlin: Springer; 2003. German. | ||
Menard S. Applied Logistic Regression Analysis. Sage University Paper Series on Quantative Applications in the Social Sciences. Thousand Oaks, CA: Sage Publications; 1995:7–106. | ||
Dworkin RH, Turk DC, Farrar JT, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113:9–19. | ||
Levine TR, Hullett CR. Eta squared, partial eta squared, and misreporting of effect size in communication research. Hum Commun Res. 2002;28(4):612–625. | ||
Corp I. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corporation; 2013. | ||
Leeuw M, Goossens M, van Breukelen G, et al. Exposure in vivo versus operant graded activity in chronic low back pain patients: results of a randomized controlled trial. Pain. 2008;138:192–207. | ||
Fisseni H-J. Lehrbuch der Psychologischen Diagnostik. [Textbook of Psychological Testing]. Göttingen: Hogrefe; 1997. German. | ||
Crombez G, Eccleston C, De Vlieger P, Van Damme S, De Clercq A. Is it better to have controlled and lost than never to have controlled at all? An experimental investigation of control over pain. Pain. 2008;137(3):631–639. | ||
Viane I, Crombez G, Eccleston C, et al. Acceptance of pain is an independent predictor of mental well-being in patients with chronic pain: empirical evidence and reappraisal. Pain. 2003;106(1–2):65–72. | ||
Samolsky Dekel BG, Gori A, Vasarri A, Adversi M, DiNino GF, Melotti RM. Psychometric properties and validation of the Italian version of the Mainz pain staging system as a tool for pain-patients referral selection. J Eval Clin Pract. 2014;20(5):622–630. | ||
Holzapfel S, Riecke J, Rief W, Schneider J, Glombiewski JA. Development and validation of the behavioral avoidance test – back pain (BAT-Back) for patients with chronic low back pain. Clin J Pain. 2016;32(11):940–947. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.