Back to Journals » Medical Devices: Evidence and Research » Volume 7
Critical evaluation of stents in the peripheral arterial disease of the superficial femoral artery – focus on the paclitaxel eluting stent
Authors Litsky J, Chanda A, Stilp E, Lansky A , Mena C
Received 22 December 2013
Accepted for publication 11 February 2014
Published 28 May 2014 Volume 2014:7 Pages 149—156
DOI https://doi.org/10.2147/MDER.S45472
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Jason Litsky,1 Arijit Chanda,2 Erik Stilp,1 Alexandra Lansky,1 Carlos Mena1
1Section of Cardiovascular Medicine, Department of Internal Medicine, Yale University School of Medicine, New Haven, CT, USA; 2Section of Cardiology, Department of Internal Medicine, Bridgeport Hospital, Bridgeport, CT, USA
Abstract: The endovascular management of obstructive disease of the superficial femoral artery (SFA) is challenging due to unique anatomical and biomechanical forces. Obstructive lesions of the SFA make up the largest proportion of lesions leading to symptomatic peripheral arterial disease. Accordingly, endovascular treatment of SFA disease is becoming increasingly common and, in many cases, is the preferred initial therapy. The use of self-expanding nitinol stents have proven superior to percutaneous transluminal balloon angioplasty in the treatment of intermediate length SFA stenosis. However, achieving durable results, as well as attaining adequate therapy for long occlusions typically seen in clinical practice, remains problematic. Newer technologies, such as paclitaxel eluting stents, seem promising in improving outcomes.
Keywords: Zilver PTX, self-expanding stent, atherosclerotic disease, superficial femoral artery
Introduction
Peripheral arterial disease (PAD) is the third leading cause of cardiovascular morbidity after myocardial infarction and stroke.1 The prevalence of PAD increases with age and, accordingly, there has been a rapid rise in disease recognition as well as treatment. Current estimates state that there are over 8 million US and 200 million global patients with PAD.1,2 Patients with PAD have a three-fold increase in mortality and major cardiovascular events.3–5 Ten to twenty percent of patients with PAD have intermittent claudication; however, approximately 50% will have atypical symptoms or be asymptomatic.6,7 Further, patients with PAD, regardless of symptomatology, have a worse quality of life than those without.8
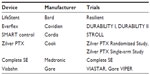
Obstructive disease of the superficial femoral artery (SFA) is the most common cause of intermittent claudication.9 Almost 50 years after Dotter performed the first endovascular SFA intervention, endovascular treatment of lower extremity atherosclerotic disease has become increasingly common.10 Obstructive disease of the SFA accounts for a great proportion of endovascular procedures performed. The low associated morbidity and mortality as well as high technical success rates of endovascular treatment of SFA disease have made it the preferred initial revascularization modality for patients with significant symptomatic disease and short lesions (<10 cm).11 However, unique biomechanical, anatomic, and hemodynamic forces make management of SFA disease challenging. Subsequently, there is a high rate of recurrent lesions requiring additional interventions. Randomized trials have proven primary stenting with self-expanding bare metal stents (BMS) to be better than balloon angioplasty in longer lesions (Table 1).12–14 However, effective treatments of complex lesions commonly encountered in clinical practice, including long occlusions, heavily calcified lesions, and ostial as well as popliteal extension of disease, continue to be lacking. Fortunately, advances in endovascular technologies, including new stent designs and drug eluting technologies, have improved results and offer promise for the future. Herein, we review the data supporting current use of stents in SFA PAD as well as that of the emerging therapeutics of drug-eluting stents (DES).
Difficulty of SFA space
The SFA presents significant challenges in achieving durable results after endovascular intervention secondary to the unique forces to which it is subjected. Continuity with both the popliteal and common femoral arteries exposes the SFA to elongation with ambulation.15 Further, its superficial course and interaction with surrounding musculature subject the SFA to compressive and torsional forces.16 These mechanical forces imparted on the SFA can result in metal fatigue and stent fracture, which has been associated with restenosis.15 In addition, the SFA responds to stent implantation with a more potent inflammatory response than other vessels.17,18 This is in part related to micromovements of the stent alongside the vessel wall leading to activation of the endothelium and inflammation. Further, multiple overlapping stents often utilized in treating long SFA stenosis create hinge points, which can potentiate stent fracture. Additionally, the potential for significant multivessel disease, popliteal and tibial outflow lesions, as well as complex long and calcific lesions often encountered in SFA stenosis can complicate lasting success after endovascular interventions.
Randomized trials of nitinol self-expanding stents
Percutaneous transluminal balloon angioplasty (PTA) for revascularization of the SFA can result in technical success rates of greater than 95% with low rates of associated complications.19 PTA patency rates for treated stenoses <4 cm in length have been reported to be as high as 78% at 3 years.20 However, durable results for more complicated lesions are lacking. Results for long stenoses (>100 mm) are particularly poor, with restenosis rates greater than 70% at 1 year. Stenting improves initial results of SFA intervention via resistance of initial elastic recoil, prevention of flow limiting dissections, and minimizing residual stenoses. However, despite promising early results, balloon expandable stainless steel stents failed to show a sustained benefit over PTA alone in multiple randomized trials.21–25
Second generation self-expanding nitinol stents offer a more flexible stent platform that is more resistant to deformation than previous stainless-steel balloon-expandable stents. To date, there have been five published randomized trials comparing self-expanding nitinol stents to PTA alone in the treatment of symptomatic obstructive SFA disease. The Balloon Angioplasty Versus Stenting with Nitinol Stents in the Superficial Femoral Artery (Vienna-ABSOLUTE) trial was the first randomized trial to report a benefit of primary SFA stenting versus PTA alone.12 The trial randomized 104 patients with Rutherford class 3–5 chronic critical limb ischemia to either PTA or primary stenting with either Dynalink or Absolute (Abbott Laboratories, Abbott Park, IL, USA) self-expanding stents. Fifty-one patients were randomized to the stenting group (mean lesion length of 10.1±7.5 cm) and 53 to PTA alone with bailout stenting (mean lesion length 9.2±6.4 cm). They reported a significant reduction (24% versus 43%; P=0.05) in the primary endpoint of binary restenosis at 6 months. Assessment by Duplex ultrasonography at 12 months also showed significantly lower rates of restenosis in the stenting group (37% versus 63%; P=0.01). These results were maintained at 2 years.26 The observed fracture rate of 2% was greatly improved from the high rates reported in previous balloon expandable trials.
The Femoral Artery Stenting Trial (FAST) randomized patients with at least Rutherford class 2 chronic critical limb ischemia to implantation of a single nitinol self-expanding Luminexx 3 stent (Bard Peripheral Vascular, Inc., Tempe, AZ, USA) or PTA alone.27 Two hundred and forty-four patients were randomized to either stenting (n=123) or PTA (n=121) with a mean lesion length of 45 mm. After 1 year, there was no significant difference (31.7% stenting group versus 38.6% PTA group; P=0.377) in the primary end point of restenosis evaluated by duplex ultrasound. There was also no significant difference in target lesion revascularization (TLR) (18.4% stenting group versus 14.0% PTA group; P=0.595). The low observed rates of restenosis in the PTA group left the trial underpowered to detect a difference of 7% between the two groups. Further, the fracture rate was reported at 12% despite treating shorter lesions. The results of this trial have led to the recommendation that short SFA lesions can be adequately treated with provisional PTA and bailout stenting.
The Balloon Angioplasty Versus Stenting with Nitinol Stents in Intermediate Length Superficial Femoral Artery Lesions (ASTRON) trial randomized 73 patients with symptomatic claudication and intermediate length SFA lesions (mean lesion length 8.4 cm) to either primary stenting (n=34) with the Astron self-expanding nitinol stent (Biotronik, Berlin, Germany) or PTA (n=39).13 Binary restenosis rates at 12 months determined by duplex ultrasonography were 34.4% in the stent group and 61.1% in the PTA group (P=0.028). Further, the patients in the stent group reported a significantly higher maximum walking capacity compared with the PTA group at 6 and 12 months. Unfortunately, stent fracture rates were not reported in this trial.
Treatment of intermediate length lesions was similarly evaluated in the Nitinol Stent Implantation Versus Balloon Angioplasty for Lesions in the Superficial Femoral Artery and Proximal Popliteal Artery (RESILIENT) trial.14 Two hundred and six patients with intermittent claudication (Rutherford categories 1–3) in the US and Europe were randomized at a ratio of 2:1 to stenting (n=134) with the self-expanding nitinol LifeStent (Edwards Lifesciences Corporation, Irving, CA, USA acquired by Bard Peripheral Vascular, Inc.) or PTA (n=72). Mean lesion length was 7.1 cm in the stenting group and 6.4 cm in the PTA group. As part of the trial design, patients who received bailout stenting were considered a TLR and subsequently a loss of a primary patency. Utilizing this analysis, there was a significant benefit in the primary endpoint of freedom from target lesion revascularization at 12 months in the stenting group (87.3% versus 45.1%; P<0.0001). It should be noted that 29 patients (40%) in the PTA group received bailout stenting and were thus considered a TLR at day 0. Lesions that required bailout stenting were significantly longer and more calcified than those effectively treated with PTA alone. Because of the high crossover rate, the data was also analyzed according to the actual treatment received. Primary patency at 1 year for the combined primary and provisional stent group was significantly better than that seen in the optimal PTA alone group (80.4% versus 61.5%; P=0.03), despite the lesions being significantly longer (63.3±41.9 mm versus 47.7±32.6 mm; P<0.01). Three year follow-up intention-to-treat analysis (ITT) data reported freedom from TLR (75.5% versus 41.8%; P<0.0001) and clinical success (63.2% versus 17.9%; P<0.0001) to be significantly better in the stent group.28 This trial confirms the findings from both the ABSOLUTE and ASTRON trials that support the utilization of self-expanding nitinol stents in intermediate length lesions in the SFA.
The recently published Randomized Trial of the SMART Stent versus Balloon Angioplasty in Long Superficial Femoral Artery Lesions (SUPER) study hints at the possible limitations of bare metal stents in long lesions.29 The trial randomized 150 patients with SFA occlusions or severe stenoses of 5–22 cm in length to either the SMART stent (Cordis Corporation, Hialeah, FL, USA) or PTA. The patients had long average lesion lengths (12.3±5.4 cm) and 93% had total occlusions. The study reported no significant benefits to stenting over PTA (47.2% versus 43.5%; P=0.68) in the primary endpoint of restenosis at 1 year. The SUPER trial recruited patients with lesions 20% longer and with 2.5 times the total occlusion of previously published trials. Further, there was a higher percentage of patients enrolled with critical limb ischemia. The authors postulate that these factors, which predispose towards poorer outcomes, along with subintimal tracking and reentry techniques used in the majority of the procedures accounted for the reduced expected effect size observed.
Registries of nitinol self-expanding stents
Registry data from second generation nitinol self-expanding BMS have lent further promise to endovascular treatment of obstructive SFA disease. These data have led to US Food and Drug Administration (FDA) approval of a number of newer available stents that may provide greater flexibility, less stent fracture, and, possibly, more durable results. The Everflex Protégé (Covidien, Mansfield, MA, USA) nitinol self-expanding stent was evaluated in The United States Study for Evaluating Endovascular Treatments of Lesions in the Superficial Femoral Artery and Proximal Popliteal By using the Protégé Everflex Nitinol Stent System (DURABILITY I and DURABILITY II) trials.30,31 Although these trials were nonrandomized, they enrolled a similar group of patients evaluated in previous randomized studies and treated long complex lesions (mean lesion lengths of 96.4±26.8 and 89±44.8, respectively, with an average of 40% complete occlusions). The results from both trials reinforced the findings from the randomized ABSOLUTE, ASTRON, and RESILIENT trials in supporting primary stenting for intermediate length SFA lesions. The authors reported 6 and 12 month freedom from restenosis in DURABILITY I of 91.3% and 72.2%, respectively, with similar patency rates seen in DURABILITY II.
The COMPLETE SE trial evaluated the use of the Complete SE stent (Medtronic, Inc., Fridley, MN, USA) in intermediate length SFA disease.32 One hundred and ninety-six patients were enrolled and the authors reported favorable results with primary patency rates of 73.1% at 1 year. Similarly the STROLL trial is a single-arm nonrandomized prospective study evaluating the efficacy of the SMART stent in intermediate length (mean lesion length 77 mm) SFA obstructions.33 Recently reported data revealed a 2 year primary patency rate of 74.9% with 80.3% freedom from target lesion revascularization.
The SUPERA stent (IDEV Technologies, Webster, TX, USA, acquired by Abbott) is a self-expanding stent composed of six pairs of interwoven nitinol wires in a closed-cell configuration. This design imparts significantly greater radial strength and resistance to stent fracture, which has been one of the shortcomings of treating longer stenosis typically seen in clinical practice. A European retrospective registry study of 107 patients with complex SFA (mean lesion length 111±50 mm) disease reported cumulative primary patency rates at 6, 12, and 24 months of 93.1%±2.5%, 84.7%±3.6%, and 76.1%±4.5%, respectively.34 Encouragingly, there were no reported stent fractures at a mean of 16.8±7 months. This device is currently being evaluated in the US in the SUPERB registry. Currently, there are multiple ongoing trials both in the US and Europe evaluating other self-expanding stent designs including the 4EVER, SuperNOVA, TIGRIS, and OSPREY trials.
Covered stents
Treatment with covered stents provides an alternative approach in endovascular treatment of SFA obstructive disease. The device is analogous to a surgical bypass graft as there is complete exclusion of potential collaterals within the stented segment. Although there is some promise to newer self-expanding bare metal stents in treating long diseased segments, they are subject to neointimal hyperplasia and restenosis.35 The GORE® VIABAHN® Endoprosthesis (WL Gore and Associates, Inc., Newark, DE, USA) is a heparin-bonded expanded-polytetrafluoroethylene-covered stent that has been FDA approved for use in SFA disease. The expanded polytetrafluoroethylene covering mitigates ingrowth of neointimal tissue regardless of lesion length. In a randomized comparison of surgical bypass versus Viabahn stent grafting, patency rates were similar at up to 4-years follow-up.36 The VIABAHN endoprosthesis versus bare nitinol stent implantation for complex superficial femoral artery occlusive disease (VIBRANT) trial was a randomized trial that enrolled 148 patients with complex symptomatic TASC C or D SFA disease (mean lesion length 18±8 cm).37 At 3 years, the primary patency rates did not significantly differ between the patients treated with the Viabahn endograft and those treated with bare metal stents (24.2% versus 25.9%; P=0.392). Further, hemodynamic and quality measures improved equally in both groups. A newer generation Viabahn stent incorporating a contoured proximal edge was recently evaluated in the Viabahn Endoprosthesis With PROPATEN Bioactive Surface [VIA] Versus Bare Nitinol Stent in the Treatment of Long Lesions in Superficial Femoral Artery Occlusive Disease (VIASTAR) trial.38 One hundred and forty-one patients with complex disease (mean lesion length 18.1 cm) were randomized to either a Viabahn covered stent (n=72) or a self-expanding nitinol stent (n=69). The 12-month primary patency rate in the ITT analysis was not significantly different (70.9% versus 55.1%; P=0.11). However, major protocol deviations were noted in 8.5% of the patients. Accordingly, in the treatment per-protocol analysis, the Viabahn endoprosthesis showed a primary patency rate of 78.1% versus 53.5% (P=0.009) for BMS group. Of note, in patients with long lesions (>20 cm), the primary patency rates at 12 months by ITT were significantly higher in the Viabahn group than in the BMS group (71.3% versus 36.8%; P=0.01). While the durability of bare metal stenting procedures seems to be inversely proportional to the length of the treatment zone, patency following implantation of covered stents appears independent.
Drug eluting stents
Sirolimus is an immunosuppressant drug with direct inhibitory effects on the mammalian target of rapamycin. It is highly effective in reducing neointimal proliferation leading to coronary artery restenosis. The Sirolimus-Coated Cordis Self-Expandable Stent for the Treatment of SFA Disease (SIROCCO) trial was a double-blind randomized controlled trial comparing the efficacy of the sirolimus-eluting SMART stent (Cordis Corporation) with its BMS counterpart in the treatment of long SFA obstructions.39,40 The stents were composed of a SMART stent with a 5 μm coating composed of an elastic copolymer combined with sirolimus at an equivalent dose to that used in coronary applications (90 μg/cm2) at the time. The trial was undertaken in two separate 6-month phases, each with slightly different endpoints. Although the initial results were encouraging, with reduced binary restenosis and neointimal hyperplasia in the sirolimus-eluting group at 6 months, by 18 months, the sirolimus group had demonstrated significant catch-up phenomenon resulting in similar clinical and angiographic outcomes between the two groups. Further, after 4 years of follow-up, there continued to be no significant benefit in any metric found in the sirolimus-eluting group.41 Some hypothesized explanations for the poor results seen in the SIROCCO trials, which are lower than expected rates of restenosis in the BMS group, and the high rates of stent fracture (18% at 6 months). Further, the stent was loaded with a significantly lower dose of sirolimus than was utilized in the successful sirolimus-eluting DES (Cypher [Cordis Corporation], 140 μg/cm2). Lastly, the SIROCCO stent eluted the majority of the drug within 7 days, which is substantially more rapid than the approximate 30-day elution profile in the Cypher stent.
Similarly to sirolimus, everolimus effectively inhibits vascular-smooth-muscle-cell proliferation and has been shown to be a safe and effective drug component in coronary DES.42,43 The safety and performance of an everolimus-eluting self-expanding stent was evaluated in the Superficial Femoral Artery Treatment with Drug-Eluting Stents (STRIDES) trial.44 STRIDES was proposed to address some of the potential short comings of the SIROCCO trials. STRIDES was a prospective nonrandomized single-arm trial that utilized the Dynalink-E stent. The stent entailed three components: a Dynalink self-expanding stent, the antiproliferative drug everolimus, and an ethylene–vinyl–alcohol copolymer. The total drug load was 225 μg/cm2, which was a higher dose than coronary sirolimus-eluting (140 μg/cm2) or everolimus-eluting (100 μg/cm2) stents. The elution profile was such that 80% of the drug was released over the first 90 days, as opposed to 30 days in coronary applications. The primary patency was 94%±2.3% and 68%±4.6% at 6 and 12 months, respectively, and there was no evidence of stent fracture. The patency rates at 12 months were nominally improved over those observed in a similar patient population implanted with the Dynalink/Absolute bare metal stent (63%±7%).12 Similar restenosis phenomena were observed in the SIROCCO trials, with good short-term results followed by a rapid rise in restenosis rates. This suggests, perhaps, that the DES were either not implanted with enough drug or that the nature of the elution kinetics is not enough to overcome chronic interactions between the stent and the SFA. In conclusion, there is not strong data at this time to suggest that results in the treatment of SFA disease attained with DES, implanted with either sirolimus or everolimus, are more durable than those attained with their BMS counterparts.
Zilver PTX
The Zilver PTX stent (Cook Group Incorporated, Bloomington, IN, USA) is the only FDA-approved drug-eluting stent for use in the SFA. The stent incorporates a flexible self-expanding nitinol platform with a polymer-free paclitaxel coating at 3 μg/mm2 dose density. Paclitaxel is a highly lipophilic drug that alters microtubule formation and inhibits smooth muscle cell migration and proliferation.45 It has a narrow therapeutic range and, at higher concentrations, can disrupt the internal elastic lamina.46 The stent was evaluated in the pivotal Zilver PTX trial, which randomized patients with relatively short SFA (mean lesion length 5.4±4.1 cm, 29.6% total occlusions) lesions to either the Zilver PTX stent or PTA.47 A BMS was not used as a comparator as, at the onset of the trial, there was no FDA-approved device for use in the SFA. The trial allowed use of only one stent per patient. Four hundred and seventy-nine patients were randomized to receive either the Zilver stent (n=238) or PTA (n=241). There were 120 therapeutic failures in the primary PTA group, and this group underwent a second randomization to receive either the Zilver PTX stent (n=61) or a BMS (Zilver; Cook Group Incorporated) (n=59). In the primary analysis, acute PTA failure was considered as a loss of patency. The primary effectiveness endpoint at 12 months was primary patency, defined by a peak systolic velocity ratio of less than 2.0 by duplex ultrasonography or a stenosis of >50% on angiography. Primary patency at 12 months was significantly better in the Zilver PTX group (83.1% versus 32.8%; P<0.01). These benefits were maintained at 2 years with superior event-free survival (86.6% versus 77.9%; P=0.02) and primary patency (74.8% versus 26.5%; P<0.01) in the Zilver PTX group.48 A 12-month primary patency rate of 65.3% observed in the group treated with optimal initial PTA (n=118) was also statistically inferior to that of the Zilver PTX group (P<0.01). Analysis of the subgroup with suboptimal initial PTA results, who underwent a second randomization before provisional stenting, found the 12-month primary patency rate to be better in the PTA and Zilver PTX group than in the PTA and BMS group (89.9% versus 73%; P=0.01). The provisional DES group exhibited continued superior primary patency at 2 years over the provisional BMS group (83.4% versus 64.1%; P=0.05). Four-year results, encompassing >75% of patients enrolled, found continued superiority in freedom from TLR (83.2% versus 69.4%; P<0.01) and primary patency (67.6% versus 45.5%; P<0.01) in the Zilver PTX group.49 Further, 4-year data of patients treated with provisional stenting after suboptimal PTA found improved freedom from TLR (75% versus 57.9%; P=0.04) in the Zilver PTX group. Some criticisms of the trial were that the lesions treated were relatively short and not typical of those seen in clinical practice, and that the use of a single stent may have aided in minimizing stent fracture.
A covariate analysis for TLR and patency was performed for all DES patients, including metrics often considered predictive of restenosis and loss of primary patency such as reference vessel diameter, lesion length, calcification, total occlusion, and DM. Smoking was the only factor that predicted TLR. The duration of dual antiplatelet therapy was the only factor that predicted patency rates. Patients adhering to DAPT for greater that 1 month had better patency rates than those not on DAPT. However, a significant added benefit could not be demonstrated in patients on DAPT for intervals greater than 3 months.
Further evaluation of the clinical effectiveness of the Zilver PTX stent was attained in the single-arm clinical study, which was a prospective multicenter registry trial enrolling 737 patients with symptomatic SFA disease. This study included longer and more complicated lesions than the randomized trial (mean lesion length 99.2±82.1 mm, 31.1% total occlusions, 8.4% severely fractured stents [type III or IV]) and multiple stent use was permitted (average 2.2 stents per patient). Nine hundred lesions were treated (38.3% total occlusions, 24.3% restenosis) in total with a primary patency rate of 83% at 1 year and freedom from TLR of 90.5% and 80.5% at 1 and 2 years, respectively.
This trial also gleaned hope for treatment of some of the most notoriously difficult to manage lesions. There was a significant cohort of patients enrolled in the trial with in-stent restenosis lesions (ISR). Success in this difficult to treat cohort of patients has continued to be one of the biggest shortcomings of endovascular therapy in the SFA. In total, 108 patients with 119 ISR lesions were enrolled in the ZILVER-PTX single-arm study.50 The lesions were long (mean lesion length 133±91.7 mm) and an average of 2.1±1.2 stents were used per patient. The results achieved were encouraging, with primary patency rates of 95.7% and 78.8% at 6 months and 1 year, respectively, and freedom from TVR of 96.2%, 81.0%, and 60.8% at 6 months, 1 year, and 2 years, respectively. Diabetes and long (>15 cm) de novo lesions are independent predictors of decreased long term patency in SFA interventions.51 Previously reported 1-year patency rates after SFA stenting in diabetic patients with long lesions have been reported to be as low as 22%.52 One-year patency rates of 86% and 77% observed in diabetic patients and patients with long (15 cm) lesions, respectively, enrolled in the single arm of the Zilver study offer promise. Further, the 1-year patency rate of 77% in diabetics with long lesions is also encouraging.
Conclusion
Endovascular therapy has become increasingly common in the treatment of obstructive SFA disease. It can be accomplished with high levels of procedural success despite low clinical risk to patients. However, durable results with PTA were found to be clearly lacking in early studies. The advent of self-expanding nitinol stents has greatly improved results in treatment of intermediate length SFA lesions, and there are currently a number of FDA-approved devices (Table 2). Yet, there still remains substantial room for improvement both in de novo and ISR lesions. Endovascular intervention in the SFA is complex secondary to the unique mechanical, anatomical, and hemodynamic metrics at work, and durable results in complex lesions are lacking at this time. Early drug-eluting studies utilizing mammalian-target-of-rapamycin inhibitors, unfortunately, did not show the clinical effectiveness they had in coronary artery interventions. Whether this is a result of under dosing of the delivered drug, inadequate drug-elution kinetics, or the relative thickness of the tunica media in the SFA in comparison to its coronary artery counterpart is not clear. Despite all these potential limitations, recent data on paclitaxel-eluting therapies (both DES and drug-eluting balloons) are encouraging. These new technologies will certainly lead to an improvement in current endovascular therapy. However, exuberance should be tempered and caution exercised until long term randomized results prove to be durable and safe.
Disclosure
The authors report no conflicts of interest in this work.
References
Fowkes FG, Rudan D, Rudan I, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet. 2013;382: 1329–1340. | |
Roger VL, Go AS, Lloyd-Jones DM, et al. Heart Disease and Stroke Statistics 2011 Update: A Report From the American Heart Association. Circulation. 2011;123:e18–e209. | |
Pande RL, Perlstein TS, Beckman JA, Creager MA. Secondary prevention and mortality in peripheral artery disease: National Health and Nutrition Examination Study, 1999 to 2004. Circulation. 2011;124:17–23. | |
Smith GD, Shipley MJ, Rose G. Intermittent claudication, heart disease risk factors, and mortality. The Whitehall Study. Circulation. 1990;82:1925–1931. | |
Ankle Brachial Index Collaboration, Fowkes FG, Murray GD, et al, and the Ankle Brachial Index Collaboration. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. JAMA. 2008;300:197–208. | |
Stoffers HE, Rinkens PE, Kester AD, Kaiser V, Knottnerus JA. The prevalence of asymptomatic and unrecognized peripheral arterial occlusive disease. Int J Epidemiol. 1996;25:282–290. | |
Hirsch AT, Criqui MH, Treat-Jacobson D, et al. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001;286:1317–1324. | |
McDermott MM, Fried L, Simonsick E, Ling S, Guralnik JM. Asymptomatic peripheral arterial disease is independently associated with impaired lower extremity functioning: the women’s health and aging study. Circulation. 2000;101:1007–1012. | |
White C. Clinical practice. Intermittent claudication. N Engl J Med. 2007;356:1241–1250. | |
Dotter CT, Judkins MP. Transluminal treatment of atherosclerotic obstructions: description of a new technique and preliminary report of its applications. Circulation. 1964;30:654–670. | |
Norgren L, Hiatt WR, Dormandy JA, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg. 2007;45 Suppl S:S5–S67. | |
Schillinger M, Sabeti S, Loewe C, et al. Balloon angioplasty versus implantation of nitinol stents in the superficial femoral artery. N Engl J Med. 2006;354:1879–1888. | |
Dick P, Wallner H, Sabeti S, et al. Balloon angioplasty versus stenting with nitinol stents in intermediate length superficial femoral artery lesions. Catheter Cardiovasc Interv. 2009;74:1090–1095. | |
Laird JR, Katzen BT, Scheinert D, et al. Nitinol stent implantation versus balloon angioplasty for lesions in the superficial femoral artery and proximal popliteal artery: twelve-month results from the RESILIENT randomized trial. Circ Cardiovasc Interv. 2010;3:267–276. | |
Schienert D, Schienert S, Sax J, et al. Prevalence and clinical impact of stent fractures after femoropopliteal stenting. J Am Coll Cardiol. 2005;45(2):312–315. | |
Cheng CP, Wilson NM, Hallett RL, Herfkens RJ, Taylor CA. In vivo MR angiographic quantification of axial and twisting deformations of the superficial femoral artery resulting from maximum hip and knee flexion. J Vasc Interv Radiol. 2006;17(6):979–987. | |
Schillinger M, Exner M, Mlekusch W, et al. Balloon angioplasty and stent implantation induce a vascular inflammatory reaction. J Endovasc Ther. 2002;9(1):59–66. | |
Schillinger M, Exner M, Mlekusch W, et al. Inflammatory response to stent implantation: differences in femoropopliteal, iliac, and carotid arteries. Radiology. 2002;224(2):529–535. | |
Dormandy JA, Rutherford RB. Management of peripheral arterial disease (PAD). TASC Working Group. TransAtlantic Inter-Society Consensus (TASC). J Vasc Surg. 2000;31:S1–S296. | |
Capek P, Maclean GK, Berkowitz HD. Femoropopliteal angioplasty: factors influencing long-term success. Circulation. 1991;83(Suppl 2):I70–I80. | |
Cejna M, Turnher S, Illiasch H, et al. PTA versus Palmaz stent in femoropopliteal artery obstructions: a multicenter prospective randomized study. J Vasc Interv Radiol. 2001;12:23–31. | |
Vroegindeweij D, Vos LD, Tielbeek AV, Buth J, vd Bosch HC. Balloon angioplasty combined with primary stenting versus balloon angioplasty alone in femoropopliteal obstructions: a comparative randomized study. Cardiovasc Intervent Radiol. 1997;20:420–425. | |
Grimm J, Müller-Hülsbeck S, Jahnke T, Hilbert C, Brossmann J, Heller M. Randomized study to compare PTA alone versus Palmaz stent placement for femoropopliteal lesions. J Vasc Interv Radiol. 2001;12: 935–942. | |
Zdanowski Z, Albrechtsson U, Lundin A, et al. Percutaneous transluminal angioplasty with or without stenting for femoropopliteal occlusions? A randomized controlled study. Int Angiol. 1999;18:251–255. | |
Becquemin JP, Favre JP, Marzelle J, Nemoz C, Corsin C, Leizorovicz A. Systematic versus selective stent placement after superficial femoral artery balloon angioplasty: a multicenter prospective randomized study. J Vasc Surg. 2003;37:487–494. | |
Schillinger M, Sabeti S, Dick P, et al. Sustained benefit at 2 years of primary femoropopliteal stenting compared with balloon angioplasty with optional stenting. Circulation. 2007;115:2745–2749. | |
Krankenberg H, Schlüter M, Steinkamp HJ, et al. Nitinol stent implantation versus percutaneous transluminal angioplasty in superficial femoral artery lesions up to 10 cm in length: the femoral artery stenting trial (FAST). Circulation. 2007;116:285–292. | |
Laird JR, Katzen BT, Scheinert D, et al. Nitinol stent implantation vs balloon angioplasty for lesions in the superficial femoral and proximal popliteal arteries of patients with claudication: three-year follow-up from the RESILIENT randomized trial. J Endovasc Ther. 2012;19: 1–9. | |
Chalmers N, Walker PT, Belli AM, et al. Randomized trial of the SMART stent versus balloon angioplasty in long superficial femoral artery lesions: the SUPER study. Cardiovasc Intervent Radiol. 2013;36(2):353–361. | |
Bosiers M, Torsello G, Gissler HM, et al. Nitinol stent implantation in long superficial femoral artery lesions: 12-month results of the DURABILITY I study. J Endovasc Ther. 2009;16:261–269. | |
Matsumara JS, Yamonouchi D, Goldstein JA, et al. The United States study for evaluating endovascular treatments of lesions in the superficial femoral artery and proximal popliteal by using the Protégé Everflex nitinol stent system II (DURABILITY II). J Vasc Surg. 2013;58(1):73–83. | |
Laird JR. Update on the Complete SE trial. Paper presented at: International Symposium on Endovascular Therapy; January 18, 2012; Miami, FL. | |
Gray W. SMART Vascular Stent Systems in the Treatment of Obstructive Superficial Femoral Artery Disease trial 2 year data. Paper presented at: International Symposium on Endovascular Therapy; January 21, 2013; Miami, FL. | |
Scheinert D, Grummt L, Piorkowski M, et al. A novel self-expanding interwoven nitinol stent for complex femoropopliteal lesions: 24-month results of the SUPERA SFA registry. J Endovasc Ther. 2011;18(6):745–752. | |
Bosiers M, Deloose K, Callert J, et al. Results of the Protégé EverFlex 200-mm-long nitinol stent (ev3) in TASC C and D femoropopliteal lesions. J Vasc Surg. 2011;54:1042–1050. | |
McQuade K, Gable D, Pearl G, Theune B, Black S. Four-year randomized prospective comparison of percutaneous ePTFE/nitinol self-expanding stent graft versus prosthetic femoral-popliteal bypass in the treatment of superficial femoral artery occlusive disease. J Vasc Surg. 2010;52:584–590. | |
Geraghty PJ, Mewissen MW, Jaff MR, Ansel GM; VIBRANT Investigators. Three-year results of the VIBRANT trial of VIABAHN endoprosthesis versus bare nitinol stent implantation for complex superficial femoral artery occlusive disease. J Vasc Surg. 2013;58(2):386–395. | |
Lammer J, Zeller T, Hausegger KA, et al. Heparin-bonded covered stents versus bare-metal stents for complex femoropopliteal artery lesions: the randomized VIASTAR trial (Viabahn endoprosthesis with PROPATEN bioactive surface [VIA] versus bare nitinol stent in the treatment of long lesions in superficial femoral artery occlusive disease). J Am Coll Cardiol. 2013;62(15):1320–1327. | |
Duda SH, Pusich B, Richter G, et al. Sirolimus-eluting stents for the treatment of obstructive superficial femoral artery disease: six month results. Circulation. 2002;106(12):1505–1509. | |
Duda SH, Bosiers M, Lammer J, et al. Sirolimus-eluting versus bare metal nitiniol stent for obstructive superficial femoral artery disease: the SIROCCO II trial. J Vasc Interv Radiol. 2005;16(3):331–338. | |
Duda SH, Bosiers M, Lammer J, et al. Drug-eluting and bare metal nitinol stents for the treatment of atherosclerotic lesions in the superficial femoral artery: long-term results from the SIROCCO trial. J Endovasc Ther. 2006;13(6):701–710. | |
Carter AJ, Brodeur A, Collingwood R, et al. Experimental efficacy of an everolimus eluting cobalt chromium stent. Cath Cardiovasc Interv. 2006;68:97–103. | |
Stone GW, Midei M, Newman W, et al. Comparison of an everolimus-eluting stentand a paclitaxel-eluting stent in patient with coronary artery disease: a randomized trial. JAMA. 2008;299:1903–1913. | |
Lammer J, Bosiers M, Zeller T, et al. First clinical trial of nitinol self-expanding everolimus-eluting stent implantation for peripheral arterial occlusive disease. J Vasc Surg. 2011;54:394–401. | |
Axel DI, Kunert W, Göggelmann C, et al. Paclitaxel inhibits arterial smooth muscle cell proliferation and migration in vitro and in vivo using local drug delivery. Circulation. 1997;96:636–645. | |
Pires NM, Eefting D, de Vries MR, Quax PH, Jukema JW. Sirolimus and paclitaxel provoke different vascular pathologic responses after local delivery in a murine model for restenosis on underlying atherosclerotic arteries. Heart. 2007;93:922–927. | |
Dake MD, Ansel GM, Jaff MR, et al. Paclitaxel-eluting stents show superiority to balloon angioplasty and bare metal stents in femoropopliteal disease: twelve-month Zilver PTX randomized study results. Circ Cardiovasc Interv. 2011;4:495–504. | |
Dake MD, Ansel GM, Jaff MR, et al. Sustained safety and effectiveness of paclitaxel-eluting stents for femoropopliteal lesions: 2-year follow-up from the Zilver PTX randomized and single-arm clinical studies. J Am Coll Cardiol. 2013;61:2417–2427. | |
Ansel G. PTX Randomized Trial of Paclitaxel-Eluting Stents for Femoropopliteal Artery Disease: 4-Year Results. Paper presented at: Vascular Interventional Advances; October 8, 2013; Las Vegas, NV. | |
Zeller T, Dake MD, Tepe G, et al. Treatment of femoropopliteal in-stent restenosis with paclitaxel-eluting stents. JACC Cardiovasc Interv. 2013;6:274–281. | |
Abularrage CJ, Conrad MF, Hackney LA, et al. Long-term outcomes in diabetic patients undergoing endovascular infrainguinal interventions. J Vasc Surg. 2010;52(2):314–322. | |
Sabeti S, Mlekusch W, Amighi J, Minar E, Schillinger M. Primary patency of long-segment self-expanding nitinol stents in the femoropopliteal arteries. J Endovasc Ther. 2005;12(1):6–12. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.