Back to Journals » OncoTargets and Therapy » Volume 7
Critical appraisal of sorafenib in the treatment of Chinese patients with renal cell carcinoma
Received 9 August 2013
Accepted for publication 4 November 2013
Published 6 June 2014 Volume 2014:7 Pages 925—935
DOI https://doi.org/10.2147/OTT.S41828
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Ding-Wei Ye, Hai-Liang Zhang
1Department of Urology, Fudan University Shanghai Cancer Center, 2Department of Oncology, Shanghai Medical College, Fudan University, Shanghai, People's Republic of China
Abstract: Renal cell carcinoma (RCC) accounts for 3% of all malignancies, and is the most aggressive cancer of the genitourinary system. Metastatic RCC is naturally resistant to chemotherapy and radiotherapy, and immunotherapy is of little benefit. In recent years, the emergence of molecular-targeted therapies has largely changed the therapeutic approach to metastatic RCC. These novel multikinase inhibitors have now become first-choice therapy because of their activity in inhibiting both cell proliferation and tumor angiogenesis. Sorafenib is the first tyrosine kinase inhibitor found to be effective in treating patients with metastatic RCC. Due to its good efficacy and safety, this agent is recommended as both first-line and second-line therapy for metastatic RCC in the People's Republic of China. Sorafenib seems to be more effective in patients of Chinese ethnicity than in western patients, and is well tolerated with a manageable toxicity profile, even at higher dosages and when used in combination with other anticancer agents. Novel biomarkers for predicting the efficacy of sorafenib have potential clinical value for guiding individualized targeted therapy.
Keywords: kidney cancer, renal cell carcinoma, sorafenib, tyrosine kinase inhibitor
Introduction
Renal cell carcinoma (RCC) is the third most common malignancy of the genitourinary system, accounting for about 3% of all adult malignancies and 2% of all cancer deaths.1 In the People’s Republic of China, the incidence of RCC has increased significantly in the past 10 years, and is currently estimated to be six per 100,000 people per year. Around 78,000 new cases occur each year, of which 19,500 (25%) are at a late stage and 20,000 deaths occur each year due to this cancer.2 In Shanghai, the incidence of RCC reached 14.2 per 100,000 people in 2009, and became the ninth most common malignancy in men.3
RCC is highly resistant to chemotherapy, and its response to cytokine therapy, including high-dose interleukin-2 and/or interferon-alpha, is less than 20%.4 Moreover, the toxicity of cytokine therapy, particularly interleukin-2, makes this treatment only appropriate for a small number of selected cases. For decades, the outcome for patients with metastatic disease was dismal, and the 5-year overall survival rate was less than 10%, despite systemic treatment.5
Recently, treatment strategies for metastatic RCC have changed dramatically due to the introduction of several new agents targeting tumor angiogenesis and intracellular pathways mediating growth and proliferation. Among these agents are tyrosine kinase inhibitors such as sorafenib, sunitinib, pazopanib, and axitinib; mammalian target of rapamycin (mTOR) inhibitors such as temsirolimus and everolimus; and the anti-vascular endothelial growth factor (VEGF) monoclonal antibody bevacizumab, usually given in combination with interferon.6
Sorafenib (Nexavar®, Bayer Healthcare Pharmaceuticals, Wayne, NJ, USA, and Onyx Pharmaceuticals, South San Francisco, CA, USA) is a multi-targeting tyrosine kinase inhibitor against VEGF receptors, platelet-derived growth factor receptors, Fms-like tyrosine kinase 3, RET, and KIT, as well as the RAF serine/threonine kinases B-RAF and C-RAF.7 The efficacy of sorafenib in RCC has been confirmed in Phase II and Phase III trials, leading to its approval by the US Food and Drug Administration in December 2005 as the first targeted agent to show clinical activity in RCC.6,9,10 Ten months later, sorafenib was approved by the State Food and Drug Administration in the People’s Republic of China as first-line/second-line treatment for advanced RCC. This paper reviews the available data on the efficacy, safety, and clinical application status of sorafenib in Chinese patients with RCC.
Efficacy of sorafenib as first/second- line treatment after cytokine therapy in advanced RCC
Since December 2006, more than 4,000 Chinese patients with advanced RCC have received sorafenib. Because most patients in the People’s Republic of China cannot afford the cost of continued sorafenib treatment, in April 2007, the China Charity Federation accepted donations from Bayer Healthcare Products Co, Ltd and established the Nexavar (sorafenib) patient assistance program to enable more patients with advanced RCC to have access to sorafenib. As of May 2013, over 3,000 patients have been enrolled in this program. After 3 months of treatment, patients who fit this program are able to receive free sorafenib until progression of their disease.
Most of the data on sorafenib in Chinese patients with RCC have been reported retrospectively in local medical journals, and only four studies have been published in non-Chinese language journals or as abstracts of papers presented at American Society of Clinical Oncology meetings. In the first of these studies, Sun et al10 reported the results of an open-label, multicenter, noncontrolled, investigator-initiated trial in Chinese patients with advanced RCC. The clinical benefit rate (complete response + partial response + stable disease) was 84.2% in the 57 patients evaluated, and the objective response rate (complete response + partial response) was 21%. Median progression-free survival was up to 41 weeks, but median overall survival was not reached after a mean follow-up period of 40 weeks. Subsequently, in 2009, Zhang et al11 reported similar results in a study of 98 patients treated at two major centers in Shanghai. Radiologically-confirmed complete response, partial response, stable disease, and progressive disease were observed in one (1%), 23 (23.5%), 62 (63.3%), and 12 (12.2%) patients, respectively. Median progression-free survival was 60 weeks, but median overall survival was not reached after a follow-up period of 76 weeks.
In 2012, Yang et al12 reported the outcome of sorafenib therapy in Chinese patients with advanced RCC and from Wuhan, the middle region of the People’s Republic of China. Among the 30 patients treated, one had a complete response (3.3%), four had a partial response (13.3%), 19 had stable disease (63.3%), and six had progressive disease (20%). The clinical benefit rate (complete response + partial response + stable disease) was 80%, median progression-free survival was 14 months, and median overall survival was 16 months. Most recently, Guo et al13 provided data from patients with RCC in the northeastern region of the People’s Republic of China. Among the 131 patients who were available for the survival analysis, median progression-free survival and overall survival were 10.5 months and 16.1 months, respectively. Comparison of the efficacy data for sorafenib in Chinese patients with data from western patients reported in the Phase III TARGET (Treatment Approach in Renal Cancer Global Evaluation Trial) study7 shows that the objective response rate (complete response + partial response) was higher in Chinese patients and progression-free survival seemed much longer, although the clinical benefit rate (complete response + partial response + stable disease) was similar. The ARCCS (Advanced Renal Cell Carcinoma Sorafenib) program made sorafenib available to patients with advanced RCC before regulatory approval in the US/Canada (NA-ARCCS)14 and European countries (EU-ARCCS),15 and the efficacy results were consistent with the TARGET population, as shown in Table 1.
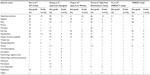
As sorafenib was recommended as one of the first-line treatments for advanced RCC according to the Chinese guideline for RCC, some of the patients in the four studies had not previously received cytokine therapy. In the study reported by Zhang et al,11 the efficacy of sorafenib was similar regardless of whether patients had received it as first-line treatment or second-line treatment after cytokine therapy. These favorable outcomes in both objective response rate and survival confirmed the efficacy of sorafenib in Chinese patients with advanced RCC. Different efficacy profiles of other targeted agents (sunitinib, pazopanib, and everolimus) between Asian and western populations are listed in Table 2,16–21 and it is difficult to determine the underlying mechanisms for these differences.
A potential explanation for the seemingly greater efficacy of sorafenib in Chinese patients than in western patients may be the inherent differences between ethnic Chinese and other ethnic groups. Data from other areas of Asia, such as Japan22,23 and Korea,24 have also shown better clinical outcomes in patients with advanced RCC treated using sorafenib in comparison with western patients. Differences in expression of tumor markers and molecular features in patients from different ethnic groups have been well documented for a number of malignancies, including lung cancer, prostate cancer, breast cancer, and astrocytoma,25–29 and it has been demonstrated that RCC may have different characteristics and behavior in different ethnic groups.30 However, whether ethnicity and associated differences in molecular features are the major reason for the observed differences in the efficacy of sorafenib needs further investigation. A possible solution may be found by use of gene-profiling technologies to detect differences between patients from different ethnic backgrounds and different responses to sorafenib. Single nucleotide polymorphisms in VEGF, VEGF receptors, fibroblast growth factor receptors, and the ABCB1 gene have been found to be correlated with treatment of advanced RCC;31,32 however, there is no such evidence for sorafenib in RCC. Studies of hepatocellular carcinoma have shown that specific single nucleotide polymorphisms in organic cation transporter-1 might reduce sorafenib uptake and responsiveness,33 and a similar mechanism may also occur in patients with RCC. Therefore, some answers may be obtained by comparing these potential single nucleotide polymorphisms between different ethnic groups.
Sorafenib as second-line treatment after prior sunitinib therapy
In a multicenter, randomized, open-label trial, Qin et al34 compared the progression-free survival times achieved with axitinib and sorafenib administered as second-line treatments. A total of 204 Asian patients with metastatic RCC were randomly assigned (2:1) to 28-day cycles of axitinib 5 mg twice daily or sorafenib 400 mg twice daily; 135 patients received axitinib and 69 received sorafenib. Prior therapy included sunitinib (45%) or cytokines (53%). The objective response rate was 23.7% with axitinib and 10.1% with sorafenib, and median progression-free survival was 6.4 months with axitinib and 4.8 months with sorafenib, which is quite similar to the findings of the AXIS (Comparative effectiveness of axitinib versus sorafenib in advanced renal cell carcinoma) study in which a median progression-free survival of 6.7 months was reported with axitinib and 4.7 months with sorafenib.35 However, in a recent update of data from the AXIS study,36 axitinib did not prove to be superior to sorafenib in the analysis of overall survival; median overall survival was 20.1 months (95% confidence interval [CI] 16.7–23.4) with axitinib and 19.2 months (95% CI 17.5–22.3) with sorafenib (P=0.3744). As a result of these data and the National Comprehensive Cancer Network guideline for RCC, sorafenib remains a treatment option for patients with treatment failure on sunitinib.
Adverse effects of sorafenib in Chinese patients
A systematic review of the adverse effects of sorafenib in western patients was conducted by Bhojani et al.37 Hand-foot skin reaction, rash, alopecia, mucositis, diarrhea, hypertension, fatigue, hypophosphatemia, and weight loss were the most commonly reported toxicities.38 Grade 3 or 4 toxicities (which have included hypophosphatemia) are uncommon.
The most common adverse events observed with sorafenib in the studies of Chinese patients are shown in Table 3. The overall incidence of adverse events with sorafenib has ranged from <1% to 80%, and that of grade 3/4 toxicity from <1% to 24%. In comparison with data for western patients reported in the TARGET study,7 Chinese patients seem to experience more hand-foot skin reaction and alopecia. However, these two adverse effects are not fatal and have always been manageable, even in outpatients. A higher incidence of hand-foot skin reaction was also seen in the sorafenib Asian-Pacific trial in patients with hepatocellular carcinoma. Therefore, Chinese patients may be more prone to the hand-foot skin reaction caused by sorafenib. In several pooled safety analyses of sorafenib in the treatment of solid tumors, including RCC, the severity of the skin reaction and was statistically correlated with the time to progression.39–41
In the study by Zhang et al9 in Chinese patients with metastatic RCC, grade 3 and 4 toxicities were observed in 35.7% of patients, and only nine (9.2%) terminated their treatment because of drug-related adverse events. In A-PREDICT (A Phase II Study Of Axitinib In Metastatic Renal Cell Cancer in Patients Unsuitable for Nephrectomy), Ye et al42 investigated the safety and efficacy of sorafenib in a large subset of Asian patients (n=1,092, including 1,033 from the People’s Republic of China) in daily clinical practice. Drug-related adverse events were experienced by 35% of patients, the most frequent being hand-foot skin reaction (21%), diarrhea (7%), rash (7%), alopecia (5%), and hypertension (3%). Serious drug-related adverse events were seen in less than 2% of all patients, and only 3% discontinued sorafenib due to drug-related adverse events. These results indicate that sorafenib is well tolerated by Chinese patients with RCC.
Cardiotoxicity is seldom reported in patients treated with sorafenib. Sun et al10 noted palpations in 17% of sorafenib-treated patients, while Zhang et al11 reported one case of angina on a combination of sorafenib and interferon therapy; however, no angina events occurred with sorafenib alone.
Bleeding events related to sorafenib have occurred in some Chinese patients, although not in western patients treated in the TARGET study.7 Digestive tract hemorrhage (4%), nasal or mucocutaneous hemorrhage (9%), hematuria (4%), and hemoptysis (14%) were observed in the study by Zhang et al.11 Although uncommon, hemorrhagic events could be lethal, so careful clinical monitoring is necessary. Treatment with sorafenib should be suspended if gross bleeding appears, and should not be resumed until it has abated.
Neoadjuvant and adjuvant sorafenib therapy in Chinese patients
Neoadjuvant and adjuvant treatments in RCC are not evidenced-based and still experimental
Neoadjuvant therapy is usually used to downstage locally advanced tumors and to improve survival in other malignancies, such as breast cancer and rectal cancer. However, its application in RCC has been limited, due to the minor responses achieved with targeted agents in primary kidney tumors.43 Moreover, the toxicity associated with targeted therapy, such as diarrhea, hypertension, fatigue, weight loss, and coagulopathy, may affect subsequent surgical treatment, and patients may experience more perioperative complications.44 In a study of sorafenib, Cowey et al45 evaluated the safety and feasibility of neoadjuvant therapy in the preoperative setting, and observed a median decrease of 9.6% in the size of primary tumors. Thus, preoperative sorafenib therapy appears to be safe and feasible, and has the potential to reduce the size and density of primary kidney tumors. Unfortunately, there are no serial studies of the preoperative use of targeted therapy in Chinese patients with locally advanced RCC, although several case reports in Chinese medical journals have provided data, albeit limited, on the use of such therapy in the neoadjuvant setting.
The adjuvant use of targeted therapy after resection of localized RCC is being investigated in view of the expectation that earlier targeted therapy interventions can decrease the incidence of recurrence and metastasis, and therefore increase the cure rate for localized RCC. Two Phase III clinical trials are ongoing to determine the potential role of sorafenib in the adjuvant setting. The primary endpoint for both studies is disease-free survival. One of these studies, the ASSURE (Adjuvant Sorafenib or Sunitinib for Unfavorable Renal Carcinoma) trial, compares sorafenib twice daily continuously, sunitinib once daily for 4 weeks on and 2 weeks off, and placebo in patients with resectable localized RCC,46 while the other, the SORCE (Sorafenib in Treating Patients at Risk of Relapse After Undergoing Surgery to Remove Kidney Cancer) trial, compares adjuvant sorafenib for one year, adjuvant sorafenib for 3 years, and placebo in patients with a high or intermediate risk of relapse after complete resection of kidney tumors.47 As yet, no strong evidence-based data are available from either of these studies.
Other Phase II clinical trials of adjuvant sorafenib or sunitinib have been reported recently. Zhao et al48 evaluated the efficacy and safety of targeted agents (sorafenib and sunitinib) as postoperative adjuvant therapy in Chinese patients with clear-cell RCC who were at high risk of disease recurrence. In this study, patients who received either sorafenib (n=20) or sunitinib (n=23) for one year were compared with 388 patients at high risk of disease recurrence who did not receive adjuvant therapy. The recurrence rate in the sorafenib and sunitinib groups was not significantly different (15% and 17.4%, respectively), but was lower than in the control group (38.7%). Disease-free survival was significantly longer in the sorafenib and sunitinib groups than in the control group (18.9±5.9 months and 16.9±6.1 months, respectively, versus 13.3±7.2 months). This study provides preliminary evidence of the efficacy of adjuvant sorafenib therapy after radical nephrectomy in Chinese patients, and suggests that sorafenib might have the potential to decrease the recurrence rate and prolong disease-free survival in high-risk patients in this setting. However, the sample size of this study was rather small and the control group was an historical population, which made it insufficient to support clinical decision-making.
Dose escalation of sorafenib after failure of treatment at regular dosages
In 2009, Si et al48 performed a preliminary study of sorafenib dosage escalation after failure of conventional dosages in Chinese patients with metastatic RCC. An increase in the sorafenib dosage from 800 mg daily to 1,200 mg or 1,600 mg daily achieved an objective response (complete response + partial response) rate of 44% (7/16), and a disease control rate (complete response + partial response + stable disease) of 81% (13/16). In another study, Zhang et al49 reported the results for dose escalation of sorafenib to 600 mg twice daily or 800 mg twice daily after failure of treatment at regular dosages in 24 Chinese patients. The disease control rate achieved in this study was 83.3% and median progression-free survival was 5 months. Adverse effects were only slightly increased in these patients. A large, globally-driven, dose-escalation study of sorafenib was also performed in 83 patients.51 A dosage of sorafenib escalated above 400 mg twice daily appeared to contribute greater clinical benefit. However, dose escalation per protocol was not feasible for the majority of patients. In 2012, Amato et al52 reported the efficacy and toxicity of escalated doses of sorafenib in patients with metastatic RCC. In 44 patients who received sorafenib at dosages of 600–800 mg twice daily, the objective response (complete response + partial response) rate reached 55% (24/44), and median progression-free survival was 8.43 months. The higher dosage of sorafenib led to better disease control without a significant increase in adverse effects. In the People’s Republic of China, most patients treated with sorafenib are enrolled into the patient assistance program after 3 months and obtain free treatment from the China Charity Federation. If disease progression occurs, patients who have tolerated regular dosages of sorafenib well can be considered for a dosage increase to 600 mg twice daily, still at no charge. Larger studies to verify the efficacy of sorafenib dose escalation are planned.
Combination strategies using sorafenib with other anticancer agents
Although single-agent use of sorafenib has demonstrated a survival benefit in patients with metastatic RCC, few patients are cured and most patients will eventually become resistant to it. In other malignancies, combination chemotherapy regimens consisting of drugs with different antitumor activity are commonly used, but whether combinations of sorafenib and other anticancer agents are able to improve the efficacy of treatment needs to be investigated. Several clinical trials of sorafenib in combination with cytokines, gemcitabine, capecitabine, bevacizumab, temsirolimus, everolimus, panobinostat, or vorinostat have been conducted.
Full-dose sorafenib plus interferon was found to be feasible in a Phase I study,53 and two Phase II studies have shown that this combination increases response rates but not progression-free survival or overall survival.54,55 A randomized Phase II trial of sorafenib plus two different doses of interferon has been investigated. Bracarda et al reported that sorafenib plus frequent low-dose interferon (3 mU five times a week) showed good efficacy and tolerability, and interestingly, a 6% complete response rate was reported with this intriguing regimen, while in 2011, Procopio et al56 reported that a combination of sorafenib and interleukin-2 (4.5 mU five times a week) did not demonstrate improved efficacy versus sorafenib alone. In a Phase IV trial of first-line therapy with sorafenib in combination with interferon in Chinese patients, Huang et al57 found that the objective response rate reached 32.8% (45/137), which was higher than the response rate achieved with single-agent sorafenib in other studies, but adverse effects were significantly increased with this combination regimen.
Bevacizumab and temsirolimus are being investigated in combination with sorafenib in patients with advanced RCC in the BEST (Bevacizumab, Sorafenib Tosylate, and Temsirolimus in Treating Patients With Metastatic Kidney Cancer) trial.58 This four-arm, randomized, Phase II study compares bevacizumab alone and in combination with temsirolimus or sorafenib and also a combination of sorafenib plus temsirolimus. Although the study aimed to detect a 67% improvement in median progression-free survival in the three combination therapy arms in comparison with single-agent bevacizumab, none of the combination regimens achieved this primary endpoint. Median progression-free survival was 8.7 months with bevacizumab alone as compared with 7.3 months for bevacizumab plus temsirolimus (hazards ratio 0.91, 95% CI 0.68–1.23), 11.3 months for bevacizumab plus sorafenib (hazards ratio 0.84, 95% CI 0.62–1.13), and 7.7 months for sorafenib plus temsirolimus (hazards ratio 1.11, 95% CI 0.83–1.49). Objective response rates (complete response + partial response) were 12% for bevacizumab single-agent therapy versus 28% for bevacizumab plus temsirolimus, 30% for bevacizumab plus sorafenib, and 27% for sorafenib plus temsirolimus. Although bevacizumab plus sorafenib achieved the longest progression-free survival and highest response rate, no statistically significant differences between the four study arms were found. Common toxicities included hypertension, fatigue, hand-foot syndrome, and diarrhea. Grade 3/4 adverse events and dose reductions were more common in the combination therapy arms. In the People’s Republic of China, combination therapy with sorafenib plus bevacizumab is mostly applied as second-line treatment in patients who have failed first-line tyrosine kinase inhibitor therapy. Preliminary results from a Phase II clinical trial of 24 patients who received this combination (including 16 who had failed on single-agent sorafenib, six who had failed on sunitinib, and two who had failed on pazopanib) have been reported by Sheng et al.59 Sorafenib was given at a dosage of 400 mg twice daily and bevacizumab at a dosage of 5 mg/kg every 2 weeks. The objective response (complete response + partial response) rate was 16.8% (4/24), the disease control rate (complete response + partial response + stable disease) was 70.8% (17/24), and median progression-free survival was 7 months. However, the efficacy of sorafenib plus bevacizumab needs to be further verified before its widespread clinical use is contemplated.
The outcomes of combination regimens of sorafenib and cytotoxic agents in Chinese patients with RCC were reported at the 2013 American Society of Clinical Oncology meeting. Guo et al60 conducted a multicenter Phase II clinical trial to investigate the efficacy in terms of overall response rate and progression-free survival achieved with a combination of gemcitabine, fluorouracil, and sorafenib as first-line treatment in Chinese patients with metastatic RCC. The regimen consisted of intravenous gemcitabine 800 mg/m2 (days 1 and 15) and fluorouracil 1,250 mg/m2 by continuous intravenous infusion over 48 hours (days 1 and 15) every 28-day cycle, plus oral sorafenib 400 mg twice daily (days 1–28) for four cycles, followed by sorafenib monotherapy. In 52 patients who received this regimen, partial response and stable disease were achieved in 23 patients (44%) and 28 patients (54%), respectively, and the disease control rate was 98%. The 6-month progression-free survival rate was 56.25%, but median progression-free survival was not reached. Most adverse events were grade 1 or 2, and included hand-foot skin reaction (n=32), rash (n=24), diarrhea (n=23), fatigue (n=13), and hypertension (n=4). Grade 3 adverse events included hand-foot skin reaction (n=8), neutropenia (n=13), thrombocytopenia (n=1), and pulmonary edema (n=1). These preliminary results suggest that sorafenib in combination with gemcitabine and fluorouracil may improve response rates and progression-free survival in Chinese patients, with acceptable adverse effects. Guo et al61 also investigated anti-VEGF drugs combined with gemcitabine-based chemotherapy in metastatic collecting duct carcinoma. Four patients received sorafenib (400 mg twice daily) and two received sunitinib (37.5 mg once daily), both in combination with gemcitabine (1.0 g/m2 on days 1 and 8) and cisplatin (40 mg on days 1–3) every 28 days. One patient achieved a partial response and four had stable disease, with a disease control rate of 83.3% (5/6). Median progression-free survival and overall survival were 3.5 months and 6.5 months, respectively. Grade 3–4 toxicities included neutropenia (4/6), thrombocytopenia (2/6), hand-foot syndrome (1/6), and rash (1/6). Although collecting duct carcinoma accounts for less than 1% of kidney cancers, it is highly aggressive with an extremely poor prognosis, and there is currently no standard treatment for this disease. Nevertheless, this small-sample trial has demonstrated modest antitumor activity of sorafenib plus gemcitabine and cisplatin in collecting duct carcinoma.
Prognostic and predictive biomarkers for the efficacy of sorafenib
A number of clinical and pathologic markers, such as prior nephrectomy, anemia, serum calcium level, lactate dehydrogenase, Karnofsky performance status, number of metastatic sites, blood neutrophil levels, and blood platelet levels have all been demonstrated to be of prognostic value in patients with metastatic RCC treated with targeted drugs.62 Given that there are few definitive biomarkers for predicting the efficacy and toxicity of targeted agents, identifying potential predictive and surrogate biomarkers in patients receiving sorafenib and other targeted agents remains an area of active investigation. A retrospective univariate analysis of baseline plasma samples collected in a cohort of the TARGET trial7 suggested that VEGF (P=0.0024), carbonic anhydrase IX (P=0.034), tissue inhibitor of metalloproteinase-1 (P=0.001), and RAS p21 (P=0.016) may be prognostic biomarkers for overall survival. Further, tissue inhibitor of metalloproteinase-1 remained prognostic for survival in a multivariate analysis (P=0.002).63
Several Chinese investigators have made contributions towards identifying predictive biomarkers for sorafenib treatment. Recent studies have indicated that hypertension and obesity predict a longer progression-free survival with targeted therapy.64,65 In a study of 77 patients with metastatic RCC treated with sorafenib or sunitinib, Chi et al66 found that patients with primary hypertension had a longer median progression-free survival than those with normal baseline blood pressure (14.0 months versus 9.5 months, P=0.01), and in a multivariable analysis, primary hypertension was an independent predictor of progression-free survival. Mao et al67 tested the polymorphisms in hypertension-associated genes (angiotensinogen and VEGF) and obesity-associated genes (apolipoprotein E), and showed that a polymorphism in the promoter of the angiotensinogen gene (rs2493137) might be associated with a better clinical outcome in patients treated with sorafenib.
In another study, Guo et al68 used CXCR4 (a chemokine receptor) to predict the efficacy of sorafenib in patients with metastatic RCC. CXCR4 is implicated in the process of metastasis in RCC, and previous studies have shown that higher expression of CXCR4 predicts a higher rate of metastasis and a poorer prognosis in patients with localized RCC. In 58 patients with metastatic RCC who were treated with targeted drugs (26 with sorafenib, 23 with sunitinib, five with pazopanib, two with CCI-779, and two with axitinib) as first-line therapy, the progression-free survival of sorafenib-treated patients with negative or low CXCR4 expression was 20.0±8.0 months, while the progression-free survival of patients with intermediate or high CXCR4 expression was 6.0±0.8 months (P=0.038). However, no such correlation was found in the group of patients treated with sunitinib (P=0.947). Thus, CXCR4 has a potential role in predicting progression-free survival in patients treated with sorafenib.
Serum erythrocyte sedimentation rate (ESR) was measured by Zhang et al69 in 83 patients with metastatic clear-cell RCC. Forty-three (41%) patients had an ESR higher than 40 mm/hour. Median progression-free survival was 27 months in the decreased ESR group, 12 months in the stable ESR group, and 6 months in the increased ESR group. ESR was an independent predictor for progression-free survival in a multivariate Cox regression model analysis, indicating that a dynamic change in ESR could be useful for monitoring the treatment response and predicting progression-free survival in patients with metastatic RCC treated with sorafenib as second-line therapy. Zhang et al70 also measured c-KIT expression in 17 patients with metastatic sarcomatoid RCC treated with sorafenib, and found that c-KIT-positive patients had a higher disease control rate than c-KIT-negative patients (75% versus 25%, respectively, P=0.036). Median overall survival time was 92 weeks for c-KIT-positive patients and 44 weeks for c-KIT-negative patients (P=0.002). A multivariate Cox regression model analysis revealed that only number of metastatic organs and c-KIT were independent prognostic factors.
The abovementioned biomarkers are summarized in Table 4.
Conclusion
Sorafenib is the first oral multikinase inhibitor to be approved by the Chinese State Food and Drug Administration for the treatment of patients with advanced RCC. The findings of the studies reviewed in this paper indicate that sorafenib can be used as both first-line and second-line treatment for Chinese patients with RCC. Sorafenib seems to be more effective in Chinese patients than in western patients, but causes relatively higher rates of some adverse effects in Chinese patients. Studies in Chinese patients have indicated that sorafenib can also be used safely at higher dosages and in combination with other anticancer agents. Overall, this targeted agent is well tolerated with a manageable toxicity profile, even at higher dosages and when used together with other agents. Ongoing research with sorafenib may encourage its use in new strategies for the treatment of RCC. Further, novel biomarkers may be used to predict the efficacy of sorafenib and guide individualized targeted therapy.
Disclosure
The authors report no conflicts of interest in this work.
References
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63(1):11–30. | |
Hao J, Chen WQ. 2012 Annual Report of Cancer Registration in China. Beijing, the People’s Republic of China: Military Medical Science Press; 2012. | |
Shanghai Cancer Institute. 2009 Cancer incidence in downtown Shanghai. Tumor. 2012;32(10):964. | |
Law TM, Motzer RJ, Mazumdar M, et al. Phase III randomized trial of interleukin-2 with or without lymphokine-activated killer cells in the treatment of patients with advanced renal cell carcinoma. Cancer. 1995;76(5):824–832. | |
Rini BI, Campbell SC, Escudier B. Renal cell carcinoma. Lancet. 2009;373(9669):1119–11132. | |
Singer EA, Gupta GN, Srinivasan R. Update on targeted therapies for clear cell renal cell carcinoma. Curr Opin Oncol. 2011;23(3):283–289. | |
Escudier B, Eisen T, Stadler WM, et al. Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med. 2007;356(2):125–134. | |
Strumberg D. Sorafenib for the treatment of renal cancer. Expert Opin Pharmacother. 2012;13:407–419. | |
Porta C, Paglino C, Imarisio I, Ferraris E. Sorafenib tosylate in advanced kidney cancer: past, present and future. Anticancer Drugs. 2009;20(6):409–415. | |
Sun Y, Na Y, Yu S, et al. Sorafenib in the treatment of Chinese patients with advanced renal cell cancer. J Clin Oncol. 2008;26 Suppl: Abstr 16127. | |
Zhang H, Dong B, Lu JJ, et al. Efficacy of sorafenib on metastatic renal cell carcinoma in Asian patients: results from a multicenter study. BMC Cancer. 2009;9:249. | |
Yang L, Shi L, Fu Q, et al. Efficacy and safety of sorafenib in advanced renal cell carcinoma patients: results from a long-term study. Oncol Lett. 2012;3(4):935–939. | |
Guo F, Xie XD, Liu ZZ, et al. Prognostic analysis of Chinese patients with metastatic renal cell cancer (mRCC) receiving sorafenib: a multicenter retrospective study. J Clin Oncol. 2013;31 Suppl: Abstr e15582. | |
Walter M, Stadler MD, Robert A, et al. Safety and efficacy results of the advanced renal cell carcinoma sorafenib expanded access program in North America. Cancer. 2010;116(5):1272–1280. | |
Beck J, Procopio G, Bajetta E, et al. Final results of the European Advanced Renal Cell Carcinoma Sorafenib (EU-ARCCS) expanded-access study: a large open-label study in diverse community settings. Ann Oncol. 2011;22(8):1812–1823. | |
Qin SK, Jin J, Guo J, et al. Sunitinib as 1st line treatment in Chinese advance mRCC patients: a multi-center clinical study. Abstract Z006 presented at the Annual Meeting of the Chinese Society of Clinical Oncology, September 19–23, 2012, Beijing, People’s Republic of China. | |
Motzer RJ, Hutson TE, Tomczak P, et al. Overall survival and updated results for sunitinib compared with interferon alfa in patients with metastatic renal cell carcinoma. J Clin Oncol. 2009;27(22):3584–3590. | |
Motzer RJ, Hutson TE, Cella D, et al. Pazopanib versus sunitinib in metastatic renal-cell carcinoma. N Engl J Med. 2013;369(8):722–731. | |
Sternberg CN, Davis ID, Mardiak J, et al. Pazopanib in locally advanced or metastatic renal cell carcinoma: results of a randomized phase III trial. J Clin Oncol. 2010;28(6):1061–1068. | |
Guo J, Huang Y, Zhang X, et al. Safety and efficacy of everolimus in Chinese patients with metastatic renal cell carcinoma resistant to vascular endothelial growth factor receptor-tyrosine kinase inhibitor therapy: an open-label phase 1b study. BMC Cancer. 2013;13:136. | |
Motzer RJ, Escudier B, Oudard S, et al. Phase 3 trial of everolimus for metastatic renal cell carcinoma: final results and analysis of prognostic factors. Cancer. 2010;116(18):4256–4265. | |
Akaza H, Tsukamoto T, Murai M, et al. Phase II study to investigate the efficacy, safety, and pharmacokinetics of sorafenib in Japanese patients with advanced renal cell carcinoma. Jpn J Clin Oncol. 2007;37(10):755–762. | |
Naito S, Tsukamoto T, Murai M, et al. Overall survival and good tolerability of long-term use of sorafenib after cytokine treatment: final results of a phase II trial of sorafenib in Japanese patients with metastatic renal cell carcinoma. BJU Int. 2011;108(11):1813–1819. | |
Park SJ, Lee JL, Park I, et al. Comparative efficacy of sunitinib versus sorafenib as first-line treatment for patients with metastatic renal cell carcinoma. Chemotherapy. 2012;58(6):468–474. | |
Bell DW, Brannigan BW, Matsuo K, et al. Increased prevalence of EGFR-mutant lung cancer in women and in East Asian populations: analysis of estrogen-related polymorphisms. Clin Cancer Res. 2008;14(13):4079–4084. | |
Mu XL, Li LY, Zhang XT, et al. Gefitinib-sensitive mutations of the epidermal growth factor receptor tyrosine kinase domain in Chinese patients with non-small cell lung cancer. Clin Cancer Res. 2005;11(12):4289–4294. | |
Weston MK, Moss DP, Stewart J, et al. Differences in breast cancer biological characteristics between ethnic groups in New Zealand. Breast Cancer Res Treat. 2007;11(3):555–558. | |
Chen P, Aldape K, Wiencke JK, et al. Ethnicity delineates different genetic pathways in malignant glioma. Cancer Res. 2001;61(10):3949–3954. | |
Wiencke JK, Aldape K, McMillan A, et al. Molecular features of adult glioma associated with patient race/ethnicity, age, and a polymorphism in O6-methylguanine-DNA-methyltransferase. Cancer Epidemiol Biomarkers Prev. 2005;14(7):1774–1783. | |
Stafford HS, Saltzstein SL, Shimasaki S, et al. Racial/ethnic and gender disparities in renal cell carcinoma incidence and survival. J Urol. 2008;179(5):1704–1708. | |
Beuselinck B, Karadimou A, Lambrechts D, et al. Single-nucleotide polymorphisms associated with outcome in metastatic renal cell carcinoma treated with sunitinib. Br J Cancer. 2013;108(4):887–900. | |
Kim JJ, Vaziri SA, Rini BI, et al. Association of VEGF and VEGFR2 single nucleotide polymorphisms with hypertension and clinical outcome in metastatic clear cell renal cell carcinoma patients treated with sunitinib. Cancer. 2012;118(7):1946–1954. | |
Herraez E, Lozano E, Macias RI, et al. The expression of SLC22A1 variants may affect the response of hepatocellular carcinoma and cholangiocarcinoma to sorafenib. Hepatology. 2013;58(3):1065–1073. | |
Qin SQ, Bi F, Cheng Y, et al. Axitinib versus sorafenib as second-line therapy in Asian patients with metastatic renal cell carcinoma (mRCC): results from a registrational study. J Clin Oncol. 2012;30 Suppl: Abstr LBA4537. | |
Rini BI, Escudier B, Tomczak P, et al. Comparative effectiveness of axitinib versus sorafenib in advanced renal cell carcinoma (AXIS): a randomised phase 3 trial. Lancet. 2011;378(9807):1931–1939. | |
Motzer RJ, Escudier B, Tomczak P, et al. Axitinib versus sorafenib as second-line treatment for advanced renal cell carcinoma: overall survival analysis and updated results from a randomised phase 3 trial. Lancet Oncol. 2013;14(6):552–562. | |
Bhojani N, Jeldres C, Patard JJ, et al. Toxicities associated with the administration of sorafenib, sunitinib, and temsirolimus and their management in patients with metastatic renal cell carcinoma. Eur Urol. 2008;53(5):917–930. | |
Gollob JA, Rathmell K, Richmond TM, et al. Phase II trial of sorafenib plus interferon alfa-2b as first- or second-line therapy in patients with metastatic renal cell cancer. J Clin Oncol. 2007;25(22):3288–3295. | |
Cheng AL, Kang YK, Chen Z, et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10(1):25–34. | |
Llovet JM, Ricci S, Mazzaferro V, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359(4):378–390. | |
Strumberg D, Awada A, Hirte H, et al. Pooled safety analysis of BAY 43-9006 (sorafenib) monotherapy in patients with advanced solid tumors: is rash associated with treatment outcome? Eur J Cancer. 2006;42(200):548–556. | |
Ye DW, Guo J, Lee JL, et al. Sorafenib treatment of Asian patients with advanced renal cell carcinoma (RCC) in daily practice: subset analysis of the large non-interventional PREDICT study. J Clin Oncol. 2012; 30 Suppl:Abstr 4628. | |
Shuch B, Riggs SB, LaRochelle JC, et al. Neoadjuvant targeted therapy and advanced kidney cancer: observations and implications for a new treatment paradigm. BJU Int. 2008;102(6):692–696. | |
Amin C, Wallen E, Pruthi RS, et al. Preoperative tyrosine kinase inhibition as an adjunct to debulking nephrectomy. Urology. 2008;72(4):864–868. | |
Cowey CL, Amin C, Pruthi RS, et al. Neoadjuvant clinical trial with sorafenib for patients with stage II or higher renal cell carcinoma. J Clin Oncol. 2010;28(9):1502–1507. | |
Bayer HealthCare Pharmaceuticals Inc. Nexavar® (sorafenib), prescribing information November, 2010. Available from: http://berlex.bayerhealthcare.com/html/products/pi/Nexavar_PI.pdf. Accessed November 6, 2013. | |
ClinicalTrials.gov. Sorafenib in treating patients at risk of relapse after undergoing surgery to remove kidney cancer. ClinicalTrials.gov Identifier NCT00492258. Available from: http://clinicaltrials.gov. Accessed November 6, 2013. | |
Zhao J, Zhu Y, Zhang C, et al. Sorafenib or sunitinib as postoperative adjuvant therapy for Chinese patients with locally advanced clear cell renal cell carcinoma at high risk for disease recurrence. Urol Oncol. May 30, 2012. [Epub ahead of print.] | |
Si L, Ma JH, Zhou AP, et al. Sorafenib escalation treatment for metastatic renal cell carcinoma: preliminary results. Chinese Journal of Urology. 2009;30:18–20. | |
Zhang HL, Ye DW, Yao XD, et al. Clinical evaluation of sorafenib dose escalation after failure to conventional dosage in advanced renal cell carcinoma. Chinese Journal of Urology. 2010;31:24–27. | |
Gore ME, Jones RJ, Ravaud A, et al. Efficacy and safety of intrapatient dose escalation of sorafenib as first-line treatment for metastatic renal cell carcinoma (mRCC). J Clin Oncol. 2011;29 Suppl:Abstr 4609. | |
Amato RJ, Harris P, Dalton M, et al. A phase II trial of intra-patient dose-escalated sorafenib in patients with metastatic renal cell carcinoma. Clin Genitourin Cancer. 2012;10(3):153–158. | |
Escudier B, Lassau N, Angevin E, et al. Phase I trial of sorafenib in combination with IFN alpha-2a in patients with unresectable and/or metastatic renal cell carcinoma or malignant melanoma. Clin Cancer Res. 2007;13(6):1801–1809. | |
Bracarda S, Porta C, Boni C, et al. Could interferon still play a role in metastatic renal cell carcinoma? A randomized study of two schedules of sorafenib plus interferon-alpha 2a (RAPSODY). Eur Urol. 2013;63(2):254–261. | |
Procopio G, Verzoni E, Bracarda S, et al. Sorafenib with interleukin-2 vs sorafenib alone in metastatic renal cell carcinoma: the ROSORC trial. Br J Cancer. 2011;104(8):1256–1261. | |
Ryan CW, Goldman BH, Lara PN Jr, et al. Sorafenib with interferon alpha-2b as first line treatment of advanced renal carcinoma: a phase II study of the Southwest Oncology Group. J Clin Oncol. 2007;25(22):3296–3301. | |
Huang YR, Ma JH, Huang J, et al. Sorafenib in combination with interferon as first-line treatment for advanced renal cell carcinoma: a phase IV clinical trial interim analysis. Chinese Journal of Urology. 2010;31(4):5–7. | |
McDermott DF, Manola J, Pins M, et al. The BEST trial (E2804): a randomized phase II study of VEGF, RAF kinase, and mTOR combination targeted therapy (CTT) with bevacizumab (bev), sorafenib (sor), and temsirolimus (tem) in advanced renal cell carcinoma (RCC). J Clin Oncol. 2013;31 Suppl:Abstr 345. | |
Sheng XN, Guo J. Phase II clinical trial of sorafenib plus bevacizumab as second-line targeted therapy for advanced renal cell carcinoma. Abstract EI005 presented at the annual meeting of the Chinese Society of Clinical Oncology, September 19–23, 2012, Beijing, People’s Republic of China. | |
Guo J, Cui CI, Chen H, et al. Efficacy of sorafenib in combination with gemcitabine and fluorouracil in metastatic renal-cell carcinoma: preliminary result of a multicenter phase II study. J Clin Oncol. 2011; 29 Suppl:Abstr e15042. | |
Guo J, Cui CL, Chi ZH, Si L. Anti-VEGF drugs combined with gemcitabine-based chemotherapy in treatment of metastatic collecting duct carcinoma. J Clin Oncol. 2011;29 Suppl 7:Abstr 403. | |
Patil S, Figlin RA, Hutson TE, et al. Prognostic factors for progression-free and overall survival with sunitinib targeted therapy and with cytokine as first-line therapy in patients with metastatic renal cell carcinoma. Ann Oncol. 2011;22(2):295–300. | |
Peña C, Lathia C, Shan M, et al. Biomarkers predicting outcome in patients with advanced renal cell carcinoma: results from sorafenib phase III Treatment Approaches in Renal Cancer Global Evaluation Trial. Clin Cancer Res. 2010;16(19):4853–4863. | |
Ryanne Wu R, Lindenberg PA, Slack R, et al. Evaluation of hypertension as a marker of bevacizumab efficacy. J Gastrointest Cancer. 2009;40(3–4):101–108. | |
Steffens S, Grünwald V, Ringe KI, et al. Does obesity influence the prognosis of metastatic renal cell carcinoma in patients treated with vascular endothelial growth factor-targeted therapy? Oncologist. 2011;16(11):1565–1571. | |
Chi ZH, Mao LL, Si L, et al. Primary hypertension to predict progression-free survival of target therapy in patients with metastatic renal cell carcinoma. J Clin Oncol. 2012;30 Suppl:Abstr e15052. | |
Mao LL, Si L, Chi ZH, et al. Association of single nucleotide polymorphisms in AGT, VEGF, and apoe genes with clinical outcome of target therapy in advanced renal cell carcinoma. J Clin Oncol. 2012; 30 Suppl:Abstr e15051. | |
Guo J, Tang B, Sheng XN, et al. Use of CXCR4 expression to predict the efficacy of sorafenib treatment in patients with metastatic renal cell carcinoma. J Clin Oncol. 2011;29 Suppl 7:Abstr 359. | |
Zhang HL, Zhu Y, Wang CF, et al. Erythrocyte sedimentation rate kinetics as a marker of treatment response and predictor of prognosis in Chinese metastatic renal cell carcinoma patients treated with sorafenib. Int J Urol. 2011;18(6):422–430. | |
Zhang HL, Zhu Y, Qin XJ, et al. c-KIT: potential predictive factor for the efficacy of sorafenib in metastatic renal cell carcinoma with sarcomatoid feature. Clin Genitourin Cancer. 2013;11(2):134–140. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.