Back to Journals » Journal of Multidisciplinary Healthcare » Volume 14
Cost-Effectiveness of Telemedicine in Asia: A Scoping Review
Authors Salsabilla A , Azzahra AB , Syafitri RIP , Supadmi W, Suwantika AA
Received 4 August 2021
Accepted for publication 14 December 2021
Published 29 December 2021 Volume 2021:14 Pages 3587—3596
DOI https://doi.org/10.2147/JMDH.S332579
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Aisha Salsabilla,1 Alifia B Azzahra,1 Raden IP Syafitri,1 Woro Supadmi,2 Auliya A Suwantika1,3,4
1Department of Pharmacology and Clinical Pharmacy, Faculty of Pharmacy, Universitas Padjadjaran, Bandung, Indonesia; 2Faculty of Pharmacy, Universitas Ahmad Dahlan, Yogyakarta, Indonesia; 3Center of Excellence in Higher Education for Pharmaceutical Care Innovation, Universitas Padjadjaran, Bandung, Indonesia; 4Center for Health Technology Assessment, Universitas Padjadjaran, Bandung, Indonesia
Correspondence: Auliya A Suwantika
Department of Pharmacology and Clinical Pharmacy, Faculty of Pharmacy, Universitas Padjadjaran, Bandung, Indonesia
Email [email protected]
Background: In the area where there is a lack of medical experts, telemedicine gives a lot of benefits to deal with the distance and limited public infrastructure.
Objective: This study aimed to review the literature on the cost-effectiveness of telemedicine in Asian countries and possibly to provide recommendations on implementing telemedicine in this region.
Methods: Articles were independently screened in two selected databases (PubMed and EBSCO). The framework of patient, intervention, comparison, and outcome (PICO) was applied by considering Asian population, the intervention of telemedicine, current situation (without telemedicine) as the comparator, and cost per QALY gained as the major outcome.
Results: A total of 870 articles were identified from two databases: PubMed (n = 689 articles) and EBSCO (n = 181 articles). After removing 181 duplicates, 689 articles were screened by title and abstract, excluding 665 records. After the full-text screening on 24 articles, 8 articles were selected for further analysis. Various perspectives were applied in the included studies, such as societal, healthcare, and program perspectives. All studies applied different time horizons, such as 3-month, 25-year, 40-year, and lifetime. Among all included studies, several studies applied mathematical modeling.
Conclusion: The implementation of telemedicine in Asia can be a promising intervention since it can enhance the effectiveness of health services by saving time and travel costs. It also can reduce the overall costs of treatment, improve patients’ quality of life, and expand access to essential health services.
Keywords: cost per QALY gained, economic evaluation studies, cost utility analysis, cost-effective, cost saving
Introduction
Over the last decade, the use of telemedicine has improved patients’ health because both of patients and physicians are able to interact two ways and real-time via the internet.1 The main objective of telemedicine is to provide equal access of healthcare to the users. In the area where there is a lack of medical experts, telemedicine gives a lot of benefits to deal with the distance and limited public infrastructure. In particular, it is also beneficial for mitigating crises or emergencies, including for mitigating the pandemic of coronavirus disease 2019 (COVID-19). It can provide information about the treatment of COVID-19 that can be accessed quickly and easily, as reported in Singapore.2 In particular, its services have been rising in some countries in Asia, according to a previous study by Suzuki et al in 2016.3 Because of the internet penetration and the shortage of physicians, the use of telemedicine in Thailand and Indonesia has been increasing significantly.3
Despite the fact that telemedicine offers a lot of advantages, its services have not been fully integrated into the national healthcare systems.2 The progress of this integration was reported to be very slow, specifically in Asian countries.4 This situation might be caused by several complicated factors.5,6 A limited number of trainings for clinicians to implement telemedicine also contribute to the barriers that still exist in the national healthcare system.7 To deal with this situation, economic evaluations of telemedicine in Asia are required to be implemented.8 As a healthcare intervention, quality-adjusted life years (QALYs) can be measured as the final outcome of this intervention by taking this parameter and relevant costs into account in the studies.9 This study aimed to review the literature on the cost-effectiveness of telemedicine in Asian countries and possibly to provide recommendations on implementing telemedicine in this region.
Methods
Articles were independently screened by three investigators (AS, ABA and RIPS) in a period of June–July 2021 in two selected databases (PubMed and EBSCO) by using following keywords: a combination of economic evaluation terms (“cost benefit analysis”, “cost-effectiveness analysis”, “cost utility analysis”, “cost minimization analysis”, “quality of life”, “quality-adjusted life year”), and telemedicine terms (“video”, “mobile”, “mobile health”, “telemedicine”, “telemonitoring”, “internet”, “information technology”). The framework of patient, intervention, comparison, and outcome (PICO) was applied by considering Asian population, the intervention of telemedicine, current situation (without telemedicine) as the comparator, and cost per QALY gained as the major outcome.10 Discrepancies were dealt with by consensus or by discussions with other investigators (WS and AAS).
A scoping search was conducted by applying PRISMA flow diagram to identify telemedicine interventions in the disease management. In this study, we applied several inclusion and exclusion criteria. We included studies reported complete economic evaluations, such as cost-effectiveness analyses (CEA), cost-utility analyses (CUA), cost-minimization analyses (CMA), and cost–benefit analyses (CBA) by making comparison between telemedicine as the new intervention and without telemedicine as the current intervention. Furthermore, we included complete economic studies that were focused in Asian countries and published in the last ten years (2011–2021). We specifically excluded studies that were not published in English, not conducted in Asian countries, classified as non-original research articles (eg, systematic reviews, reviews, and meta-analysis), and only available in abstracts and conference proceedings.
To analyze the quality of reporting from each included study, we extracted data by using a predetermined standardized data extraction form, which was approved by all authors and amended as required. We extracted data regarding general study characteristics (eg, author, year of publication, setting and location, study objective, type of study, data collection and analytical method), and other specific methodological characteristics (eg, study perspective, comparison, time horizon, discount rate, choice of model, and parameters in the sensitivity analysis). If a study did not specify the year of currency and cost, we assumed it was the same as the publication year.
Result
Literature Search
A total of 870 articles were identified from two databases: PubMed (n = 689 articles) and EBSCO (n = 181 articles). After removing 181 duplicates, 689 articles were screened by title and abstract, excluding 665 records. After the full-text screening on 24 articles, 8 articles were selected for further analysis. More detailed information about PRISMA flow diagram of the study selection can be seen in Figure 1.
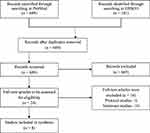 |
Figure 1 A flow diagram of study selection. Notes: From Annals of Internal Medicine, Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. 2018;169(7):467-473, Copyright© [2018] American College of Physicians. All Rights Reserved. Adapted with permission of American College of Physicians, Inc.29 |
General Characteristics
We derived eight selected studies from five different countries, such as India (n = 3), China (n = 1), Singapore (n = 2), Japan (n = 1), and Thailand (n = 1).11–18 All selected studies compared the intervention of telemedicine with regular interventions that have generally been used in healthcare facilities. Information about the general characteristics of the included studies can be seen in Table 1.
 |
Table 1 General Characteristics of Included Studies |
From three studies that were conducted in India, a study by Rachapelle et al highlighted the cost utility of telemedicine to screen for diabetic retinopathy in Rural Tamil Nadu, Southern India.11 Other studies focused on mobile health and telephone-based interventions. A cluster randomized controlled trial study by Modi et al investigated the cost-effectiveness of a mobile health intervention in improving infant mortality to be implemented in Tribal Areas of Gujarat, India.14 Another study by Arora et al explored the cost-effectiveness of telephone-based intervention to support the management of pressure ulcers in people with spinal cord injury in India and Bangladesh.18
From two studies that were conducted in Singapore, a study by Kaur et al in 2020 estimated the cost-effectiveness of using hearing aid (HA) plus aural rehabilitation versus delayed hearing aid in adults with hearing impairment.15 Applying the urban setting in Singapore, Nguyen et al determined the incremental cost-effectiveness of a new telemedicine technician-based evaluation relative to a regular family physician (FP)-based evaluation of diabetic retinopathy (DR) from the perspectives of healthcare and societal.17
A study by Song and Kanaoka in Japan specifically investigated the effectiveness of mobile application for menstrual management ini Japanese working women through a randomized controlled trial that was coupled with a medical economic evaluation.12 An economic evaluation study to evaluate the differential benefits of home visits with telephone calls and telephone calls only in Hong Kong, China was conducted by Wong et al in 2015.13 Additionally, a study by Kitwitee et al in Thailand applied cost-utility analysis to evaluate the implementation of video-electroencephalography (VEEG) monitoring followed by surgery in adults with drug-resistant focal epilepsy.16
Methodological Characteristics
In economic evaluation studies, the choice of perspective is crucial since it affects the cost component to be considered in the study.19 Various perspectives were applied in the included studies, such as societal (n = 4), societal and healthcare (n = 3), and program perspective (n = 1). Furthermore, the results of economic evaluation studies are related to the application of time horizon. All studies applied different time horizons. We found two studies applied a 25-year time horizon,11,12 and three other studies applied different time horizon, such as 3-month,18 40-year,16 and lifetime.17 The rest of the studies (n = 3) did not confirm a time horizon. If studies applied the time horizon more than a year, then the health effect should be modified with a discount rate. We found that four studies applied a discount rate at 3%,11,14,16,17 and one study applied a discount rate at 2%.12
Among all included studies, six studies applied mathematical modeling.11,14–18 Rachapelle et al used a Markov model to measure the cost-utility by comparing 6 different screening intervals on 1000 rural diabetic patients, who were 40 years of age and had not previously been screened for DR.11 A study by Kitwitee et al also used a Markov model to measure total cost and effectiveness.16 In addition, a study by Kaur et al used Markov model to assess cost effectiveness in using HA, compared with non-HA group.15 Modi et al considered relevant cost and effectiveness parameters in the implementation of mobile health intervention within a decision tree model.14 Wong et al applied a randomized control trial to explore readmission outcome by comparing home visit plus phone calls with phone calls only for patients discharged from medical unit due to chronic illness.13
Furthermore, Arora et al used a Markov model to calculate the incremental cost-effectiveness ratio (ICER) in a comparison between telemedicine-based DR screening and FP-based DR screening over a lifetime.18 A Markov model was also applied by Nguyen et al to estimate the cost-effectiveness of telemedicine by considering two major factors: (i) if telemedicine was less cost and higher utility, compared with regular model, telemedicine would be cost-saving; and (ii) if telemedicine was more expensive and higher utility, compared with regular model, ICER will be the difference in total costs divided by the difference in total QALYs gained.17
Additionally, sensitivity analysis is necessary to be included in economic evaluation studies to assess the impact of uncertain parameters in the ICER. From all retrieved studies, only two studies did not apply sensitivity analysis.13,16 Other studies (n = 6) applied sensitivity analysis by considering various parameters, such as prevalence of the disease, intervention cost (eg, direct medical, direct non-medical, indirect, and other relevant costs), utility, disease degree, and other outcomes. More detailed information about the methodological characteristics of the included studies can be seen in Table 2.
 |
Table 2 Methodological Characteristics of Included Studies |
Discussion
In this study, we reviewed eight articles that focused on investigating the cost-effectiveness of telemedicine in Asia.11–18 Two studies by Arora et al and Wong et al specifically investigated the cost-effectiveness of mobile phone intervention in India and Bangladesh; and Hong Kong, respectively. Comparing telephone-based support with usual care in management of pressure ulcers in 120 people with spinal cord injury in India and Bangladesh, a study by Arora et al concluded the probability of the intervention to be cost-effective would be 41%.18 In the context of reducing the hospital readmissions, a study by Wong et al confirmed that the intervention of home visit and calls was more effective than calls only.13 In particular, two other studies focused on the cost-effectiveness of mobile health application. Focusing on the use of m-Health program for maternal, neonatal, and child healthcare management in Gujarat, India, a study by Modi et al concluded that the intervention was cost-effective and recommended to be implemented in a wider range of population in India.14 Comparing the use of mobile application versus not using mobile application in female workers for menstrual management in Japan, a study by Song and Kanaoka highlighted the intervention group resulted QALYs and costs at 0.07 higher and $1170 lower than the control group, respectively.12
Considering the implementation of FP and Singapore Integrated Diabetic Retinopathy Program (SiDRP), a study by Nguyen et al concluded SiDRP as the new intervention showed better cost-effectiveness value than FP in the context of DR screening program.17 Another similar study by Rachapelle et al in 2018 also highlighted that teleophthalmology screening program was considered to be more cost-effective than no DR screening in rural Tamil Nadu, Southern India.11 In the context of video monitoring, a study by Kitwitee et al in Thailand confirmed the probability of VEEG to be cost-effective was 84% by applying a cost-effective threshold at THB 160,000 per QALY gain.16 Taking the use of HA as a telemedicine, a study by Kaur et al confirmed that HA as a telemedicine could be cost-effective in a person with hearing-impairment after a short period of using the device and long-term cost-effectiveness of HA would depend on the duration of use of intervention.15 More detailed information about the primary results of all included studies can be seen in Table 3.
 |
Table 3 Primary Results |
All of these included studies have proven that the use of telemedicine was more cost-effective than the traditional programs by increasing therapeutic effects and providing improvement in the efficiency of health services.20 It can be highlighted that telemedicine is a promising approach to increase life expectancy and to reduce infant mortality.14,16 It can also increase the effectiveness of treatment.18 In addition, the potential of telemedicine to be a cost-saving intervention has been confirmed by the evidence in a study by Nguyen et al,17 which strengthened the results of a previous study by Ji et al in terms of telemedicine can save patients’ time and travel costs.21
In the context of Sustainable Development Goals (SDGs), the United Nations has committed the SDGs to be achieved by 2030 with the 3rd SDG is to ensure healthy living and promote well-being for all people at all ages.22 It can be highlighted that all human beings have the same rights to access good health service that will support sustainable development and socioeconomic improvements. As an alternative choice, telemedicine can be used for people with limited access to direct health services. In low-income countries, it can be an alternative for patients who cannot afford good healthcare services that are not covered by the social insurance. For health crisis mitigation, the use of telemedicine can also be optimized because of its cost-effectiveness.1
In Asia, telemedicine has become popular and has been used to expand more access to essential health services, specifically for rural communities who have barriers to getting accessible healthcare facilities because they are concentrated in urban areas. Other problems that patients from rural areas may face are poor infrastructures and complicated geographic locations. In this case, telemedicine has the ability to deliver healthcare services, provide better information, decrease discrepancies in the healthcare, and improve healthcare outcomes.23,24 In particular, telemedicine can assist the healthcare system to be more patient-centered.25 Because of the increasing number of smartphones’ users, the extensive use of internet, and the application of electronic medical records, the possibility of telemedicine to be included in the healthcare system is getting higher.26 Nevertheless, the illiteracy of technology and the unaffordability of supporting devices remain the biggest challenges in the implementation of telemedicine in low-income countries.27,28
To our knowledge, this study is the first scoping review study that focused on the economic evaluations of telemedicine in Asia. Despite the fact that this study has a major novelty, it also has several limitations. First, we were unable to conduct a meta-analysis due to heterogeneity of the included studies. Nevertheless, we have provided a narrative review by outlining the current evidence on this topic and highlighting gap that remains unexplored for future studies. Secondly, we found the risk of publication bias since we only focused on peer-reviewed published studies to ensure comparable study quality. Nevertheless, this study provides an overview about the potential cost-effectiveness of telemedicine in health services to improve patients’ quality of life as the final outcome. Hopefully, this study can assist the stakeholders in making decisions regarding the implementation of telemedicine in Asia.
Conclusions
The results suggest that the implementation of telemedicine in Asia can be a promising intervention since it can enhance the effectiveness of health services by saving time and travel costs. It also can reduce the overall costs of treatment, improve patients’ quality of life and expand access to essential health services.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kichloo A, Albosta M, Dettloff K, et al. Telemedicine, the current COVID-19 pandemic and the future: a narrative review and perspectives moving forward in the USA. Fam Med Com Health. 2020;8(3):e000530. doi:10.1136/fmch-2020-000530
2. Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020;26(5):309–313. doi:10.1177/1357633X20916567
3. Suzuki T, Hotta J, Kuwabara T, et al. Possibility of introducing telemedicine services in Asian and African countries. Health Policy Technol. 2020;9(1):13–22. doi:10.1016/j.hlpt.2020.01.006
4. Peddle K. Telehealth in context: socio-technical barriers to Telehealth use in Labrador, Canada. Comput Supported Coop Work. 2007;16(6):595–614. doi:10.1007/s10606-006-9030-3
5. Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform. 2010;79(11):736–771. doi:10.1016/j.ijmedinf.2010.08.006
6. Green T, Hartley N, Gillespie N. Service provider’s experiences of service separation: the case of telehealth. J Serv Res. 2016;19(4):477–494. doi:10.1177/1094670516666674
7. Edirippulige S, Brooks P, Carati C, et al. It’s important, but not important enough: eHealth as a curriculum priority in medical education in Australia. J Telemed Telecare. 2018;24(10):697–702. doi:10.1177/1357633X18793282
8. Bhaskar S, Bradley S, Chattu VK, et al. Telemedicine as the new outpatient clinic gone digital: position paper from the pandemic health system REsilience PROGRAM (REPROGRAM) international consortium (Part 2). Front Public Health. 2020;8:410. doi:10.3389/fpubh.2020.00410
9. Bergmo TS. Using QALYs in telehealth evaluations: a systematic review of methodology and transparency. BMC Health Serv Res. 2014;14(1):332. doi:10.1186/1472-6963-14-332
10. Eriksen MB, Frandsen TF. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: a systematic review. jmla. 2018;106:4. doi:10.5195/JMLA.2018.345
11. Rachapelle S, Legood R, Alavi Y, et al. The cost–utility of telemedicine to screen for diabetic retinopathy in India. Ophthalmology. 2013;120(3):566–573. doi:10.1016/j.ophtha.2012.09.002
12. Song M, Kanaoka H. Effectiveness of mobile application for menstrual management of working women in Japan: randomized controlled trial and medical economic evaluation. J Med Econ. 2018;21(11):1131–1138. doi:10.1080/13696998.2018.1515082
13. Wong FKY, So C, Chau J, Law AKP, Tam SKF, McGhee S. Economic evaluation of the differential benefits of home visits with telephone calls and telephone calls only in transitional discharge support. Age Ageing. 2015;44(1):143–147. doi:10.1093/ageing/afu166
14. Modi D, Saha S, Vaghela P, et al. Costing and cost-effectiveness of a mobile health intervention (ImTeCHO) in improving infant mortality in tribal areas of Gujarat, India: cluster randomized controlled trial. JMIR Mhealth Uhealth. 2020;8(10):e17066. doi:10.2196/17066
15. Kaur P, Chong SL, Kannapiran P, et al. Cost-utility analysis of hearing aid device for older adults in the community: a delayed start study. BMC Health Serv Res. 2020;20(1):1112. doi:10.1186/s12913-020-05977-x
16. Kitwitee P, Unnwongse K, Srikijvilaikul T, Yadee T, Limwattananon C. Cost-utility of video-electroencephalography monitoring followed by surgery in adults with drug-resistant focal epilepsy in Thailand. World Neurosurg. 2017;98(750–760.e3):750–760.e3. doi:10.1016/j.wneu.2016.11.041
17. Nguyen HV, Tan GSW, Tapp RJ, et al. Cost-effectiveness of a national telemedicine diabetic retinopathy screening program in Singapore. Ophthalmology. 2016;123(12):2571–2580. doi:10.1016/j.ophtha.2016.08.021
18. Arora M, Harvey LA, Glinsky JV, et al. Cost-effectiveness analysis of telephone-based support for the management of pressure ulcers in people with spinal cord injury in India and Bangladesh. Spinal Cord. 2017;55(12):1071–1078. doi:10.1038/sc.2017.87
19. Indonesian Ministry of Health. Guidelines for the Implementation of Pharmacoeconomics Studies. Directorate General of Pharmaceutical and Medical Devices Development; 2013.
20. Jennett PA, Affleck Hall L, Hailey D, et al. The socio-economic impact of telehealth: a systematic review. J Telemed Telecare. 2003;9(6):311–320. doi:10.1258/135763303771005207
21. Ji X, Wang Y, Ma Y, et al. Improvement of disease management and cost effectiveness in Chinese patients with Ankylosing Spondylitis using a smart-phone management system: a prospective cohort study. Biomed Res Int. 2019;2019:1–11. doi:10.1155/2019/2171475
22. Nunes AR, Lee K, O’Riordan T. The importance of an integrating framework for achieving the sustainable development goals: the example of health and well-being. BMJ Glob Health. 2016;1(3):e000068. doi:10.1136/bmjgh-2016-000068
23. Delaigue S, Bonnardot L, Steichen O, et al. Seven years of telemedicine in Médecins Sans Frontières demonstrate that offering direct specialist expertise in the frontline brings clinical and educational value. J Glob Health. 2018;8(2):020414. doi:10.7189/jogh.08.020414
24. Jha AK, Sawka E, Tiwari B, et al. Telemedicine and community health projects in Asia. Dermatol Clin. 2021;39(1):23–32. doi:10.1016/j.det.2020.08.003
25. Boxer RJ. Advantages and utilization of telemedicine. mHealth. 2019;5:12. doi:10.21037/mhealth.2019.04.02
26. Chellaiyan V, Nirupama A, Taneja N. Telemedicine in India: where do we stand? J Family Med Prim Care. 2019;8(6):1872. doi:10.4103/jfmpc.jfmpc_264_19
27. Eze ND, Mateus C, Cravo Oliveira Hashiguchi T. Telemedicine in the OECD: an umbrella review of clinical and cost-effectiveness, patient experience and implementation. PLoS One. 2020;15(8):e0237585. doi:10.1371/journal.pone.0237585
28. Bonnardot L, Wootton E, Liu J, et al. User feedback on the MSF tele-expertise service after a 4-year pilot trial – a comprehensive analysis. Front Public Health. 2015;3. doi:10.3389/fpubh.2015.00257
29. Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–473. doi:10.7326/M18-0850
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
