Back to Journals » ClinicoEconomics and Outcomes Research » Volume 8
Cost-effectiveness of dipeptidyl peptidase-4 inhibitor monotherapy in elderly type 2 diabetes patients in Thailand
Authors Permsuwan U , Dilokthornsakul P , Saokaew S , Thavorn K, Chaiyakunapruk N
Received 25 May 2016
Accepted for publication 22 July 2016
Published 21 September 2016 Volume 2016:8 Pages 521—529
DOI https://doi.org/10.2147/CEOR.S113559
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Giorgio Colombo
Unchalee Permsuwan,1 Piyameth Dilokthornsakul,2 Surasak Saokaew,2–4 Kednapa Thavorn,5–7 Nathorn Chaiyakunapruk2,4,8,9
1Faculty of Pharmacy Chiang Mai University, Chiang Mai, 2Center of Pharmaceutical Outcomes Research, Faculty of Pharmaceutical Sciences, Naresuan University, Phitsanulok, 3Center of Health Outcomes Research and Therapeutic Safety, School of Pharmaceutical Sciences, University of Phayao, Phayao, Thailand; 4School of Pharmacy, Monash University Malaysia, Sunway, Malaysia; 5Ottawa Hospital Research Institute, The Ottawa Hospital, 6School of Epidemiology, Public Health and Preventive Medicine, Faculty of Medicine, University of Ottawa, Ottawa, 7Institute for Clinical and Evaluative Sciences, Toronto, ON, Canada; 8School of Population Health, The University of Queensland, Brisbane, QLD, Australia; 9School of Pharmacy, University of Wisconsin–Madison, Madison, WI, USA
Background: The management of type 2 diabetes mellitus (T2DM) in elderly population poses many challenges. Dipeptidyl peptidase-4 (DPP-4) inhibitors show particular promise due to excellent tolerability profiles, low risk of hypoglycemia, and little effect on body weight. This study evaluated, from the health care system’s perspective, the long-term cost-effectiveness of DPP-4 inhibitor monotherapy vs metformin and sulfonylurea (SFU) monotherapy in Thai elderly T2DM patients.
Methods: The clinical efficacy was estimated from a systematic review and meta-analysis. Baseline cohort characteristics and cost parameters were obtained from published studies and hospital databases in Thailand. A validated IMS CORE Diabetes Model version 8.5 was used to project clinical and economic outcomes over a lifetime horizon using a 3% annual discount rate. Costs were expressed in 2014 Thai Baht (THB) (US dollar value). Incremental cost-effectiveness ratios were calculated. Base-case assumptions were assessed through several sensitivity analyses.
Results: For treating elderly T2DM patients, DPP-4 inhibitors were more expensive and less effective, ie, a dominated strategy, than the metformin monotherapy. Compared with SFU, treatment with DPP-4 inhibitors gained 0.031 more quality-adjusted life years (QALYs) at a total cost incurred over THB113,701 or US$3,449.67, resulting in an incremental cost-effectiveness ratio of THB3.63 million or US$110,133.50 per QALY. At the acceptable Thai ceiling threshold of THB160,000/QALY (US$4,854.37/QALY), DPP-4 inhibitors were not a cost-effective treatment.
Conclusion: DPP-4 inhibitor monotherapy is not a cost-effective treatment for elderly T2DM patients compared with metformin monotherapy and SFU monotherapy, given current resource constraints in Thailand.
Keywords: cost-effectiveness analysis, DPP-4 inhibitor, elderly, type 2 diabetes, Thailand
Introduction
Type 2 diabetes mellitus (T2DM) is a common chronic health condition in the elderly. The number of elderly T2DM patients has been growing worldwide, especially in upper-middle income countries such as Thailand. Based on the findings of the Fourth Thai National Health Examination Survey in 2009, diabetes was most prevalent in women, the elderly, and urban areas. The prevalence of impaired fasting glucose and undiagnosed diabetes increased with age, peaking at age ≥75 years and 55–64 years, respectively.1 Diabetes in the elderly is associated with a greater risk of T2DM-related micro- and macrovascular complications, cognitive disorders, physical disability, morbidity, and mortality;2–5 the selection of antidiabetic treatment for elderly T2DM patients poses many challenges for a number of reasons. First, elderly T2DM patients have a greater incidence of hypoglycemia6 which can precipitate serious events such as falls and accompanying fractures. The study by Zhao et al7 showed that hypoglycemia patients had higher rates of fall-related fractures than those without hypoglycemia, within 30 days and 1 year (0.64% vs 0.02% and 2.11% vs 0.50%, respectively). Second, elderly T2DM patients are more likely to have comorbidities with their diabetes, leading to the use of polypharmacy.4,8,9 Third, chronic kidney disease often occurs in elderly T2DM patients;10 the prevalence of chronic kidney disease among T2DM patients in Australia,11 India,12 Finland,13 Singapore,14 and the US15 ranged from 40% to 70%. With these associated challenges for elderly T2DM patients, finding effective and safe therapeutic agents is very crucial.
Dipeptidyl peptidase-4 (DPP-4) inhibitors show particular promise for treating elderly T2DM patients because they have excellent tolerability profiles, low risk of hypoglycemia, and little effect on body weight.4,16,17 Therefore, this study evaluated the cost-effectiveness of DPP-4 inhibitor monotherapy compared with sulfonylurea (SFU) monotherapy or metformin monotherapy for treating elderly T2DM patients in the Thai context.
Methods
Study design and cohort population
From a Thai health care system perspective, we conducted a cost-utility analysis and used a validated IMS CORE Diabetes Model (CDM), Version 8.5, to estimate long-term costs and outcomes associated with each treatment over a lifetime horizon. Details of this model are described elsewhere.18,19 A 3% discount rate per annum was applied to both costs and outcomes in line with the Thai Health Technology Assessment (HTA) guideline.20
The cohort population was Thai people with T2DM aged at least 65 years. Table 1 presents the baseline demographics, risk factors, and clinical complications of the cohort, which were obtained from published data and hospital databases in Thailand.21–28 The all-cause mortality rate was also adjusted with the age-specific mortality rate of Thai people.29 Utility values used in the CDM were based mostly on published studies conducted in other countries.30–34
  | Table 1 Baseline characteristics of the cohort population Abbreviations: BCRH, Buddhachinaraj Regional Hospital; SD, standard deviation; TDR, Thailand diabetes registry. |
This study was approved by the Buddhachinaraj Regional Hospital Ethics Committee on August 8, 2014. As the patient data is de-identified patient consent was not required.
Interventions in the study
Our study considered the following DPP-4 inhibitors: saxagliptin, sitagliptin, and vildagliptin. These medications were administered as a monotherapy and then compared with either metformin monotherapy or SFU monotherapy. We used metformin and SFU (glipizide) as comparators for several reasons. First, the Thai HTA guideline35 recommends current practice as a comparator. Metformin and SFU are considered as usual care for elderly T2DM patients in Thailand. Second, we convened a panel of stakeholders to discuss the scope and appropriate comparators of the study, including endocrinologists, and policy makers, and then followed the consensus of the meeting. This study used the normal daily dose of each treatment option: saxagliptin (5 mg), sitagliptin (100 mg), vildagliptin (100 mg), glipizide (10 mg), and metformin (2,000 mg).
Costs
Only the direct medical costs, such as cost of intervention, concurrent medications, diabetic screening, management, and treatment complications, were included in the cost-effectiveness analysis. Cost data were derived from the published literature and retrospective hospital database analyses (Table 2).36–41 All costs were inflated using Thailand’s consumer price index42 and presented in the year 2014 THB value. Costs were converted to US$ at a rate of THB32.96 per US$ as of December 30, 2014.43
The cost of DPP-4 inhibitors was proposed to the subcommittee for the development of the National List of Essential Medicine by the pharmaceutical companies. Total cost per year of saxagliptin, sitagliptin, and vildagliptin was THB13,492 (US$409.34), THB16,570 (US$502.73), and THB15,900 (US$482.40), respectively. Glipizide and metformin have several generic products in Thailand. We used a median of the median prices of those generic products44 as recommended by the Thai HTA guideline.45 The annual total costs of metformin and SFU were THB496 (US$15.05) and THB149 (US$4.52), respectively.
Treatment efficacy and adverse events
Due to limited evidence of treatment efficacy in Thailand, we performed a systematic review and meta-analysis to estimate the pooled efficacy of DPP-4 inhibitor monotherapy compared to SFU monotherapy and metformin monotherapy in elderly T2DM patients. The MEDLINE, EMBASE, and Clinicaltrial.gov databases were systematically searched from their inception to August 2014. We found only one study46 that indicated noninferiority of alogliptin compared to glipizide in HbA1c reduction (the weighted mean difference -0.09; 95% CI, -∞ to 0.06), substantially lower risk of hypoglycemia (risk ratio [RR] 0.21; 95% CI, 0.11–0.41), lower risk of severe hypoglycemia (RR 0.23; 95% CI, 0.03–1.99), and no weight gain with DPP-4 inhibitor monotherapy compared to glipizide monotherapy in elderly T2DM patients (Table 3).
  | Table 3 Efficacy and adverse effects of DPP-4 inhibitors, metformin, and SFU Notes: aHbA1c reduction from baseline of DPP-4 inhibitors =–0.92 (–1.20+0.28). Upper 95% CI =–1.03 (–1.2+0.17) and lower 95% CI =–0.8 (–1.2+0.4). bEstimate the efficacy of metformin from the pooled analysis of seven studies40,44–49 included in the meta-analysis by Wu et al.51 cHbA1c reduction from baseline of SFU =–0.83 (–0.92+0.09). Upper 95% CI assumed to be =0 (–0.92+∞), lower 95% CI =–0.98 (–0.92-0.06). dRisk of severe hypoglycemia of DPP-4 inhibitors =0.55% (2.44%×0.225). eRisk of severe hypoglycemia of DPP-4 inhibitors was assumed to be equal to that of metformin. fRisk of symptomatic hypoglycemia of DPP-4 inhibitors =4.14% (19.36%×0.214), gRisk of symptomatic hypoglycemia of metformin =9.41% (4.14%/0.44). hEstimate risk ratio of severe hypoglycemia from the pooled analysis of two studies52,55 included in the meta-analysis by Wu et al.51 Abbreviations: BCRH, Buddhachinaraj Regional Hospital; DPP-4, dipeptidyl peptidase-4; SFU, sulfonylurea. |
Three studies5,47,48 compared metformin with DPP-4 inhibitor monotherapy and concluded that DPP-4 inhibitor was an effective and well-tolerated treatment option for elderly T2DM patients. In addition, reduction in HbA1c after treatment with DPP-4 inhibitors in elderly T2DM patients was not significantly different from those in younger patients.49 Therefore, we decided to systematically search a meta-analysis study that compared DPP-4 inhibitor monotherapy with metformin monotherapy in T2DM patients, and found two eligible studies.50,51 Both were high quality studies (with scores of at least 9 of 11) based on the Assessment of Multiple Systematic Reviews, We decided to use Wu et al’s51 meta-analysis as it was the most up-to-date. The efficacy of HbA1c reduction from the baseline of metformin monotherapy was estimated from the pooled analysis of seven studies48,52–57 included in the meta-analysis of Wu et al.51 Of those studies,48,52–57 severe hypoglycemia was presented in two studies,52,55 for which the RR was estimated. The calculation details are shown in Table 3.
Sensitivity analyses
To determine the robustness of the findings, we undertook a probabilistic sensitivity analysis and presented the relationship between the probability of favoring DPP-4 inhibitors and the value of the willingness to pay for an additional unit of quality-adjusted life year (QALY) as a cost-effectiveness acceptability curve. The current acceptable Thai ceiling threshold of THB160,000/QALY (US$4,854.37/QALY) was recommended by the subcommittee for the development of the universal health coverage benefit package and service delivery in Thailand.58 A series of one-way sensitivity analyses were also performed to determine the effect of HbA1c change, risk of hypoglycemia, drug cost, and discount rate. The results were displayed as a Tornado diagram.
Results
Base-case analysis
In the base-case scenario, all three DPP-4 inhibitors incurred higher costs and yielded fewer QALYs (5.965 QALYs vs 5.986 QALYs). In other words, all DPP-4 inhibitors were dominated, making metformin monotherapy a cost-saving treatment in elderly T2DM patients in Thai context (Table 4).
All three DPP-4 inhibitors were more effective (equal 0.031 higher QALYs) but more costly than SFU. Saxagliptin yielded the lowest incremental cost per QALY, followed by vildagliptin and sitagliptin (THB3,632,604/QALY or US$110,212.50/QALY, THB4,335,273/QALY or US$131,531.34/QALY, and THB4,530,556/QALY or US$137,456.19/QALY, respectively). With the current Thai threshold of THB160,000/QALY (US$4,854.37/QALY), DPP-4 inhibitors were not cost-effective compared to SFU for treating elderly T2DM patients in the Thai context (Table 4).
Sensitivity analyses
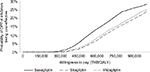
As vildagliptin and sitagliptin were dominated by saxagliptin, the results of one-way sensitivity analysis, therefore, were displayed on saxagliptin compared to SFU. The change in HbA1c from the baseline of DPP-4 inhibitors, discount rate, risk of severe hypoglycemia, and cost of saxagliptin had some effect on the incremental cost-effectiveness ratio (ICER) (Figure 1). The greater the effect of DPP-4 inhibitors on the reduction of HbA1c from baseline, the lower ICER (Figure 1). Based on the cost-effectiveness acceptability curve (Figure 2), all DPP-4 inhibitors were not a cost-effective treatment compared to SFU at the ceiling threshold of 160,000 THB/QALY. Compared to metformin, the probability of DPP-4 inhibitors being cost-effective was even smaller than being compared to SFU.
Discussion
Elderly patients with diabetes have an increased risk of T2DM-related morbidity and mortality. The treatment goal for elderly T2DM patients is to optimize glycemic control while minimizing the risk of drug-associated adverse events. Thus, this study was conducted to generate economic evidence of DPP-4 inhibitors for T2DM treatment in response to a request by the subcommittee for the development of the National List of Essential Medicine in 2014. The findings of the study were submitted and presented to the subcommittee in 2015 to justify policy decision in terms of the value for money. This cost-effectiveness study followed the Thai national HTA guideline.59 Our findings indicated that DPP-4 inhibitor monotherapy was not a cost-effective treatment for elderly T2DM patients in Thailand compared to either SFU monotherapy or metformin monotherapy. Efficacy in HbA1c reduction, risk of severe hypoglycemia, and cost of DPP-4 inhibitors play an important role in the findings of the study.
We are not aware of other studies evaluating the cost-effectiveness of DPP-4 inhibitor monotherapy in elderly T2DM patients. Geng et al60 conducted a systematic review of cost-effectiveness of DPP-4 inhibitors for treating T2DM; the eleven included studies assessed DPP-4 inhibitors as an add-on therapy. Of those, seven studies compared DPP-4 inhibitors and metformin with SFU and metformin. Six studies concluded that DPP-4 inhibitors were cost-effective compared to SFU for treating T2DM patients for whom metformin monotherapy failed to achieve glycemic control.
Our study was strengthened by incorporating input parameters, such as costs, baseline cohort characteristics, and adverse events, from data sources that were reliable and relevant to the Thai context. Similarly, it is important to point out some potential limitations of our study. First, based on our systematic review, we found only one study46 that evaluated the efficacy and safety of a DPP-4 inhibitor monotherapy compared to SFU monotherapy in elderly T2DM patients. This study indicated noninferiority in HbA1c reduction but a lower risk of hypoglycemia and no weight gain with the DPP-4 inhibitor monotherapy compared to SFU monotherapy. Only three studies5,47,48 compared DPP-4 inhibitor monotherapy with metformin monotherapy in elderly T2DM patients. However, HbA1c reduction after treatment with DPP-4 inhibitors was not significantly different in elderly T2DM patients vs younger T2DM patients.49 We addressed this limitation by the pooled analysis of seven studies48,52–57 included in the meta-analysis study by Wu et al51 that compared metformin monotherapy with DPP-4 inhibitor monotherapy in T2DM patients. Second, we tried our best to use resource utilization and cost data from Thailand. Some cost data were not available, such as the cost of an infected ulcer; we assumed them equal to zero. We reanalyzed our base-case analysis, assuming the cost of an infected ulcer similar to an uninfected ulcer. The results showed a slightly lower ICER from THB3,632,604/QALY (US$110,212.50/QALY) to THB3,630,697/QALY (US$110,154.64/QALY) comparing saxagliptin to SFU. Metformin monotherapy was still a dominant treatment compared to DPP-4 inhibitor monotherapy, when assuming equal cost of an infected and uninfected ulcer. The availability of local evidence is another limitation. Even though costs, baseline cohort characteristics, and adverse events were obtained from published studies or hospital databases in Thailand, this study relies on utility values and transition probabilities within the CDM from studies conducted in other countries. Given these limitations, the confirmation of this study’s findings may be premature. However, the findings indicate that treating elderly T2DM patients using DPP-4 inhibitor monotherapy in a Thai context may not be cost-effective.
Conclusion
For treating elderly T2DM patients in Thailand, DPP-4 inhibitor monotherapy is not a cost-effective treatment compared to metformin monotherapy. In addition, DPP-4 inhibitor monotherapy is not a cost-effective treatment compared to SFU monotherapy at the current Thai threshold of THB160,000/QALY. The high acquisition cost of DPP-4 inhibitors is one of the key factors in the findings of this study.
Acknowledgments
The authors would like to acknowledge the National Drug Selection Working Group in Endocrinology for their valuable advice and comments. In addition, the IMS Team provided training and support for the CDM. This study was supported by grants from the Subcommittees of the National List of Essential Medicine, Thailand.
Disclosure
The authors report no conflicts of interest in this work.
References
Aekplakorn W, Chariyalertsak S, Kessomboon S, et al. Prevalence and management of diabetes and metabolic risk factors in Thai adults. Diabetes Care. 2011;34:1980–1985. | ||
Wan EY, Fong DY, Fung CS, Lam CL. Incidence and predictors for cardiovascular disease in Chinese patients with type 2 diabetes mellitus – a population-based retrospective cohort study. J Diabetes Complications. 2015;30(3):444–450. | ||
Moran C, Beare R, Phan TG, et al; Alzheimer’s Disease Neuroimaging Initiative (ADNI). Type 2 diabetes mellitus and biomarkers of neurodegeneration. Neurology. 2015;85(13):1123–1130. | ||
Du YF, Ou HY, Beverly EA, Chiu CJ. Achieving glycemic control in elderly patients with type 2 diabetes: a critical comparison of current options. Clin Interv Aging. 2014;9:1963–1980. | ||
Schweizer A, Dejager S, Foley JE, Shao Q, Kothny W. Clinical experience with vildagliptin in the management of type 2 diabetes in a patient population ≥75 years: a pooled analysis from a database of clinical trials. Diabetes Obes Metab. 2011;13(1):55–64. | ||
Rosenstock J. Management of type 2 diabetes in the elderly. Special considerations. Drugs Aging. 2001;18:31–44. | ||
Zhao Y, Kachroo S, Kawabata H, et al. Association between hypoglycemia and fall-related fractures and health care utilization in older veterans with type 2 diabetes. Endocr Pract. 2016;22(2):196–204. | ||
Chow JY, Nie JX, Tracy CS, Wang L, Upshur RE. Comorbidity in very old adults with type 2 diabetes mellitus. J Am Geriatr Soc. 2013;61(6):1028–1029. | ||
Alonso-Moran E, Orueta JF, Esteban JI, et al. Multimorbidity in people with type 2 diabetes in the Basque Country (Spain): prevalence, comorbidity clusters and comparison with other chronic patients. Eur J Intern Med. 2015;26(3):197–202. | ||
Thomas MC, Cooper ME, Zimmet P. Changing epideiology of type 2 diabetes mellitus and associated chronic kidney disease. Nat Rev Nephrol. 2016;12(2):73–81. | ||
Thomas MC, Weekes AJ, Broadley OJ, Cooper ME, Mathew TH. The burden of chronic kidney disease in Australian patients with type 2 diabetes (the NEFRON study). Med J Aust. 2006;185(3):140–144. | ||
Prasannakumar M, Rajput R, Seshadri K, et al. An observational, cross-sectional study to assess the prevalence of chronic kidney disease in type 2 diabetes patients in India (START -India). Indian J Endocrinol Metab. 2015;19(4):520–523. | ||
Metsarinne K, Broijersen A, Kantola I, et al; STages of NEphropathy inType 2 Diabetes Study Investigators. High prevalence of chronic kidney disease in Finnish patients with type 2 diabetes treated in primary care. Prim Care Diabetes. 2015;9(1):31–38. | ||
Low SK, Sum CF, Yeoh LY, et al. Prevalence of chronic kidney disease in adults with type 2 diabetes mellitus. Ann Acad Med Singapore. 2015;44(5):164–171. | ||
Bailey RA, Wang Y, Zhu V, Rupnow MF. Chronic kidney disease in US adults with type 2 diabetes: an updated national estimate of prevalence based on kidney disease: improving global outcomes (KDIGO) staging. BMC Res Notes. 2014;7:415. | ||
Moghissi E. Management of type 2 diabetes mellitus in older patients: current and emerging treatment options. Diabetes Ther. 2013;4(2):239–256. | ||
Scheen AJ. A review of gliptins in 2011. Expert Opin Pharmacother. 2012;13:81–99. | ||
Palmer AJ, Roze S, Valentine WJ, et al. The CORE diabetes model: projecting long-term clinical outcomes, costs and cost-effectiveness of interventions in diabetes mellitus (type 1 and 2) to support clinical and reimbursement decision-making. Curr Med Res Opin. 2004;20(suppl 1):S5–S26. | ||
Palmer AJ, Roze S, Valentine WJ, et al. Validation of the CORE diabetes model against epidemiological and clinical studies. Curr Med Res Opin. 2004;20(suppl 1):S27–S40. | ||
Permsuwan U, Guntawongwan K, Buddhawongsa P. Handling time in economic evaluation studies. J Med Assoc Thai. 2014;97(suppl 5):S50–S58. | ||
Ngarmukos C, Bunnag P, Kosachunhanun N, et al. Thailand diabetes registry project: prevalence, characteristics and treatment of patients with diabetic nephropathy. J Med Assoc Thai. 2006;89(suppl 1):S37–S42. | ||
Trongsakul S. The prevalence of undiagnosed cognitive impairment and prevalence of undiagnosed depressive mood in over 60’s with type 2 diabetes in a Thai community: a cross-sectional study [dissertation]. Norwich: Faculty of Medicine and Health Sciences, University of East Anglia; 2013. | ||
Porapakkham Y, Plattara-Archachai J. Elderly health problems 2004. J Health Syst Res. 2007;1(2):98–115. | ||
Thamarangsi T. The Situation of Alcohol Beaverage Consumption and Impact in Thailand 2013. Center for Alcohol Studies, International Health Policy Program, Ministry of Public Health; 2013. | ||
Thaneerat T, Tangwongchai S. Prevalence of depression, hemoglobin A1c level, and associated factors in outpatients with type 2 diabetes. Asian Biomed (Res Rev News). 2009;3:383–390. | ||
The Endocrine Society of Thailand. Diabetes Registry Project 2003. Health Systems Research Institute; 2004. | ||
Nitiyanant W, Chetthakul T, Sang-A-kad P, Therakiatkumjorn C, Kunsuikmengrai K, Yeo JP. A survey study on diabetes management and complication status in primary care setting in Thailand. J Med Assoc Thai. 2007;90(1):65–71. | ||
Supapluksakul S, Ruamviboonsuk P, Chaowakul W. The prevalence of diabetic retinopathy in Trang province determined by retinal photography and comprehensive eye examination. J Med Assoc Thai. 2008;91(5):716–722. | ||
World Health Organization [webpage on the Internet]. Life tables by country: Thailand; 2014. Available from: http://apps.who.int/gho/data/?theme=main&vid=61640. Accessed October 15, 2014. | ||
Clarke P, Gray A, Holman R. Estimating utility values for health states of type 2 diabetic patients using the EQ-5D (UKPDS 62). Med Decis Making. 2002;22(4):340–349. | ||
Tengs TO, Wallace A. One thousand health-related quality-of-life estimates. Med Care. 2000;38(6):583–637. | ||
Australian Institute of Health and Welfare. The Burden of Disease and Injury in Australia. 2003. | ||
Carrington AL, Mawdsley SK, Morley M, Kincey J, Boulton AJ. Psychological status of diabetic people with or without lower limb disability. Diabetes Res Clin Pract. 1996;32(1–2):19–25. | ||
National Institute for Clinical Excellence. Guidance on the Use of Long-Acting Insulin Analogues for the Treatment of Diabetes – Insulin Glargine. 2002. | ||
Tanvejsilp P, Ngorsuraches S. Defining the scope of health technology assessment and types of health economic evaluation. J Med Assoc Thai. 2014;97(suppl 5):S10–S16. | ||
Maharaj Nakorn Chiang Mai Hospital. Pharmacy and Healthcare Service Fees. Chiang Mai: Maharaj Nakorn Chiang Mai Hospital; 2014. | ||
Pornpinatepong S. Cost-effectiveness analysis of diabetic retinopathy screening in type2 diabetes mellitus, Master Thesis, Bangkok, Mahidol University, 2005. | ||
Riewpaiboon A. Standard Cost Lists for Health Technology Assessment: Health Intervention and Technology Assessment Program (HITAP). Nonthaburi: HITAP; 2011. | ||
National Health Security Office. Schedule of Health Benefits and Fees. Bangkok: National Health Security Office; 2014. | ||
Teerawattananon Y, Mugford M, Tangcharoensathien V. Economic evaluation of palliative management versus peritoneal dialysis and hemodialysis for end-stage renal disease: evidence for coverage decisions in Thailand. Value Health. 2007;10(1):61–72. | ||
King Chulalongkorn Memorial Hospital. Pharmacy and Healthcare Service Fees. Bangkok: King Chulalongkorn Memorial Hospital; 2014. | ||
Bureau of Trade and Economics Indices, Ministry of Commerce [webpage on the Internet]. CPI 2014. Available from: www.price.moc.go.th/price/cpi/index_new_e.asp. Accessed October 12, 2014. | ||
Bank of Thailand [webpage on the Internet]. Foreign exchange rates 2015. Available from: https://www.bot.or.th/english/statistics/financialmarkets/exchangerate/_layouts/application/exchangerate/ExchangeRate.aspx. Accessed February 11, 2016. | ||
Drug and Medical Supply Information Center [homepage on the Internet]. 2015. Available from: http://dmsic.moph.go.th. Accessed April 15, 2016. | ||
Riewpaiboon A. Measurement of costs for health economic evaluation. J Med Assoc Thai. 2014;97(suppl 5):S17–S26. | ||
Rosenstock J, Wilson C, Fleck WP. Alogliptin versus glipizide monotherapy in elderly type 2 diabetes mellitus patients with mild hyperglycaemia: a prospective, double-blind, randomized, 1-year study. Diabetes Obes Metab. 2013;15(10):906–914. | ||
Pratley RE, Rosenstock J, Pi-Sunyeer FX, et al. Management of type 2 diabetes in treatment-naive elderly patients. Diabetes Care. 2007;30:3017–3022. | ||
Schweizer A, Dejager S, Bosi E. Comparison of vildagliptin and metformin monotherapy in elderly patients with type 2 diabetes: a 24-week, double-blind, placebo-controlled study. Diabetes Obes Metab. 2009;11:804–812. | ||
Schwartz SL. Treatment of elderly patients with type 2 diabetes mellitus: a systematic review of the benefits and risks of dipeptidyl peptidase-4 inhibitors. Am J Geriatr Pharmacother. 2010;8(5): | ||
Karagiannis T, Paschos P, Paletas K, Matthews DR, Tsapas A. Dipeptidyl peptidase-4 inhibitors for treatment of type 2 diabetes mellitus in the clinical setting: systematic review and meta-analysis. BMJ. 2012;344:e1369. | ||
Wu D, Li L, Liu C. Efficacy and safety of dipeptidyl peptidase-4 inhibitors and metformin as initial combination therapy and as monotherapy in patients with type 2 diabetes mellitus: a meta-analysis. Diabetes Obes Metab. 2014;16(1):30–37. | ||
Pfutzner A, Paz-Pacheco E, Allen E, Frederich R, Chen R; CV181039 Investigators. Initial combination therapy with saxagliptin and metformin provides sustained glycaemic control and is well tolerated for up to 76 weeks. Diabetes Obes Metab. 2011;13(6):567–576. | ||
Aschner P, Katzeff HL, Guo H, et al; Sitagliptin Study 049 Group. Efficacy and safety of monotherapy of sitagliptin compared with metformin in patients with type 2 diabetes. Diabetes Obes Metab. 2010;12(3): | ||
Williams-Herman D, Johnson J, Teng R, et al. Efficacy and safety of sitagliptin and metformin as initial combination therapy and as monotherapy over 2 years in patients with type 2 diabetes. Diabetes Obes Metab. 2010;12(5):442–451. | ||
Bosi E, Dotta F, Jia Y. Vildagliptin plus metformin combination therapy provides superior glycaemic control to individual monotherapy in treatment naive patients with type 2 diabetes mellitus. Diabetes Obes Metab. 2009;11:506–515. | ||
Schweizer A, Couturier A, Foley JE. Comparison between vildagliptin and metformin to sustain reductions in HbA(1C) over 1 year in drug-naive patients with type 2 diabetes. Diabet Med. 2007;24:955–961. | ||
Haak T, Meinicke T, Jones R, Weber S, von Eynatten M, Woerle HJ. Initial combination of linagliptin and metformin improves glycaemic control in type 2 diabetes: a randomized double-blind, placebo-controlled study. Diabet Obes Metab. 2012;14(6):565–574. | ||
Teerawattananon Y, Tritasavit N, Suchonwanich N, Kingkaew P. The use of economic evaluation for guiding the pharmaceutical reimbursement list in Thailand. Z Evid Fortbild Qual Gesundhwes. 2014;108(7):397–404. | ||
Health Technology Assessment Working Team. The Guidelines for Health Technology Assessment of Thailand. 2nd ed. Nonthaburi: Watcharin PP; 2014. | ||
Geng J, Yu H, Mao Y, Zhang P, Chen Y. Cost-effectiveness of dipeptidyl peptidase-4 inhibitors for type 2 diabetes. Pharmacoeconomics. 2015;33:581–597. | ||
Chan SP, Ji LN, Nitiyanant W, Baik SH, Sheu WH. Hypoglycemic symptoms in patients with type 2 diabetes in Asia-Pacific: real-life effectiveness and care patterns of diabetes management: the RECAP-DM study. Diabetes Res Clin Pract. 2010;89:e30–e32. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.