Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 15
Correlation of Obesity and Overweight with Cervical Vascular Function Among Healthy Populations
Authors Pan X, Chen X , Ren L, Li Z, Chen S
Received 26 July 2022
Accepted for publication 16 September 2022
Published 25 September 2022 Volume 2022:15 Pages 2927—2938
DOI https://doi.org/10.2147/DMSO.S383880
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Xiaoyu Pan,1,2 Xiaoyi Chen,2 Lin Ren,2 Zelin Li,1,2 Shuchun Chen1,2
1Department of Internal Medicine, Hebei Medical University, Shijiazhuang, People’s Republic of China; 2Department of Endocrinology, Hebei General Hospital, Shijiazhuang, People’s Republic of China
Correspondence: Shuchun Chen, Department of Endocrinology, Hebei General Hospital, Shijiazhuang, People’s Republic of China, Tel/Fax +86 31185988406, Email [email protected]
Purpose: To study the effects of obesity and overweight on carotid vascular function among healthy populations by carotid ultrasound (CAU) and transcranial Doppler (TCD).
Materials and Methods: Basic clinical characteristics, CAU and TCD parameters were collected from recruited healthy individuals. Firstly, all participants were divided into three groups: normal, overweight and obese. Then, the variability of basic clinical characteristics and lipids between the three groups was calculated. Subsequently, CAU and TCD parameters were compared between the three groups. Finally, the correlation between body mass index (BMI) and neck vascular function was analyzed.
Results: A total of 613 healthy participants were included, of whom 241 were normal, 264 were overweight, and 108 were obese. Overweight and obesity significantly decreased systolic, diastolic and mean flow velocities in the basilar, vertebral and internal carotid arteries, but had no effect on pulsatility index. In addition, BMI was significantly negatively correlated with systolic, diastolic, and mean flow velocities in the basilar, vertebral, and internal carotid arteries, and remained correlated after adjusting for other factors. There was no effect of overweight and obesity on carotid plaques.
Conclusion: Our study revealed that overweight and obesity decreased carotid vascular flow velocity and showed a decreasing trend in vascular flow velocity with increasing BMI. Overweight and obesity appear to have no effect on carotid plaques.
Keywords: obesity, overweight, basilar artery, vertebral artery, internal carotid artery
Introduction
In recent years, the rising prevalence of obesity and overweight has developed into a significant public health issue. Obesity and overweight are important risk factors for vascular diseases and greatly increase the risk of cardiovascular diseases when compared to people of normal weight.1,2 Obesity and overweight are also metabolic disorders, accompanied by changes in blood pressure, lipids and glucose.3 Additionally, an excessive buildup of adipose tissue secretes large quantities of adipokines, a group of reactive small molecules that can harm multiple organs.4 Obesity is accompanied by an increase in blood volume, basal cardiac output and heart rate, which can induce intimal hyperplasia through changes in vascular wall tension. Increased levels of oxidative stress and inflammation combined with metabolic abnormalities can damage the vascular endothelium and hence start the development of a number of cardiovascular illnesses. Vascular damage is closely related to the prevalence of insulin resistance and increased renin-angiotensin-aldosterone system activation in obese and overweight populations.5
The carotid artery (CA), vertebral artery (VA), and basilar artery (BA) are the main blood channels for the brain’s blood supply, and their malfunction is strongly linked to many cerebrovascular illnesses. Inadequate CA supply is linked to dizziness, slurred speech, and amnesia. Vertigo, headaches, and a lack of blood flow to the vertebral basilar system are all related. When vascular disease is severe, stroke can happen. Therefore, it is crucial to check for vascular function early on. Doppler ultrasound non-invasive approaches for detecting carotid and cerebrovascular abnormalities include carotid ultrasound (CAU) and transcranial Doppler (TCD) ultrasound. Both are useful instruments for the identification and evaluation of carotid vascular lesions and are essential for assessing vascular function as well as the efficacy of prevention and treatment of lesions.6 Numerous investigations evaluating neck vasculature in patients with diabetes, hypertension, and coronary artery disease utilizing CAU and TCD have demonstrated good sensitivity and specificity in disease prediction.7–10 Studies have revealed that TCD has an 88% specificity and a 91% sensitivity for the diagnosis of ischemic stroke.11 Therefore, the use of CAU and TCD for the detection of vascular function in the neck can lead to early detection of vascular dysfunction, which can lead to interventional treatment and reduce the possibility of serious disease.
There are no current publications that are pertinent to the effects of obesity and overweight on neck vascular function in healthy populations, despite the fact that the vascular damage produced by these conditions is widely recognized. CAU and TCD looked at the relationship between body mass index (BMI) and neck vascular function in this study. Obesity and overweight can be considered risk factors for neck vascular dysfunction. So that interventions can be carried out at an early stage, it is important to identify risk factors for vascular dysfunction in the neck as early as feasible.
Materials and Methods
Study Population
The study followed the principles of the Declaration of Helsinki and was approved by the Medical Ethics Committee of Hebei General Hospital (Ethics Committee No. 202,027). All participants signed an informed consent form before enrollment.
This is a cross-sectional study conducted in an outpatient setting. The participants included were healthy people who had a physical examination at Hebei General Hospital in June 2022. The population recruited for this study was healthy, so all participants with underlying diseases, such as cardiovascular disease, hypertension, and diabetes, were excluded.
Information and Biomarkers Collection
Basic information was collected from all participants, including gender, age, and medical history. Height, weight, systolic blood pressure (SBP), and diastolic blood pressure (DBP) were measured by professional staff. Blood samples were collected from participants after 8 hours of fasting. Fasting blood glucose, HbA1c, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), total cholesterol (TC), and triglyceride (TG) levels were collected. All blood biomarkers were tested in the same laboratory.
Transcranial Doppler Detection
The 2MHz multichannel TCD (DWL-BOXTCD, Germany) is routinely used in our hospital as a non-invasive screening test to identify vascular lesions through the acoustic window. The patient lies on his or her side and the probe position, angle, and detector depth are adjusted. The mean flow velocity, vascular pulsatility index, systolic flow velocity and diastolic flow velocity of the vertebral, basilar and internal carotid arteries were measured bilaterally through the parietal occipital window. The above data were collected as the average of three measurements.
Carotid Artery Ultrasound
CAU is non-invasive and highly sensitive, and can clearly display the internal diameter of blood vessels, sclerotic plaque type, morphology, distribution site, and carotid artery stenosis. A Philips color Doppler ultrasound diagnostic instrument equipped with an ultrasound probe (probe frequency of 7.5–12 MHz) was used. The patient was placed in a supine position, and the carotid vessels were fully exposed. The carotid vessels were scanned transversely and longitudinally, and the number and size of plaques were analyzed.
Statistical Analysis
All data were tested for normality. Continuous variables were expressed using the mean ± standard deviation, and the one-way ANOVA test was used to compare the differences between the three groups. The odds ratio test was used to assess the variability of categorical variables. Spearman or Pearson correlation analysis was used to determine the relationship between BMI and cervical vascular function parameters. Multiple linear regression analysis was used to determine independent correlations between BMI and cervical vascular function parameters. When P<0.05 considered the difference between groups was statistically significant. All data were processed using SPSS software version 26.0 and GraphPad Prism software version 8.0.
Results
Clinical Characteristics of All Participants
A total of 613 healthy participants (including 396 men and 217 women) were recruited into this study. All participants were classified according to BMI as normal weight (241), overweight (264), and obese (108). There were no significant differences (P>0.05) between the three groups for age, fasting glucose and HbA1c (Figure 1A–C). In normal weight, overweight and obese people, SBP was 123.1±17.37, 129.8±15.95 and 133.4±18.56mmHg, and DBP was 77.8±9.62, 81.63±11.14 and 84.91±11.81mmHg, respectively. Both obesity and overweight significantly increased SBP and DBP levels (p<0.001). Obesity mainly increased DBP levels compared to overweight (P<0.05). The mean blood pressure values were within the normal range in all three groups (Figure 1D and E).
Blood Lipids of All Participants
LDL-C and TC were not significantly different (p>0.05) between the three groups (Figure 2A and B). Obesity and overweight significantly reduced HDL-C levels, and the decrease was more pronounced with increasing weight (P<0.001) (Figure 2C). Obesity and overweight significantly increased TG levels compared to those of normal weight (P<0.001), but there was no significant difference between the obese and overweight groups (P>0.05) (Figure 2D).
Obesity and Overweight Affect BA Function Parameters
There was no significant effect of obesity and overweight on BA pulsatility index (P>0.05) (Figure 3A). Overweight decreased BA systolic flow and mean flow (P<0.05), but had no significant effect on diastolic flow (P>0.05). Obesity significantly reduced BA systolic flow, diastolic flow and mean flow (P<0.001), more significantly relative to overweight (P<0.05) (Figure 3B–D).
Obesity and Overweight Affect ICA Function Parameters
Obesity and overweight do not affect the bilateral ICA pulsatility index (P>0.05) (Figure 4A and B). Obesity significantly decreased bilateral ICA systolic, diastolic, and mean flow velocities, and overweight also significantly reduced right ICA systolic, diastolic, and mean flow velocities and left systolic flow (P<0.001), slightly lowered mean flow velocity (P<0.05), and did not affect diastolic flow velocity (P>0.05). Compared to overweight, obesity further reduced systolic, diastolic and mean flow velocities in the ICA bilaterally (P<0.01), except for left-sided diastolic flow velocities (P>0.05) (Figure 4C–H).
Obesity and Overweight Affect VA Function Parameters
Similarly, obesity and overweight do not affect the bilateral VA pulsatility index (P>0.05) (Figure 5A and B). Obesity significantly reduced systolic, diastolic and mean flow velocities in the VA bilaterally (P<0.001), with a relatively small reduction in overweight (P<0.05). Obesity and overweight have comparable effects on vertebral artery function (P>0.05), except for the left vertebral artery, which declines more markedly in obesity (P<0.05) (Figure 5C–H).
Correlation of BMI with BA, VA and ICA Function Parameters
BMI was negatively correlated with systolic, diastolic and mean flow velocities among bilateral BA, VA and ICA (P<0.001). However, there was no correlation between BMI and bilateral BA, VA and ICA pulsatility indices (P>0.05) (Table 1).
 |
Table 1 Correlation Between BMI and Cervical Vascular Function Parameters |
Multivariate Linear Correlation Analysis Between BMI and BA, VA and ICA Function Parameters
To investigate the independent correlation between BMI and BA, VA and ICA function, we developed three different models (model 1: crude model; model 2: adjusted for age, SBP and DBP; model 3: adjusted for age, SBP, DBP, fasting glucose and HbA1c). BMI was negatively associated with systolic, diastolic, and mean flow rates in bilateral BA, VA, and left ICA, regardless of model adjustment (P<0.001). BMI was negatively correlated with systolic and mean flow velocity in right ICA, despite model adjustment (P<0.001), but had no correlation with diastolic flow velocity after adjustment for crude model and a negative correlation after adjustment for model 1 and model 2 (P<0.01). There was still no correlation between BMI and BA, VA and ICA pulsatility indices after model adjustment (P>0.05) (Table 2, and Figure 6).
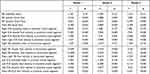 |
Table 2 Correlation Between BMI and Cervical Vascular Function After Adjustment for Confounding Factors |
Obesity and Overweight Affect Carotid Plaque
The odds ratio test showed that obesity and overweight had no significant effect on the presence or absence of carotid plaque (P>0.05) (Table 3). As well, the number of carotid plaques and the volume of the largest plaque did not vary significantly between the three groups (P>0.05) (Figure 7A–C).
 |
Table 3 Obesity and Overweight Affect Carotid Plaque |
Discussion
Due to the rising level of living, many people’s lives have changed and their weight is constantly rising, contributing to an increase in the prevalence of obesity and overweight. In addition to being a substantial contributor to the development of cardiovascular and cerebrovascular illnesses, obesity also contributes to a markedly higher rate of morbidity and death in obese people than in the general population.12 As a result, early cerebrovascular screening for obese and overweight individuals can aid in the disease’s early treatment.
According to certain research, obese adults are 1.86 times more likely to die suddenly and have a 40% higher risk of having cerebrovascular illness than the general population.1 This is explained by the fact that as body weight rises, the endocrine system is disturbed, TC and TG levels rise, HDL-C levels fall, and atherosclerosis is predisposed as a result.13 The findings of this investigation on obese and overweight individuals demonstrated that these conditions markedly lowered HDL-C levels and elevated TG levels. The limited population size and the inclusion of a healthy population may have contributed to the lack of a significant difference in TC and LDL-C between the three groups. The likelihood of developing hypertension and vascular injury in obese and overweight people is raised by the rise in blood volume that occurs as weight increases, hyperactivation of the renin-angiotensin system, increased levels of inflammation, and oxidative stress in vivo. SBP and DBP in the obese and overweight groups were significantly higher than in the normal weight population, however these mean blood pressure readings did not fulfill the standards for a diagnosis of hypertension. This better illustrates the relationship between body weight and aberrant neck vascular function since it corresponds with our recruitment sample, which eliminates vascular damage brought on by hypertension alone. In obese people, the relative insufficiency of insulin secretion by islet cells results in hunger, which prompts greater eating and weight gain, which in turn exacerbates the relative insufficiency of insulin secretion and eventually leads to the onset of diabetes mellitus.14,15 Diabetes can result in glassy small arteries and hypertension, which can contribute to cerebrovascular illness.16 According to our study’s findings, those who are obese, overweight, or normal weight have identical fasting glucose and HbA1c levels. This finding rules out the impact of blood sugar levels on the vasculature and establishes a link between body weight and neck vascular health.
The primary blood vessels for the brain are the ICA, VA, and BA, and when these blood vessels are dysfunctional, there may not be enough blood flowing to the brain, which can cause a variety of clinical symptoms. Vascular spasm, sclerosis, and stenosis are typically linked to decreased vascular flow rates. Early vascular lesions are predicted to manifest when vascular flow velocity declines. The pulsatility index is thought to be a predictor of vascular flexibility and compliance.17 According to studies, vascular compliance is higher in healthy individuals and lower in patients with ischemic cerebrovascular and advanced disease.18 Therefore, pulsatility index and blood flow velocity measurements can, to some extent, indicate vascular function. The findings of this study demonstrate that weight gain and obesity have no impact on the pulsatility index for ICA, VA, and BA. This illustrates that the vessels’ compliance and elasticity are still within a normal range. However, vascular systolic, diastolic, and mean flow velocities are decreased with obesity and overweight, indicating some degree of vascular function impairment. We conducted more carotid plaque studies to see whether the decrease in flow velocity is related to stenosis. According to CAU findings, there were no appreciable changes in carotid plaque presence, size, or number between healthy people of normal weight and those who were obese or overweight.
Even after accounting for a number of variables, the findings of multiple linear regression revealed a strong inverse relationship between BMI and vascular blood flow velocity. No matter how any risk factor was adjusted, there was still no discernible relationship between BMI and pulsatility index. So, in a group of healthy people, we hypothesize that obesity and overweight have some effect on neck artery function, but not in a way that appears to cause stenosis and lower vascular compliance. Reduced capillary blood flow in obese and overweight people appears to be mostly due to impaired vascular endothelial cell function caused by elevated blood pressure, lipids, inflammation, and oxidative stress in vivo.19 In summary, our study found that an increase in BMI in a healthy population significantly reduced neck vascular systolic, diastolic and mean flow velocities without macrovascular lesions, indicating that vascular lesions are in an early stage. In order to detect and treat cerebrovascular illness early, it is therefore advantageous to screen neck vascular function in obese and overweight populations.
Our study does have some limitations, though. First of all, because this research was cross-sectional, it was impossible to establish a causal link between BMI and cervical vascular function. Second, there was a small sample size in this single-center clinical trial. The pulsatility index was not significantly correlated with BMI, making it impossible for it to accurately depict the vascular damage brought on by BMI.
Conclusions
In conclusion, our study found a significant negative association between BMI and cervical vascular flow velocity, with or without adjusting for confounding factors. This finding implies that in healthy people, obesity and overweight are risk factors for early cervical vascular dysfunction.
Data Sharing Statement
The data presented in this study are available on request from the corresponding author.
Ethics Approval and Consent to Participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Hebei General Hospital (Date May 8, 2020/No. 202027).
Funding
No funding was received to assist with the preparation of this manuscript.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Marini S, Merino J, Montgomery BE, et al. Mendelian randomization study of obesity and cerebrovascular disease. Ann Neurol. 2020;87(4):516–524. doi:10.1002/ana.25686
2. Battineni G, Sagaro GG, Chintalapudi N, Amenta F, Tomassoni D, Tayebati SK. Impact of obesity-induced inflammation on Cardiovascular Diseases (CVD). Int J Mol Sci. 2021;22(9):4798. doi:10.3390/ijms22094798
3. Swayze S, Rotondi M, Kuk JL. The associations between blood and urinary concentrations of metal metabolites, obesity, hypertension, type 2 diabetes, and dyslipidemia among US adults: NHANES 1999–2016. J Environ Public Health. 2021;2021:2358060. doi:10.1155/2021/2358060
4. El Mulla KF, El Abd A, Donia HM, Hussein RM, Eid AA. Serum lipocalin-2 and carotid artery intima-media thickness in relation to obesity in eugonadal males over forty with venogenic erectile dysfunction. Andrologia. 2021;53(8):e14127. doi:10.1111/and.14127
5. Koenen M, Hill MA, Cohen P, Sowers JR. Obesity, adipose tissue and vascular dysfunction. Circ Res. 2021;128(7):951–968. doi:10.1161/CIRCRESAHA.121.318093
6. Chiba T, Fujiwara S, Oura K, et al. Superb microvascular imaging ultrasound for cervical carotid artery stenosis for prediction of the development of microembolic signals on transcranial Doppler during carotid exposure in endarterectomy. Cerebrovasc Dis Extra. 2021;11(2):61–68. doi:10.1159/000516426
7. Hoke M, Schillinger M, Minar E, Goliasch G, Binder CJ, Mayer FJ. Carotid ultrasound investigation as a prognostic tool for patients with diabetes mellitus. Cardiovasc Diabetol. 2019;18(1):90. doi:10.1186/s12933-019-0895-0
8. Naqvi TZ, Lee MS. Carotid intima-media thickness and plaque in cardiovascular risk assessment. JACC Cardiovasc Imaging. 2014;7(10):1025–1038. doi:10.1016/j.jcmg.2013.11.014
9. Mol A, Meskers CGM, Sanders ML, et al. Cerebral autoregulation assessed by near-infrared spectroscopy: validation using transcranial Doppler in patients with controlled hypertension, cognitive impairment and controls. Eur J Appl Physiol. 2021;121(8):2165–2176. doi:10.1007/s00421-021-04681-w
10. Vidyashree M, Deepeshwar S, Nagarathna R, et al. Transcranial Doppler studies in Type 2 diabetes mellitus: a systematic review. Diabetes Res Clin Pract. 2022;186:109808. doi:10.1016/j.diabres.2022.109808
11. Finnsdóttir H, Szegedi I, Oláh L, Csiba L. The applications of transcranial Doppler in ischemic stroke. A transcranialis Doppler-ultrahang alkalmazása ischaemiás stroke-ban. Ideggyogy Sz. 2020;73(11–12):367–378. doi:10.18071/isz.73.0367
12. La Sala L, Pontiroli AE. Prevention of diabetes and cardiovascular disease in obesity. Int J Mol Sci. 2020;21(21):8178. doi:10.3390/ijms21218178
13. Scicchitano P, Cortese F, Gesualdo M, et al. The role of endothelial dysfunction and oxidative stress in cerebrovascular diseases. Free Radic Res. 2019;53(6):579–595. doi:10.1080/10715762.2019.1620939
14. Lejawa M, Osadnik K, Czuba Z, Osadnik T, Pawlas N. Association of metabolically healthy and unhealthy obesity phenotype with markers related to obesity, diabetes among young, healthy adult men. analysis of MAGNETIC study. Life. 2021;11(12):1350. doi:10.3390/life11121350
15. Louters M, Pearlman M, Solsrud E, Pearlman A. Functional hypogonadism among patients with obesity, diabetes, and metabolic syndrome. Int J Impot Res. 2021:1–7. doi:10.1038/s41443-021-00496-7
16. Bae YJ, Shin SJ, Kang HT. Body mass index at baseline directly predicts new-onset diabetes and to a lesser extent incident cardio-cerebrovascular events, but has a J-shaped relationship to all-cause mortality. BMC Endocr Disord. 2022;22(1):123. doi:10.1186/s12902-022-01041-3
17. Zhang X, Wu Q, Wang Z, Li H, Dai J. Keap1-Nrf2/ARE signal pathway activated by butylphthalide in the treatment of ischemic stroke. Am J Transl Res. 2022;14(4):2637–2646.
18. Ormerod E, Ali K, Cameron J, et al. The association between arterial stiffness, initial stroke severity, and 3-week outcomes in patients with ischemic stroke. J Stroke Cerebrovasc Dis. 2017;26(11):2541–2546. doi:10.1016/j.jstrokecerebrovasdis.2017.05.043
19. Shen Q, Zhang G. Depletion of microglia mitigates cerebrovascular dysfunction in diet-induced obesity mice. Am J Physiol Endocrinol Metab. 2021;321(3):E367–E375. doi:10.1152/ajpendo.00086.2021
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.







