Back to Journals » Clinical Ophthalmology » Volume 10
Correlation between Hertel exophthalmometric value and refraction in young Cameroonian adults aged 20 to 40 years
Authors Dohvoma V , Epee E, Ebana Mvogo SR , Lietcheu N S, Ebana Mvogo C
Received 3 May 2016
Accepted for publication 4 June 2016
Published 29 July 2016 Volume 2016:10 Pages 1447—1451
DOI https://doi.org/10.2147/OPTH.S111915
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Viola A Dohvoma, Emilienne Epée, Stève R Ebana Mvogo, N Sandra Lietcheu, Côme Ebana Mvogo
Department of Ophthalmology, Faculty of Medicine and Biomedical Sciences, University of Yaoundé I, Yaoundé, Cameroon
Purpose: To study the relationship between exophthalmometric value (EV) and refractive error in Cameroonian young adults.
Patients and methods: A prospective descriptive study was carried out in the ophthalmic unit of the Yaoundé Central Hospital from March to May 2015. Consenting patients aged 20–40 years with no intraocular pathology who were seen for refractive errors were included. Ocular protrusion was measured using the Hertel exophthalmometer. Automatic refraction was done following cycloplegia with cyclopentolate and tropicamide.
Results: A total of 200 patients were included (68% females and 32% males). The mean age was 27.2±6 years. Hyperopia was the most common refractive error (51%), followed by hyperopic astigmatism (19.3%). EV varied between 9 mm and 23 mm, with a mean of 14.8±2.5 mm in the right eye and 15.0±2.5 mm in the left eye. The mean EVs were 17.10±2.80 mm in myopia, 14.24±1.92 mm in hyperopia, 16.72±2.58 mm in myopic astigmatism, 14.07±2.19 mm in hyperopic astigmatism, and 14.77±2.40 mm in mixed astigmatism. The spherical value had a negative correlation with EV (P=0.0000).
Conclusion: The mean EV of this Cameroonian population is smaller than that of other populations and is consistent with the known characteristic hyperopic status of the population. A study on a larger sample will determine the normative data of absolute and relative EV in our setting.
Keywords: refractive error, exophthalmometry, Cameroon
Introduction
Exophthalmometry is the clinical measurement of the anteroposition of the globe in the orbit. It is the distance between the surface of the cornea and the lateral orbital rim.1 Hertel exophthalmometry is commonly used to measure the protrusion of the globe. There are various exophthalmometers, and studies comparing different types have shown comparable accuracy.2,3 Ocular protrusion has been shown to vary with ethnicity, as different authors have reported different values in different ethnic populations.4–6 Normal accepted protrusion in Caucasians is <21 mm.7 Other factors such as age and refraction also influence ocular protrusion.6,8
The refractive power of the eye results from the relationship between the optical properties of the various components of the eye and the axial length. A refractive error may be defined as a state in which the optical system of the nonaccommodating eye fails to bring parallel rays of light to focus on the retina. Axial length plays a major role in the ocular biometry and refraction and has been shown to correlate well with spherical equivalence.9 A positive correlation is also reported between axial length and ocular protrusion. According to Chen et al, ocular protrusion increases with increasing axial length and spherical equivalence in myopic eyes. The globe tends to expand backward and forward, and with the increasing axial length, the ocular protrusion appears to be more obvious. Thus, refractive errors can be correlated to ocular protrusion.10
Previous studies on refraction in our setting reported a predominantly hyperopic population.11 We found no study on ocular protrusion in our setting. The aim of this study was to find out if there is a correlation between the refraction and ocular protrusion in Cameroonian adults aged 20–40 years.
Patients and methods
A prospective descriptive study was carried out at the ophthalmic unit of the Yaoundé Central Hospital from March to May 2015. Our study was reviewed and approved by the Institutional Ethical Clearance Committee of the Faculty of Medicine and Biomedical Sciences of the University of Yaoundé I. Written informed consent was obtained from all participants. Sampling was consecutive, and all consenting patients aged 20–40 years who came for consultation during the study period were included. Monophthalmic patients and those with a history of orbital trauma or disease, endocrine disease, congenital glaucoma, or craniofacial malformations were excluded.
Patients underwent ophthalmic examination that comprised measuring uncorrected distant visual acuity, slit lamp examination, Hertel exophthalmometry, automatic refraction under cycloplegia, and funduscopy with a 78 D lens on the slit lamp. Hertel exophthalmometry was done for all cases by a single ophthalmologist using Hertel exophthalmometer (Oculus Inc., Wetzlar, Germany). Cycloplegia was obtained by alternatively instilling one drop of cyclopentolate 0.5% and one drop of tropicamide 0.5% at intervals of 5 minutes for a total of three drops per cycloplegic agent. Refraction was measured 20–30 minutes after the last drop.
Ocular protrusion was considered normal when the exophthalmometric value (EV) was <20 mm and the interocular difference was <2 mm. Relative exophthalmos was defined as an interocular difference in the EV of ≥2 mm. Refractive error was classified as follows: hyperopia, myopia, hyperopic astigmatism, myopic astigmatism, and mixed astigmatism. Data collected included age, sex, objective refraction, and EV. Data analysis was done using SPSS 20.0 (IBM Corporation, Armonk, NY, USA). Pearson’s correlation, Student’s t-test, and Fisher’s exact test were used. Significance was set at P<0.05.
Results
A total of 200 patients were included in this study, among whom 68% were females (n=137) and 32% were males (n=63). The mean age was 27.17±5.96 years. Hyperopia was the most common refractive error (51%), followed by hyperopic astigmatism (19.3%). The distribution of the study population with respect to refractive error is shown in Figure 1. There was no significant difference in the distribution of refractive errors between the right and left eyes (P=0.05). There was no significant difference in the type of refractive error between males and females (P=0.62). There was no significant difference in the distribution of the type of refractive error with respect to the age group (P=0.5).
Ocular protrusion varied between 9 mm and 23 mm. The mean was 14.82±2.50 mm for the right eye and 14.97±2.46 mm for the left eye (P=0.9). The mean EV among females was 14.86±2.60 mm, and among males it was 14.95±2.25 mm. There was no statistically significant difference between the mean EV of males and females (P=0.98 for the right eye and P=0.67 for the left eye). Figure 2 shows that the majority of cases (91%) had normal EVs. The group with EV >20 mm was composed of five cases of myopia and four cases of myopic astigmatism. Those with values <12 mm comprised 15 cases of hyperopia, six cases of hyperopic astigmatism, five cases of mixed astigmatism, and one case of myopic astigmatism.
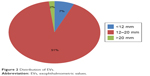  | Figure 2 Distribution of EVs. |
Relative exophthalmos was found in 8% of cases (n=16). Eight of the cases had anisometropia. There was a weak but significant negative correlation between ocular protrusion and age (r=−0.02, P=0.025). There was a strong significant negative correlation between the spherical value and the EV (r=−0.37, P=0.0000 for the right eye; r=−0.29, P=0.0000 for the left eye). Figure 3 shows the mean EV in the various types of refractive errors, with the highest found in myopia followed by myopic astigmatism. The mean EV was 17.10±2.80 mm in myopia, 14.24±1.92 mm in hyperopia, 16.72±2.58 mm in myopic astigmatism, 14.07±2.19 mm in hyperopic astigmatism, and 14.77±2.40 mm in mixed astigmatism.
Discussion
This was a monocentric study with the study site being a public hospital that receives patients of all social status, from all regions of the country. This gave a sample that fairly represents the entire country.
The effect of age on the growth of the globe is described in the literature.12 Axial length increases with increasing age. This growth of the globe leads to increasing EV. Kashkouli et al8 reported a positive correlation between age and ocular protrusion in children and teenagers (6–19 years). Similarly, Lang et al13 reported that ocular protrusion increased steadily from the third to the 20th year of life. It was for this reason that the lower age limit of the study population was set at 20 years. The choice of the upper limit at 40 years was to eliminate changes in refraction owing to the aging lens. The risk of oxidative damage increases in the fourth decade when a barrier to the transport of glutathione forms around the lens nucleus.14 The population in this study was aged between 20 years and 40 years and can therefore be considered as being homogeneous in terms of growth and aging.
The most frequent refractive error in this study was hyperopia, followed by hyperopic astigmatism. These are the most frequent refractive errors in the Cameroonian non-albino population as reported by Ebana Mvogo et al.11 The role of melanin in the type of refractive error is yet to be clearly defined, as a study on refractive errors in albinos in our setting revealed myopic astigmatism to be the most common refractive error.15 Racial variations in the prevalence of refractive errors have been reported by several authors.16–18
Sex had no influence on the distribution of refractive errors. Some authors’ findings corroborate this,11,19 while others do not. Some authors have reported myopia risk to be associated with female sex.20 Differences in methods, definitions, and demographics can explain these differences. Age had no influence on the type of refractive error in this study population.
The mean EV was 14.82±2.50 mm for the right eye and 14.97±2.46 mm for the left eye. There was no significant difference between the right and left eyes. Wu et al5 reported a similar finding. However, some authors reported right eye protrusion to be greater,8 and others reported left eye protrusion to be greater.13
The mean EV in females was not significantly different from that in males; it was 14.86±2.60 mm and 14.95±2.25 mm for females and males, respectively. These values are lower than those reported by Migliori and Gladstone,21 which were 16.5 mm in White men, 18.5 mm in Black men, 15.4 mm in White women, and 17.8 mm in Black women. The mean reported in a Turkish population was 16.1±2.6 mm for males and 15.5±2.6 mm for females.6 In a Chinese Han adult population, the mean for females was 15.7±1.8 mm for the right eye and 15.8±1.8 mm for the left eye. For males, 15.7±1.8 mm for the left eye and 15.8±1.8 mm for the right eye.5 EVs differ by race, and this is possibly due to differences in facial structures and ocular anatomy. Wu et al5 concluded that diagnosing proptosis by using data from other countries and races to evaluate ocular protrusion is not appropriate.
The upper normal limits of the EV (mean + 2SD) for males and females were 19.45 mm and 20.06 mm, respectively, in this study. These values are lower than those reported among White Americans by Cole et al,2 which were 22.3 mm in males and 21.99 mm in females. Values reported by Fledelius and Stubgaard,22 in White Europeans aged 19–80 years, were 21.1 mm in males and 19.4 mm in females. Upper limits in adult Iranians (19.2–19.4 mm)8 and Chinese Han populations (19.3 mm)5 are closer to those reported here.
The maximum interocular difference in this study was 4 mm. However, other studies have reported a maximum asymmetry of 2 mm between both eyes.4,21 Anisometropia can explain the interocular differences. Anisometropic eyes have been shown to have greater axial length asymmetry than nonanisometropic eyes.23 Protrusion has equally been shown to vary with axial length.10 How genetic and environmental factors cause an interocular difference in axial length growth is still not fully understood.
EVs increased with decreasing spherical value. In some studies, myopia of <−6 D was eliminated. Conflicting results are reported. Some reported a negative correlation,6 like that found in this study, while others reported the absence of any correlation.24
Conclusion
The mean EV of this Cameroonian population differs from that of other populations and correlates with the characteristic hyperopic status of the population. The upper EV limit is consequently different from that in other populations. A study with a larger sample can provide much more valuable data about exophthalmometric measurements that will help determine the normative data of absolute and relative EVs in our setting.
Disclosure
The authors report no conflicts of interest in this work.
References
Davanger M. Principles and sources of error in exophthalmometry. A new exophthalmometer. Acta Ophthalmol (Copenh). 1970;48(4):625–633. | ||
Cole HP, Couvillion JT, Fink AJ, Haik BG, Kastl PR. Exophthalmometry: a comparative study of the Naugle and Hertel instruments. Ophthal Plast Reconstr Surg. 1997;13(3):189–194. | ||
Chang AA, Bank A, Francis IC, Kappagoda MB. Clinical exophthalmometry: a comparative study of the Luedde and Hertel exophthalmometers. Aust N Z J Ophthalmol. 1995;23(4):315–318. | ||
Osuobeni EP, al-Harbi AA. Normal values of ocular protrusion in Saudi Arabian male children. Optom Vis Sci. 1995;72(8):557–564. | ||
Wu D, Liu X, Wu D, et al. Normal values of Hertel exophthalmometry in a Chinese Han population from Shenyang, Northeast China. Sci Rep. 2015;5:8526. | ||
Karti O, Selver OB, Karahan E, Zengin MO, Uyar M. The effect of age, gender, refractive status and axial length on the measurements of hertel exophthalmometry. Open Ophthalmol J. 2015;9:113–115. | ||
Ducasse A. Conduite pratique à tenir devant une exophtalmie [Practical management of proptosis]. J Fr Ophtalmol. 2009;32(8):581–588. French. | ||
Kashkouli MB, Nojomi M, Parvaresh MM, Sanjari MS, Modarres M, Noorani MM. Normal values of hertel exophthalmometry in children, teenagers, and adults from Tehran, Iran. Optom Vis Sci. 2008;85(10):1012–1017. | ||
Touzeau O, Allouch C, Borderie V, Kopito R, Laroche L. Corrélation entre la réfraction et la biométrie oculaire [Correlation between refraction and ocular biometry]. J Fr Ophtalmol. 2003;26(4):355–363. French. | ||
Chen M, Zhou X-T, Xue A-Q, et al. [Myopic proptosis and the associated changes in axial components of the eye]. Zhonghua Yan Ke Za Zhi. 2007;43(6):525–529. Chinese. | ||
Ebana Mvogo C, Bella-Hiag AL, Ellong A, Metogo Mbarga B, Litumbe NC. Les amétropies statiques du noir camerounais [Static ametropias of black Cameroonians]. Ophthalmologica. 2001;215(3):212–216. French. | ||
Fledelius HC, Christensen AS, Fledelius C. Juvenile eye growth, when completed? An evaluation based on IOL-Master axial length data, cross-sectional and longitudinal. Acta Ophthalmol. 2014;92(3):259–264. | ||
Lang J, Schäfer WD, Grafen W, Wallner B. Über Seitenunterschiede der Lage des Hornhautscheitelpunktes zum lateralen Orbitarand (Messungen mit dem Exophthalmometer nach Hertel) [Side differences in the position of the corneal apex in relation to the lateral orbital margin (measurements with the Hertel exophthalmometer)]. Klin Monatsbl Augenheilkd. 1985;187(6):521–524. German. | ||
Michael R, Bron AJ. The ageing lens and cataract: a model of normal and pathological ageing. Philos Trans R Soc B Biol Sci. 2011;366(1568):1278–1292. | ||
Mvogo CE, Bella-Hiag AL, Ellong A, Mbarga BM. Les troubles visuels de l’albinos. Étude hospitalière réalisée à l’Hôpital général de Douala [Visual problems in albinos: a hospital study carried out at the Douala General Hospital]. Cah Détudes Rech Francoph Santé. 1999;9(2):89–91. French. | ||
Pan C-W, Klein BE, Cotch MF, et al. Racial variations in the prevalence of refractive errors in the United States: the multi-ethnic study of atherosclerosis. Am J Ophthalmol. 2013;155(6):1129.e–1138.e. | ||
Midelfart A, Kinge B, Midelfart S, Lydersen S. Prevalence of refractive errors in young and middle-aged adults in Norway. Acta Ophthalmol Scand. 2002;80(5):501–505. | ||
Kleinstein RN, Jones LA, Hullett S, et al. Refractive error and ethnicity in children. Arch Ophthalmol. 2003;121(8):1141–1147. | ||
Ayed T, Sokkah M, Charfi O, El Matri L. Épidémiologie des erreurs réfractives chez des enfants scolarisés, socio-économiquement défavorisés en Tunisie [Epidemiologic study of refractive errors in schoolchildren in socioeconomically deprived regions in Tunisia]. J Fr Ophtalmol. 2002;25(7):712–717. French. | ||
Dandona R, Dandona L, Srinivas M, et al. Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci. 2002;43(3):615–622. | ||
Migliori ME, Gladstone GJ. Determination of the normal range of exophthalmometric values for black and white adults. Am J Ophthalmol. 1984;98(4):438–442. | ||
Fledelius HC, Stubgaard M. Changes in eye position during growth and adult life as based on exophthalmometry, interpupillary distance, and orbital distance measurements. Acta Ophthalmol (Copenh). 1986;64(5):481–486. | ||
O’Donoghue L, McClelland JF, Logan NS, Rudnicka AR, Owen CG, Saunders KJ. Profile of anisometropia and aniso-astigmatism in children: prevalence and association with age, ocular biometric measures, and refractive status. Invest Ophthalmol Vis Sci. 2013;54(1):602–608. | ||
Chan W, Madge SN, Senaratne T, et al. Exophthalmometric values and their biometric correlates: the Kandy Eye Study. Clin Experiment Ophthalmol. 2009;37(5):496–502. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.