Back to Journals » International Journal of General Medicine » Volume 15
Correlation and Prognostic Assessment of Low T3 Syndrome and Norepinephrine Dosage for Patients with Sepsis: A Retrospective Single-Center (Cohort) Study
Authors Zhang J, Fu S, Liu F, Wan J, Wu S, Jiang G, Tao W , Zhou W, Qian K
Received 17 February 2022
Accepted for publication 27 April 2022
Published 10 May 2022 Volume 2022:15 Pages 4837—4847
DOI https://doi.org/10.2147/IJGM.S362748
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Jian-guo Zhang,1– 3,* Shang-miao Fu,1,* Fen Liu,1 Jian-guo Wan,4 Shu-bing Wu,4 Guang-hui Jiang,4 Wen-qiang Tao,1 Wen Zhou,4 Ke-jian Qian1
1Department of Critical Care Medicine, First Affiliated Hospital of Nanchang University, Nanchang, Jiangxi, People’s Republic of China; 2Department of Infection, First Affiliated Hospital of Nanchang University, Nanchang, Jianxi, People’s Republic of China; 3Department of Critical Care Medicine, Linyi People’s Hospital, Linyi, Shandong, People’s Republic of China; 4Department of Critical Care Medicine, First Hospital of Nanchang, Nanchang, Jiangxi, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ke-jian Qian, Department of Critical Care Medicine, First Affiliated Hospital of Nanchang University, No. 17 YongwaiZheng Street, Nanchang, Jiangxi, 330006, People’s Republic of China, Email [email protected] Wen Zhou, Department of Critical Care Medicine, First Hospital of Nanchang, No. 128 Xiangshan North Road, Nanchang, Jiangxi, 330006, People’s Republic of China, Email [email protected]
Purpose: To investigate the correlation and prognostic significance of low triiodothyronine (T3) syndrome and norepinephrine dosage in patients with sepsis and septic shock.
Methods: This single-center, retrospective, cohort study enrolled 169 patients with sepsis and septic shock that were admitted to the intensive care unit of First Hospital of Nanchang, Nanchang, China from June 2017 to July 2019. All included patients were followed up for 28 days or died, whichever was earlier. Patients with free T3 (FT3) of < 3.1 pmol/L were considered with low T3 syndrome. The correlation and prognostic significance of the FT3 and maximum dosage of norepinephrine (MDN) within 72 h, as well as other clinical indicators, were analyzed by using correlation analysis, principal component analysis, receiver operating characteristic curve, Youden index, and logistic regression.
Results: A total of 138 patients were allocated to the low T3 group. FT3 inversely correlated with the Sequential Organ Failure Assessment (SOFA) score within 24 h, fluid resuscitation volume within 24 h, and lactic acid levels, and positively correlated with the mean arterial pressure. The critical values of age, SOFA, and MDN for predicting the 28-day mortality were 79.5 years, 8.5 points, and 0.61 μg/kg/min, respectively. The mortality of the low T3 and normal T3 groups was similar. Considering the MDN of 0.61 μg/kg/min as the cutoff value, the mortality between the two groups was significantly different.
Conclusion: Among patients with sepsis and septic shock, FT3 was inversely correlated with the disease severity. An MDN ≥ 0.61 μg/kg/min within 72 h may be an important prognostic indicator.
Keywords: euthyroid sick syndromes, low T3 syndrome, non-thyroidal illness syndrome, norepinephrine, sepsis, septic shock
Introduction
Low triiodothyronine (T3) syndrome (LTS), also known as euthyroid sick syndrome or non-thyroid illness syndrome, is characterized by changes in serum levels of thyroid hormone in patients with normal baseline thyroid function and is usually caused by acute stress conditions, such as injury, surgery, various infectious diseases, and acute myocardial infarction.1 The main feature of this syndrome is a decreased free T3 (FT3) level, while the thyroid-stimulating hormone (TSH) level remains within the reference range. Considering that the thyroid hormone finely modulates energy metabolism, LTS appears to be an adaptive process to counterbalance catabolism during illness.2 However, research results from several studies do not agree with the above point of view.3–5 Critically ill patients with LTS, who were characterized by increasing consumption and imbalanced immunity during the acute phase, usually have longer intensive care unit (ICU) stay and higher mortality.6 In addition, a study demonstrated the important role of FT3 in recognizing susceptibility and degrees of debilitation among elderly patients.7 However, the effect of LTS on patient morbidity remains unclear.
Sepsis and septic shock are complex disease processes involving life-threatening organ dysfunction, which is induced by a dysregulated host response to infection. These disease processes remain associated with considerably high mortality despite the administration of bundle therapy within 1 h of admission, which includes antibiotics and fluid resuscitation.8 In bundle therapy, norepinephrine is the prioritized agent if a vasopressor is needed to treat septic shock. The norepinephrine dosage must be adjusted according to the patient’s presenting condition so that the mean arterial pressure (MAP) can be increased to more than 65 mm Hg. A previous study showed the difference in the 28-day mortality between the high-dosage norepinephrine group (≥ 416 µg/kg/week) and the low-dosage norepinephrine group (< 416 µg/kg/week) was not significant.9 The cut-off value of the grouping was 416 μg/kg/week, that is, 0.04 µg/kg/min. Although there was no uniform standard for grouping patients in the clinic, the dosage of 0.04 µg/kg/min was too small.10 On the contrary, another study showed that a maximum dosage of norepinephrine, which was ≥ 0.6 µg/kg/min, was notably associated with 7-day mortality in patients with septic shock.11 Although the duration of mortality studied was different between the two reports, the correlation between the norepinephrine dosage and prognosis in patients with septic shock remains unclear.
To date, the correlation between sepsis and FT3, as well as the prognostic value of norepinephrine dosage in patients with septic shock needs better clarity.12 Therefore, this current study aimed to investigate the correlation and prognostic significance of LTS and norepinephrine dosage in patients with sepsis and septic shock.
Materials and Methods
Study Population
This single-center, retrospective, cohort study enrolled consecutive patients with sepsis and septic shock that were admitted to the ICU of the First Hospital of Nanchang, Nanchang, Jiangxi Province, China between June 2017 and July 2019. The follow-up duration was 28 days or until the death of the patient, whichever was earlier.
Inclusion criteria for eligible patients were as follows: (i) age ≥ 18 years; (ii) diagnosis of sepsis and septic shock; (iii) serum level of thyroid hormone within the first 24 h after ICU admission; (iv) administration of norepinephrine as the initial vasopressor. Exclusion criteria were as follows: (i) primary thyroid disease; (ii) autoimmune disease; (iii) malignant tumor; (iv) pregnancy; (v) recent intake of drugs, such as amiodarone, carbamazepine, lithium, phenytoin, heparin, interferons, and interleukins, or submission to chemotherapy that could affect thyroid metabolism. Patients with suspected infection whose Sequential Organ Failure Assessment (SOFA) score ≥ 2 can be diagnosed with sepsis.8 Septic shock was diagnosed if the level of serum lactic acid was more than 2 mmol/L or vasopressor was needed to maintain MAP ≥ 65 mm Hg after adequate fluid resuscitation.8
Patient Evaluation
The thyroid hormone levels were evaluated during the first 24 h of ICU admission and measured in all patients via chemiluminescent immunoassay. In compliance with a previous study,13 the reference ranges for the thyroid hormones were as follows: TSH, 0.27–4.2 µIU/mL; FT3, 3.1–6.8 pmol/L; and free T4 (FT4), 12–22 pmol/L. According to the level of FT3, all included patients were divided into two groups: the low T3 group (FT3 < 3.1 pmol/L) and the normal group (TSH, FT3, and FT4 were all normal).
Demographic data included age, sex, and underlying diseases (comorbidities included in the Charlson Comorbidity Index,14 any condition that may affect thyroid hormone levels, coronary artery disease, and hypertension). The following clinical data were obtained from the electronic medical records of the included patients: infection diagnosis, initial vital signs (heart rate [HR], respiratory rate [RR], MAP, and body temperature) at the time of ICU admission, indicators within the first 24 h (thyroid hormone levels [TSH, FT3, FT4], SOFA score,15 procalcitonin [PCT], and fluid resuscitation volume), lactic acid levels at the time of ICU admission and the second 24 h, the maximum dosage of norepinephrine (MDN) within 72 h in patients with septic shock, microbiological results and adjunctive treatment (erythrocyte infusion 3 days before admission and 3 days after admission, noninvasive mechanical ventilation [NMV], duration of invasive mechanical ventilation [IMV], and continuous renal replace treatment [CRRT]). Referring to the methods of previous studies,11,16 the MDN within 72 h was calculated by dividing the total dosage in 72 h by the actual body weight and the number of minutes of norepinephrine use.
Patients that progressed to experience septic shock were initiated on norepinephrine therapy at a dosage of 0.01 µg/kg/min. Following the 2016 Surviving Sepsis Guidelines,17 the norepinephrine dosage can be titrated up to 35–90 µg/min to increase the MAP above 65 mm Hg. Otherwise, another vasopressor was administrated by the treating team.
A sample from the infected site was collected from each patient within 3 days for bacteriological cultures, such as sputum of deep part or endotracheal intubation internal from patients with a respiratory infection, or ascites collected via abdominal paracentesis from patients with intra-abdominal infection. SOFA was the main score recommended by Sepsis 3.0,8 including respiration, coagulation, liver, renal, cardiovascular, and central nervous system. Each system ranges from 0 (normal) to 4 (the most abnormal). The worst value within 24 h of each system was used for grading. The total score was the sum of the six system scores, ranging from 0 to 24.18 As for mechanical ventilation, the patients that only received NMV via a face mask through treatment procession were classified as NMV and those that received IMV via an endotracheal tube or tracheostomy cannula were classified as IMV regardless of whether they received NMV before and after IMV. The number of cases of NMV and IMV was calculated respectively and the duration of IMV was calculated in hours. Missing data were replaced with the adjacent data.19
The primary outcome indicator was the 28-day mortality, which was described as death occurring at any time from ICU admission to day 28, irrespective of whether the death occurred in ICU, in-hospital, or out of the hospital.20
Statistical Analysis
All statistical analyses were performed using the IBM® SPSS Statistics for Windows, Version 23.0 (IBM Corp., Armonk, NY, USA). The Kolmogorov–Smirnov test was used to analyze whether the variables were by the normal distribution. Continuous normally distributed variables, expressed as mean ± standard deviation (SD), were compared using the Student’s t-test. Continuous variables that were not normally distributed, expressed as the median and interquartile range (IQR), were compared using the nonparametric test. Count variables, reported as numbers and percentages, were compared using the χ2-test or Fisher’s exact test. Correlation coefficients were used to summarize the correlation between the variables. A P-value < 0.05 was considered statistically significant. Pearson’s correlation analysis was conducted if the data were of normal distribution. Spearman correlation analysis was performed if the data were not normally distributed. Kendall’s correlation analysis was used to analyze count variables. The correlation strength was determined according to the r-value, which was expressed as follows: 0.00–0.09, negligible correlation; 0.10–0.39, weak correlation; 0.40–0.69, moderate correlation; 0.70–0.89, strong correlation; and 0.90–1.00, very strong correlation.21 Positive numbers indicated a positive correlation, whereas negative numbers indicated an inverse correlation.
The principal component analysis (PCA) was used to identify the major contributing factors among clinical parameters of the included patients. Based on PCA, the diagnostic efficiency of the screened parameters was computed through the area under the receiver operating characteristic (ROC) curve. The cut-off, sensitivity, and specificity values were established through the ROC curve. The cut-off value was dependent on the Youden index, which is the sum of the sensitivity and specificity minus one. After completing these two steps, the prognostic value for mortality of the remaining meaningful indicators was assessed using the Kaplan–Meier method and multivariate Cox regression analysis.
Results
Baseline and Clinical Data
A total of 169 patients were included during the indicated period, and the flow diagram of case selection was shown in Figure 1. According to the level of FT3, 138 patients were allocated to the low T3 group (FT3 < 3.1 pmol/L) and 31 patients to the normal T3 group (normal FT3). The incidence of LTS was 81.7% (138 of 169 patients). The baseline demographic and clinical characteristics for the two groups were presented in Table 1. The most common infection was a respiratory infection (139 of 169 patients; 82.25%), followed by gastrointestinal and biliary infections (20 of 169 patients; 11.83%). According to the results of ascites culture, the 5 patients with severe acute pancreatitis (2.96%) had infection-related complications. There was a significant difference in the level of FT3 between the two groups (P < 0.001). Among these data, the FT3 values from 4 patients and the PCT values from 3 patients were missing, which were replaced by the nearest values of 3 days before ICU admission.
 |
Table 1 Baseline Characteristics and Clinical Data of the Two Groups |
 |
Figure 1 Flow diagram of case selection. |
As is shown in Table 2, all of the treatment-associated clinical indicators were not statistically different between the two groups. A total of 41 of 169 patients (24.26%) had an Acinetobacter baumannii infection. Of the 169 patients, 82 were diagnosed with septic shock and were treated with vasopressors. Only 16 of 169 patients (9.47%) needed NMV, whereas 111 of 169 patients (65.68%) required IMV. The 28-day mortality was higher in the normal T3 group than in the low T3 group, but the difference was not statistically significant.
 |
Table 2 Comparison of Treatment-Related Clinical Characteristics Between the Two Groups |
Correlation and Prognostic Value of FT3 and MDN
The correlation between FT3, MDN, and other indicators was shown in Table 3. The association between FT3 and MDN was not significant (r=−0.022, P=0.698). The level of FT3 was inversely correlated with SOFA, fluid resuscitation volume, lactic acid levels at the time of ICU admission, and lactic acid levels at the second 24 h; and positively correlated with MAP. However, the r-values for these associations were < 0.39, which implied weak correlations. MDN was positively correlated with SOFA, PCT, HR, the lactic acid levels at the time of ICU admission, and lactic acid levels at the second 24 h; and inversely correlated with survival days and MAP. Except for the moderate correlation between MDN and SOFA, the other correlations were weak.
 |
Table 3 Correlation Analysis of FT3, MDN and the Other Indicators |
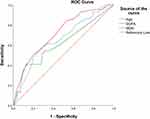
In PCA, the Kaiser–Meyer–Olkin test coefficient was 0.599 and the P-value for Bartlett’s test was < 0.001, which suggested that the principal components could be extracted from the research data. First, five principal components with an Eigenvalue of > 1 were calculated. Secondly, seven original indicators with a load capacity of > 0.7 in the five principal components were selected: age, SOFA, PCT, FT3, lactic acid level at the second 24 h, MDN and CRRT. Thirdly, the ROC curve was constructed for these seven indicators. The results indicated that only age, SOFA, and MDN yielded prognostic values, as shown in Figure 2 and Table 4. Fourthly, the Kaplan–Meier survival analysis was conducted based on specific prognostic risks. For FT3, the difference remained non-significant between the two groups (P = 0.620). Considering the cut-off value of MDN as 0.61 µg/kg/min, all the patients were categorized into either the ≥ 0.61 µg/kg/min group (n = 34) or the < 0.61 µg/kg/min group (n = 135). There was a significant difference in the survival rate between the two groups (P = 0.006). Finally, the multivariate COX regression model analysis, after adjusting for age, SOFA, and FT3, demonstrated that MDN was still a significant independent predictor of mortality (P = 0.006), as shown in Figure 3.
 |
Table 4 The Area Under the Curve and the Cut-Off Value for Diagnosing Death |
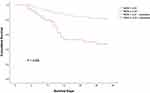 |
Figure 3 Cumulative survival in patients with MDN ≥ 0.61 µg/kg/min (n = 34) and MDN < 0.61 µg/kg/min (n = 135). Abbreviation: MDN, maximum dosage of norepinephrine. |
Discussion
In this retrospective study, we analyzed 169 patients with sepsis and septic shock admitted to ICU. The result showed that FT3 inversely correlated with the SOFA score, fluid resuscitation volume, and lactic acid levels, and positively correlated with the MAP. The mortality of the low T3 and normal T3 groups was similar. MDN ≥ 0.61 µg/kg/min within 72 h may be used as an important index to judge the prognosis of patients with septic shock.
The primary function of FT3 is to regulate body metabolism and facilitate growth and development. The levels of FT3 can be modified in critically ill patients with disease progression, resulting in LTS that is closely related to poor prognosis and long-term mortality.22 In a previous study, 35 of the 114 patients receiving long-term hemodialysis had LTS, an incident rate of 30.7%.23 However, in the present study, 138 of the 169 patients with sepsis and septic shock had LTS, an incident rate of 81.7%. The high incidence of LTS in this current study could be attributed to the following reasons. First, the disease type of patients in this current study was different from those of previous studies, which included patients with chronic kidney disease, acute myocardial infarction, or other disease types.4 The current patients (median age > 70 years) had sepsis and septic shock, most of whom had respiratory system infection. An earlier study, which included 66 patients (mean age 81 years) requiring emergency surgery, indicated that the incidence of LTS was 51.5% (n = 34).24 Secondly, the diagnostic criteria of LTS, which are not currently unified, varied between different studies.25 Few studies considered a cut-off value of 2.772 pmol/L,23 whereas others considered a cut-off value of 3.234 pmol/L.4 In the present study, 3.1 pmol/L of FT3 was considered as the cut-off value.
The incidence of sepsis and septic shock, which are important clinical challenges faced by the critical care medicine team, is on the rise.8 Millions of patients experience sepsis and septic shock every year and more than a quarter of them will die.26,27 Whether the change in the level of FT3 is a prognostic indicator in such patients with LTS remains ambiguous. A previous study demonstrated that the level of FT3 at the initiation of peritoneal dialysis was a strong independent predictor of long-term mortality for cardiovascular disease, especially sudden death.28 In contrast, in the present study, the FT3 level did not demonstrate any correlation with the 28-day mortality, which is in accordance with the results of another study.5 In addition, by analyzing patients with chronic kidney disease having LTS, a study observed that a low level of FT3 was an independent predictor of mortality in a Cox regression analysis and that a low level of FT3 was not a significant predictor of all-cause mortality in a multivariate stepwise Cox regression analysis.23 The differences in the above findings may be due to the different diseases of the study populations. Nevertheless, the current statistical analysis demonstrated that FT3 was correlated with disease severity indicators such as SOFA, MAP, fluid resuscitation volume, and the lactic acid value, although the correlation was weak. This correlation may indicate the possibility of a poor prognosis, although further studies are needed to support this finding.
To normalize and guide the diagnosis and treatment of sepsis, the European Society of Intensive Care Medicine and the Society of Critical Care Medicine published an updated sepsis definition, called Sepsis 3.0, in 2016.8 In this updated version, early goal-directed therapy with norepinephrine as the preferred agent among the vasopressors for the septic shock to maintain the MAP > 65 mm Hg was still recommended.8 However, several studies have indicated that early goal-directed therapy did not improve the prognosis of sepsis.29 Therefore, it is important to know if the norepinephrine dosage is associated with LTS and prognosis in patients with sepsis and septic shock. One previous study, as early as 1998, demonstrated that older patients with LTS, who required emergency surgery, had higher levels of norepinephrine.24 Based on this, we speculate that the decrease of FT3 levels in patients with LTS weakens the vasoconstriction effect of norepinephrine. By injecting T3 into the brachial artery of healthy subjects, a subsequent study showed that FT3 could enhance the vasoconstrictive action of norepinephrine.30 Based on this, we speculate that the decrease of FT3 levels in patients with LTS weakens the vasoconstrictive effect of norepinephrine, resulting in more endogenous norepinephrine. However, the present study found no significant correlation between MDN and FT3. Based on the above results and speculations, we further speculate that the body has a mechanism to regulate the levels of FT3 and norepinephrine, that is, when the FT3 level in patients with LTS decreases, the vasoconstriction of norepinephrine weakens and the body produces more endogenous norepinephrine, resulting in a discretional need for exogenous norepinephrine. The above speculation needs more research to verify.
In this current study, the correlation analysis suggested that MDN was inversely correlated with survival days. Furthermore, the ROC curve and multivariate Cox regression model analyses confirmed that the MDN was an efficient prognostic indicator for mortality in patients with septic shock. This conclusion was in line with the results of a previous study that evaluated 7-day mortality,11 which was different from the 28-day mortality used in the current study. Combining the results of the previous study and this current study,11 it can be concluded that the dosage of norepinephrine is a prognostic indicator of both early and late mortality and should be paid close attention to. Furthermore, another study demonstrated that there was no difference in the 28-day mortality by performing a subgroup analysis with a norepinephrine dosage cut-off of 0.04 µg/kg/min.9 The reason for this difference in results could be because the cut-off value for the subgroup analysis dosage was low. In addition, MDN was positively correlated with SOFA, PCT, HR, lactic acid levels at the time of ICU admission, and lactic acid levels at the second 24 h; and inversely correlated with MAP. This finding indicates that MDN is closely associated with the severity of the disease and can assist in choosing an appropriate clinical treatment.
Sepsis 3.0 emphasizes organ failure and the SOFA score is a relatively accurate scale to reflect the severity of organ failure.31 By categorizing 448 patients with sepsis as a derivation cohort and 199 patients with sepsis as a validation cohort, a study demonstrated that the change of SOFA at day 7 was a useful early prognostic marker of the 28-day mortality.32 A 2019 systematic review included 17 prospective and two retrospective studies.33 The review suggested that PCT might be a promising alternative biomarker for patients with trauma and that the initial peak in PCT can serve as an early predictor of sepsis, multi-organ failure, and mortality in the trauma population.33 In view of the importance of SOFA and PCT in predicting the prognosis of sepsis and septic shock,34,35 they were emphasized in the present research study. Through correlation analysis, the current study found that FT3 was inversely correlated with SOFA within the first 24 h and that MDN was positively correlated with SOFA and PCT within the first 24 h. These findings can provide an important reference to evaluate the clinical prognosis of patients with sepsis and septic shock and assist in choosing the correct norepinephrine dosage in clinical settings. Moreover, in the present study, the area under the ROC curve of SOFA within the first 24 h was 0.715, which was slightly higher than that in one study and slightly lower than that in another study.36,37
Limitations
This study had several limitations. First, although the diagnostic efficiency of the three indicators (age, SOFA, and MDN) attained statistical significance, the sensitivity and specificity were not adequately high, which could be attributed to the small sample size, especially as there were only 31 patients in the normal T3 group. Secondly, among the 169 patients, 138 patients were allocated to the low T3 group, accounting for 81.7%, which is the inherent selection bias of the retrospective study. Thirdly, in this study, the MDN was calculated regarding the methods of literature,11,16 but other vasopressors dosages were not converted to the norepinephrine equivalent dosage, which was one of the limitations of this study and needs to be applied in future studies. Consequently, since this study is a retrospective study, further, larger prospective studies with more study participants are required to explore the correlation between LTS and norepinephrine dosage.
Conclusions
This current study demonstrated a relationship between FT3, MDN, and the disease severity indices, such as the SOFA score, PCT, and lactate level. These findings suggest that FT3 and MDN may be considered as indices of the severity of the disease. Importantly, MDN ≥ 0.61 µg/kg/min within 72 h may be used as an important index to judge the prognosis of patients with septic shock.
Abbreviations
T3, triiodothyronine; LTS, Low triiodothyronine syndrome; FT3, free T3; TSH, thyroid-stimulating hormone; ICU, intensive care unit; MAP, mean arterial pressure; SOFA, Sequential Organ Failure Assessment; FT4, free T4; HR, heart rate; RR, respiratory rate; PCT, procalcitonin; MDN, maximum dosage of norepinephrine; NMV, noninvasive mechanical ventilation; IMV, invasive mechanical ventilation; CRRT, continuous renal replace treatment; SD, standard deviation; IQR, interquartile range; PCA, principal component analysis; ROC, receiver operating characteristic; Lac, lactic acid.
Data Sharing Statement
The data sets used and analyzed in the current study are available from the corresponding authors upon reasonable request.
Ethics Approval and Informed Consent
This study was performed in accordance with the principles of the Declaration of Helsinki and was approved by the Ethics Committee of the First Hospital of Nanchang (number: ZKY2019002; date: December 2, 2019). Considering the retrospective design of this study and the de-identified disposition for information of patients, patient consent was waived. The identity information of all included patients was anonymized so that the identity of patients could not be determined in any way.
Funding
This research received a grant from the National Natural Science Foundation of China (No. 81560306), Key Research and Development Plan Projects of Jiangxi Science and Technology Department (No. 20161BBG70173), Science and Technology Program of Health and Family Planning Commission of Jiangxi, China (No. 20184003, 20204033), and Science and Technology Program of the First Hospital of Nanchang, Jiangxi, China (No. 2017L006).
Disclosure
The authors declare that there is no conflict of interest in this work.
References
1. Van den Berghe G. Non-thyroidal illness in the ICU: a syndrome with different faces. Thyroid. 2014;24(10):1456–1465. doi:10.1089/thy.2014.0201
2. Boelen A, Boorsma J, Kwakkel J, et al. Type 3 deiodinase is highly expressed in infiltrating neutrophilic granulocytes in response to acute bacterial infection. Thyroid. 2008;18(10):1095–1103. doi:10.1089/thy.2008.0090
3. Bunevicius A, Deltuva V, Tamasauskas S, Tamasauskas A, Laws EJ, Bunevicius R. Low triiodothyronine syndrome as a predictor of poor outcomes in patients undergoing brain tumor surgery: a pilot study: clinical article. J Neurosurg. 2013;118(6):1279–1287. doi:10.3171/2013.1.JNS121696
4. Su W, Zhao X, Wang M, Chen H, Low LH. T3 syndrome improves risk prediction of in-hospital cardiovascular death in patients with acute myocardial infarction. J Cardiol. 2018;72(3):215–219. doi:10.1016/j.jjcc.2018.02.013
5. Meyer S, Schuetz P, Wieland M, Nusbaumer C, Mueller B, Christ-Crain M. Low triiodothyronine syndrome: a prognostic marker for outcome in sepsis? Endocrine. 2011;39(2):167–174. doi:10.1007/s12020-010-9431-4
6. Maiden MJ, Torpy DJ. Thyroid hormones in critical illness. Crit Care Clin. 2019;35(2):375–388. doi:10.1016/j.ccc.2018.11.012
7. Bertoli A, Valentini A, Cianfarani MA, Gasbarra E, Tarantino U, Federici M. Low FT3: a possible marker of frailty in the elderly. Clin Interv Aging. 2017;12:335–341. doi:10.2147/CIA.S125934
8. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–810. doi:10.1001/jama.2016.0287
9. Yamamura H, Kawazoe Y, Miyamoto K, Yamamoto T, Ohta Y, Morimoto T. Effect of norepinephrine dosage on mortality in patients with septic shock. J Intensive Care. 2018;6:12. doi:10.1186/s40560-018-0280-1
10. Hammond DA, Ficek OA, Painter JT, et al. Prospective open-label trial of early concomitant vasopressin and norepinephrine therapy versus initial norepinephrine monotherapy in septic shock. Pharmacotherapy. 2018;38(5):531–538. doi:10.1002/phar.2105
11. Kasugai D, Hirakawa A, Ozaki M, et al. Maximum norepinephrine dosage within 24 hours as an indicator of refractory septic shock: a Retrospective Study. J Intensive Care Med. 2019;35:1585793280.
12. Fontes KN, Cabanelas A, Bloise FF, et al. Differential regulation of thyroid hormone metabolism target genes during non-thyroidal illness syndrome triggered by fasting or sepsis in adult mice. Front Physiol. 2017;8:828. doi:10.3389/fphys.2017.00828
13. Gao R, Liang J-H, Wang L. Low T3 syndrome is a strong prognostic predictor in diffuse large B cell lymphoma. Brit J Haematol. 2017;177(1):95–105. doi:10.1111/bjh.14528
14. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8
15. Vincent JL, Moreno R, Takala J, The AE. SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European Society of intensive care medicine. Intensive Care Med. 1996;7(22):707–710. doi:10.1007/BF01709751
16. Singer KE, Sussman JE, Kodali RA, et al. Hitting the vasopressor ceiling: finding norepinephrine associated mortality in the critically Ill. J Surg Res. 2021;265:139–146. doi:10.1016/j.jss.2021.03.042
17. Dellinger RP, Schorr CA, Levy MM. A users’ guide to the 2016 surviving sepsis guidelines. Intensive Care Med. 2017;43(3):299–303. doi:10.1007/s00134-017-4681-8
18. Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286(14):1754–1758. doi:10.1001/jama.286.14.1754
19. Pedersen AB, Mikkelsen EM, Cronin-Fenton D, et al. Missing data and multiple imputation in clinical epidemiological research. Clin Epidemiol. 2017;9:157–166. doi:10.2147/CLEP.S129785
20. Brouwer WP, Duran S, Kuijper M, Ince C. Hemoadsorption with CytoSorb shows a decreased observed versus expected 28-day all-cause mortality in ICU patients with septic shock: a propensity-score-weighted retrospective study. Crit Care. 2019;23(1):317. doi:10.1186/s13054-019-2588-1
21. Schober P, Boer C, Schwarte LA. Correlation coefficients: appropriate use and interpretation. Anesth Analg. 2018;126(5):1763–1768. doi:10.1213/ANE.0000000000002864
22. Luo B, Yu Z, Li Y. Thyroid hormone disorders and sepsis. Biomed Mater Eng. 2017;28(s1):S237–S241. doi:10.3233/BME-171646
23. Fragidis S, Sombolos K, Thodis E, et al. Low T3 syndrome and long-term mortality in chronic hemodialysis patients. World J Nephrol. 2015;4(3):415–422. doi:10.5527/wjn.v4.i3.415
24. Girvent M, Maestro S, Hernandez R, et al. Euthyroid sick syndrome, associated endocrine abnormalities, and outcome in elderly patients undergoing emergency operation. Surgery. 1998;123(5):560–567. doi:10.1067/msy.1998.87238
25. Fliers E, Boelen A. An update on non-thyroidal illness syndrome. J Endocrinol Invest. 2021;44(8):1597–1607. doi:10.1007/s40618-020-01482-4
26. Kaukonen KM, Bailey M, Suzuki S, Pilcher D, Bellomo R. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000–2012. JAMA. 2014;311(13):1308–1316. doi:10.1001/jama.2014.2637
27. Meghraoui-Kheddar A, Chousterman BG, Guillou N, et al. Two new neutrophil subsets define a discriminating sepsis signature. Am J Respir Crit Care Med. 2022;205(1):46–59. doi:10.1164/rccm.202104-1027OC
28. Chang TI, Nam JY, Shin SK, Kang EW. Low triiodothyronine syndrome and long-term cardiovascular outcome in incident peritoneal dialysis patients. Clin J Am Soc Nephrol. 2015;10(6):975–982. doi:10.2215/CJN.03350414
29. Zhang L, Zhu G, Han L, Fu P. Early goal-directed therapy in the management of severe sepsis or septic shock in adults: a meta-analysis of randomized controlled trials. BMC Med. 2015;13:71. doi:10.1186/s12916-015-0312-9
30. Napoli R, Guardasole V, Angelini V, et al. Acute effects of triiodothyronine on endothelial function in human subjects. J Clin Endocrinol Metab. 2007;92(1):250–254. doi:10.1210/jc.2006-1552
31. Seymour CW, Liu VX, Iwashyna TJ, et al. Assessment of clinical criteria for sepsis: for the third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):762–774. doi:10.1001/jama.2016.0288
32. Karakike E, Kyriazopoulou E, Tsangaris I, Routsi C, Vincent JL, Giamarellos-Bourboulis EJ. The early change of SOFA score as a prognostic marker of 28-day sepsis mortality: analysis through a derivation and a validation cohort. Crit Care. 2019;23(1):387. doi:10.1186/s13054-019-2665-5
33. AlRawahi AN, AlHinai FA, Doig CJ, et al. The prognostic value of serum procalcitonin measurements in critically injured patients: a systematic review. Crit Care. 2019;23(1):390. doi:10.1186/s13054-019-2669-1
34. Wen K, Du H, Tang B, Xiong B, Zhang A, Wang P. Complete blood count and myocardial markers combination with sequential organ failure assessment score can effectively predict the mortality in sepsis: a Derivation and Validation Study. Int J Gen Med. 2022;15:3265–3280. doi:10.2147/IJGM.S349751
35. Li Y, Wang J, Wei B, Zhang X, Hu L, Ye X. Value of neutrophil: lymphocyte ratio combined with sequential organ failure assessment score in assessing the prognosis of sepsis patients. Int J Gen Med. 2022;15:1901–1908. doi:10.2147/IJGM.S348200
36. Liu Z, Meng Z, Li Y, et al. Prognostic accuracy of the serum lactate level, the SOFA score and the qSOFA score for mortality among adults with Sepsis. Scand J Trauma Resusc Emerg Med. 2019;27(1):51. doi:10.1186/s13049-019-0609-3
37. Zhang Y, Khalid S, Jiang L. Diagnostic and predictive performance of biomarkers in patients with sepsis in an intensive care unit. J Int Med Res. 2019;47(1):44–58. doi:10.1177/0300060518793791
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.