Back to Journals » Journal of Pain Research » Volume 15
Correlation Analysis of the Characteristics of Spino-Pelvic Parameters and Health-Related Quality of Life After Long-Segment Fixation for Lenke–Silva Type 5 or 6 Degenerative Scoliosis
Authors Hu W, Song Y, Ma H, Wang H , Zhang K, Gao Y
Received 30 March 2022
Accepted for publication 27 July 2022
Published 2 August 2022 Volume 2022:15 Pages 2171—2179
DOI https://doi.org/10.2147/JPR.S368142
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Krishnan Chakravarthy
Weiran Hu,1,2,* Yuepeng Song,1,3,* Haohao Ma,1,2 Hongqiang Wang,1,2 Kai Zhang,1,2 Yanzheng Gao1,2
1Department of Spinal Cord Surgery, Henan Provincial People’s Hospital, Zhengzhou, Henan, People’s Republic of China; 2Department of Spinal Cord Surgery, People’s Hospital of Zhengzhou University, Zhengzhou, Henan, People’s Republic of China; 3Department of Spinal Cord Surgery, People’s Hospital of Henan University, Zhengzhou, Henan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yanzheng Gao, Department of Spinal Cord Surgery, Henan Provincial People’s Hospital, No. 7 Wei Wu Road, Zhengzhou, 450003, People’s Republic of China, Email [email protected]
Purpose: To retrospectively evaluate the characteristics of spino-pelvic parameters after long-segment fixation in patients with Lenke–Silva type 5 or 6 adult degenerative scoliosis and analyze the correlation between spino-pelvic parameters and health-related quality of life (HRQL).
Methods: Thirty-two patients with degenerative scoliosis underwent long-segment posterior fixation were included. The spino-pelvic parameters were evaluated after surgery, and the HRQL scores were determined using the Scoliosis Research Society-22 (SRS-22), Oswestry Disability Index (ODI), and visual analog scale (VAS). Linear regression was used to analyze the correlation between changes in spino-pelvic parameters and improvements in HRQL.
Results: Except for PI and TK, the other parameters showed significant differences after surgery (P < 0.05). All the scores of HRQL showed significant differences after surgery. The coefficient of correlation between ΔSVA and ΔVAS is 0.687 (P = 0.003), the coefficient of correlation between ΔSVA and ΔODI is 5.828 (P < 0.001). The coefficient of correlation between ΔLL and ΔVAS is − 0.089 (P < 0.001), the coefficient of correlation between ΔLL and ΔODI is − 1.553 (P = 0.003). The VAS score between the SVA ≥ 4cm and SVA < 4cm group have no significant difference, but have a significant difference in ODI. In PI-LL ≥ 20°and PI-LL < 20°group, the VAS and ODI all have a significant difference between the two groups.
Conclusion: SVA and LL have an important role in maintaining the overall balance of the spine and closely related to the postoperative HRQL, better HRQL may be achieved by reducing SVA and increasing LL. Good preoperative design will help achieve the best clinical efficacy.
Keywords: degenerative scoliosis, spino-pelvic parameters, long-segment fixation, health-related quality of life
Introduction
Adult degenerative scoliosis (ADS) is characterized by an abnormal spine curvature of >10° after skeletal maturity that is generally not observed in children and adolescents.1 ADS is common in individuals over 40 years. With the increase in the aging population, the incidence of ADS has also been gradually increasing, making ADS an important public health problem. In patients older than 40 years, the incidence of ADS increases with age (6–68%).2 Previous studies have focused on the etiology, patient statistics, clinical features, imaging findings, and treatment methods of ADS. Recent studies have suggested that sagittal imbalance, coronal changes, and vertebral rotation in ADS have a great impact on patients’ health-related quality of life (HRQL).3–6
The treatment strategies for ADS include simple decompression and post-decompression fixation fusion, which involves short-segment and long-segment. Short-segment fixation and fusion cannot prevent further scoliosis and postoperative complications such as scoliosis progression and proximal segment degeneration, whereas long-segment fixation and fusion ensures complete decompression while restoring spinal stability to prevent further scoliosis development. The advantages of long-segment fixation and fusion have gradually emerged, especially in patients with Lenke–Silva type 5 or 6.7 Long-segment fixation improves the overall balance of the spine and reduces the incidence of postoperative complications.7 In a recent study comparing long-segment with short-segment, Zhang et al8 suggested that long-segment is superior in terms of correction and restoration of sagittal balance. Kasten et al9 followed up 78 patients for 2 years and found that long-segment posterior fixation corrected scoliosis from an average curvature of 61° before surgery to an average curvature of 29° after surgery and achieved good lumbosacral fusion through posterior spino-pelvic fixation, thereby reducing the incidence of postoperative pseudarthrosis. Further, Schroeder et al10 found that the visual analog scale (VAS) scores decreased from 6.5 to 2.0 for lower extremity pain and from 7.83 to 2.67 for low back pain after long-segment surgery, at the same time Oswestry Disability Index (ODI) decreased from 22.2 to 10.5.
Previous studies have focused on the advantages and disadvantages of long-segment fixation versus short-segment fixation and on the improvement in postoperative pain and function. To the best of our knowledge, the characteristics of postoperative spino-pelvic parameters and the correlation between the improvement in these spino-pelvic parameters and the HRQL scores have not been investigated to date, and whether these parameters are as closely related to HRQL remains to be verified. Therefore, our study aimed to analyze the characteristics of spino-pelvic parameters and their correlation with the HRQL scores after long-segment fixation to develop a more reasonable surgical correction strategy.
Methods
Data
This study conducted a retrospective analysis of patients with degenerative scoliosis who were admitted to our hospital between March 2013 and May 2018. All the patients underwent long-segment posterior spinal fixation. (a typical case is shown in Figure 1). This study has been reviewed and approved by the Ethics Committee of Henan Provincial People’s Hospital, and all the included patients have signed the consent form.
Inclusion and Exclusion Criteria
Inclusion criteria were as follows: (1) age >60 years; (2) ADS is classified as Lenke–Silva type 5 or 6;7 (3) fusion/fixation for three or more segments; (4) available standing full-length X-ray images of the spine; (5) available Scoliosis Research Society-22 (SRS-22) score, ODI, and VAS scores; (6) the operation was successful and no complications occurred. Exclusion criteria were as follows: (1) spinal surgery history; (2) neurodegenerative diseases; (3) other serious systemic diseases.
HRQL Score Evaluation
All patients completed the SRS-22 questionnaire in a quiet environment. The SRS-22 questionnaire comprises 22 questions and is divided into five domains: function, pain, self-perceived image, mental health, and satisfaction with treatment. Each question is scored on a scale of 1–5, 1 is the worst score and 5 is the best score. The score for each domain is the sum of the scores of the corresponding questions, and the total score in the SRS-22 questionnaire is the sum of scores for all questions. Simultaneously, ODI and the VAS scale were used to evaluate the patients’ HRQL.
Imaging Parameter Evaluation
Preoperative and postoperative imaging indicators were evaluated using the Picture Archiving and Communication System (PACS), including sagittal vertical axis (SVA); thoracic kyphosis (TK), Cobb’s angle for T4–T12; lumbar lordosis (LL), Cobb’s angle between the upper L1 endplate and upper S1 endplate; sacral slope (SS), angle between the endplate on S1 and the horizontal line; pelvic incidence (PI), angle from the midpoint of the bilateral femoral head central line to the center of the upper S1 endplate and the double perpendicular line. All imaging indicators were independently measured by two physicians and then averaged for analysis (Figure 2).
At the same time, the Cobb angle and trunk shift was also included in this study. Cobb angle: the angle between the cervix and caudal vertebral body with maximum oblique angle in the posterior and anterior full spine X-rays. Trunk shift: the distance between C7 plumb line (C7PL) and center sacral vertical line (CSVL). All imaging indicators were independently measured by two physicians and then averaged for analysis.
Statistical Analysis
SPSS version 20.0 (IBM Corp, Armonk, New York, USA) was used for statistical analysis. All values are presented as mean ± standard deviation. Comparisons of means between variables were performed using independent Student’s t-test. Linear regression was used to analyze the correlation between postoperative changes in spino-pelvic parameters and improvements in HRQL. The significance level for all statistical tests was set as P<0.05.
Results
A total of 32 patients with degenerative scoliosis treated at our hospital from March 2013 to May 2018 were analyzed retrospectively, these patient cohort comprised 10 men and 22 women aged 60.2–73.4 years (average age 64.0 ± 3.5 years). The fixed fusion segments were 7.2 ± 1.9 and the decompression segments was 3.1 ± 1.7. The estimated blood loss (EBV) was 1236.5 ± 461.7cc (%EBV is 17.1 ± 4.6cc/kg), and the operation time was 230.5 ± 34.1 mins (Table 1).
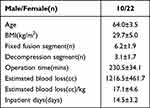 |
Table 1 The General Information of the Patient |
The characteristics of the preoperative and postoperative imaging parameters are summarized in Table 2. Except for PI, TK and trunk shift, the other parameters showed significant differences after surgery (P<0.05).With SVA have a change of −4.4 ± 1.4 cm, LL have a change of 9.4 ± 4.7°, PT have a change of −11.7 ± 5.3°, SS have a change of 13.2 ± 3.7°, the Cobb angle corrected from 36.7 ± 12.1 to 10.2 ± 5.7°.
 |
Table 2 Changes of Imaging Parameters Before and After Surgery |
Four parts of SRS-22 score changed except for the part of satisfaction with management, the function score changed from 12.5 ± 2.1 to 21.6 ± 7.1, the pain score changed from 14.2 ± 6.0 to 19.4 ± 3.7, the self-image score changed from 13.7 ± 3.1 to 22.1 ± 5.6, the mental health score changed from 16.3 ± 4.7 to 21.6 ± 8.2 (Table 3). All the scores showed significant differences after surgery. And the ODI have a change of −46.2 ± 4.2, the VAS have a change of −3.9 ± 2.6. The ODI and VAS have a significant differences before and after surgery (Table 4).
 |
Table 3 Preoperative and Postoperative SRS-22 Score |
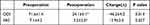 |
Table 4 Preoperative and Postoperative VAS and ODI Score |
The linear correlation between postoperative changes in spino-pelvic parameters and improvements in HRQL was made. The ΔSVA and ΔLL have a significant correlation with ΔVAS andΔODI. The coefficient of correlation between ΔSVA and ΔVAS is 0.687 (P=0.003), the coefficient of correlation between ΔSVA and ΔODI is 5.828 (P<0.001) (Figure 3A and B). This means that the smaller the SVA, the more significant the HRQL improvement. The coefficient of correlation between ΔLL and ΔVAS is −0.089 (P<0.001), the coefficient of correlation between ΔLL and ΔODI is −1.553 (P=0.003) (Figure 3C and D). This means that the larger the LL, the more significant the HRQL improvement (Table 5). And the coefficient of correlation between ΔCobb angle and ΔVAS is 0.312 (P>0.05), the coefficient of correlation between ΔCobb angle and ΔODI is 4.362 (P>0.05), the coronal balance is not an important factor affecting HRQL.
 |
Table 5 Correlation Between Postoperative Changes in Imaging Parameters and Improvements in HRQL |
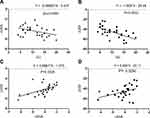 |
Figure 3 (A) correlation between ΔLL and ΔVAS. (B) correlation between ΔLL and ΔODI. (C) correlation between ΔSVA and ΔVAS. (D) correlation between ΔSVA and ΔODI. |
To further verify the above results, the patients were divided in SVA ≥ 4cm and SVA < 4cm group according to postoperative spino-pelvic parameters. The VAS score between the two groups have no significant difference, but have a significant difference in ODI (Figure 4A). Then the patients were divided in PI-LL≥20°and PI-LL<20°group, and the VAS and ODI all have a significant difference between the two groups (Figure 4B). Which means improving SVA and LL will benefit to obtain better postoperative HRQL.
 |
Figure 4 (A) the VAS and ODI in SVA≥4cm and SVA < 4cm group(*P<0.05). (B) the VAS and ODI in PI-LL≥20°and PI-LL<20°group (*P<0.05). |
Discussion
ADS is a spinal deformity caused by degeneration of intervertebral discs and facet joints, it is often accompanied by rotation and lateral displacement of the vertebral body. ADS is generally accompanied by an increase in Cobb angle as well as by changes in spino-pelvic parameters. Previous studies have shown that the symptoms of degenerative scoliosis are strongly correlated with the sagittal plane balance in patients.6 Spino-pelvic parameters are critical for maintaining spinal biomechanical stability. Spinal and pelvic sequences affect each other, making the human body relatively stable with minimum energy consumption and reducing the impact on and concussion of the spine and spinal cord.3 Therefore, spino-pelvic parameters are closely related to HRQL, and the correlation between spino-pelvic parameters and HRQL can guide the improvement of orthopedic strategies.
Previous studies have found that the risk of scoliosis increases greatly when the coronal Cobb angle is >30°, often requiring surgical treatment. Recently, it has been suggested that short-segment fixation for degenerative scoliosis must be limited to the following conditions: spinal stenosis of no more than three segments, scoliosis with a Cobb’s angle of <30°, no sagittal or coronal imbalance, and no significant progression of scoliosis.11 For patients with a Cobb angle of >30° and with sagittal imbalance, Lenke et al proposed long-segment posterior spinal fixation.7 The Lenke–Silva classification for ADS suggests that patients with type 5 or 6 ADS should undergo long-segment posterior spinal fixation with osteotomy.7
In our study, postoperative changes in SVA and improvements in HRQL is closely related, the coefficient of correlation between ΔSVA and ΔVAS is 0.687, the coefficient of correlation between ΔSVA and ΔODI is 5.828 which means that the smaller the SVA, the more significant the HRQL improvement. Previous studies have shown that SVA is an important parameter for sagittal balance, and SVA of >5 cm indicates sagittal imbalance. In the results of subgroup analysis, we found that SVA < 4cm group may have a better HRQL scores, which has come to the similar conclusions with other studies. Takemoto et al12 found that SVA was closely related to the postoperative HRQL scores evaluated using multiple linear regression analysis for the spino-pelvic parameters and HRQL. Similarly, Ogura et al13 found that SVA was negatively correlated with postoperative efficacy and HRQL scores and that the HRQL scores with SVA>50 mm was significantly lower than that with SVA<50 mm.
We found that LL was closely related to HRQL, and appropriate LL can help in improving lumbar mobility and reducing lower back pain. The coefficient of correlation between ΔLL and ΔVAS is −0.089, the coefficient of correlation between ΔLL and ΔODI is −1.553. Theoretically, a decrease in LL will stretch the lumbar paravertebral muscles and require muscular strengthening to maintain the stability of the spine, which will more likely cause muscle overstrain, decrease the muscle support function, and aggravate spinal degeneration. Based on evaluation of healthy asymptomatic adults, Schwab et al simplified the relationship between LL and PI as follows: LL = PI ± 9°. As PI is a constant anatomic parameter, theoretical LL can be deduced by using PI, which has guiding significance for the correction of LL angle. Yang et al14 retrospectively analyzed 56 ASD patients with long-segment posterior spinal fixation and concluded that restoration of LL greatly improved the HRQL. Simon et al15 concluded that LL was closely associated with the 36-Item Short Form Survey scores after a 6-year follow-up analysis and proposed that the correction of sagittal balance by can achieve long-term clinical efficacy.
Many studies have demonstrated that pelvic parameters have an important role in maintaining the overall balance of the spine. In patients with scoliosis, posterior rotation of the pelvis is often used to compensate for the sagittal imbalance. This compensatory mechanism plays an important role in maintaining the patient’s center of gravity above the femoral head and in maintaining the patient’s upright position. Although no correlation with HRQL was found, many studies still conducted that pelvic parameters may influence the sagittal sequence of the spine. Protopsaltis et al16 conducted that decompensation occurs when the posterior rotation of the pelvis leads to lower back pain and discomfort. PI is equal to the sum of PT and SS, and LL can be dynamically adjusted by adjusting PT. Zhang et al17 concluded that the occurrence probability of degenerative scoliosis increased by 1.465 times with a 0.1 increase in PT/SS. All these factors would eventually increase the incidence of scoliosis with the increase in PT. Sabou et al18 proposed that preoperative PT and age were closely related to the postoperative clinical efficacy and that younger patients and patients with a smaller PT were more likely to achieve clinical satisfaction. Eguchi et al19 concluded that a deceased PT leads to the progression of scoliosis and increases back pain scores.
PI-LL is a new index proposed by Schwab to evaluate the sagittal balance of the spine. Previous studies have suggested that the spine and pelvic sequences are not coordinated when the PI-LL is >9°, which is the basis of spinal imbalance and degeneration. However, recent studies suggest that a smaller LL is more consistent with the changes in the physiological curvature of the spine, and some studies indicate that patients with scoliosis can obtain more satisfactory clinical efficacy when the PI-LL is 20°.5 We subdivide the patients into PI-LL ≥ 20°and PI-LL < 20°group, and found that the patients with PI-LL ≥ 20°achieved better clinical outcomes. This may be related to the fact that after long-segment fixation, the overall center of gravity of patients with PI-LL ≥ 20°moved forward, which is more conducive to bending and other activities in daily life.
Many studies have confirmed our conclusion, in a retrospective study conducted by Zhang et al.20 PI-LL was divided into three groups: PI-LL <10°, PI-LL >20°, and 10° < PI-LL < 20°. The analysis of postoperative Japanese orthopedic association score, VAS score, and ODI showed that the 10° < PI-LL < 20° group had the best quality of life. At the same time, a previous study indicated that maintaining a PI-LL with the range of 10° to 20° can achieve the best clinical efficacy and can effectively prevent the occurrence of proximal borderline scoliosis.21 Ky et al3 used the SRS-Schwab classification system and found that among all parameters, PI-LL was most closely related to postoperative clinical efficacy. Sun et al4 reviewed ADS patients after long-segment fixation and found that patients with PI-LL of 10° to 20° had better clinical efficacy and a lower incidence of proximal junctional kyphosis.
At the same time, we found that coronal balance was not an important factor affecting HRQL. On the one hand, the coronal imbalance of ADS is generally not serious and can be well corrected by surgery, on the other hand, spino-pelvic parameters affect the daily activities of patients through force line changes. In patients with degenerative scoliosis, degeneration of the discs and facet joints can lead to spinal stenosis. Therefore, good clinical efficacy can be achieved by sagittal balance restoration and precision decompression in the treatment of degenerative scoliosis.
Conclusion
In our study, SVA and LL have an important role in maintaining the overall balance of the spine and closely related to the postoperative HRQL, better HRQL may be achieved by reducing SVA and increasing LL. Good preoperative design will help achieve the best postoperative clinical efficacy. This study has some limitations, including the limited number of patients and the lack of further discussion on fixed segment positions, the distal and proximal fixed vertebrae, the osteotomy position, and the osteotomy method. Further studies on the influence of various factors on the postoperative HRQL in patients with ADS are needed.
Data Sharing Statement
All data are described in the manuscript. The datasets used and/or analyzed in the present study are available from the corresponding author upon reasonable request.
Ethics Approval
This study complies with the Declaration of Helsinki, and was approved by the Ethics Committee of Henan Provincial People’s Hospital.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Henan Provincial Medical Science and Technology Tackling Program Joint Project (LHGJ20200047), the Henan Provincial Medical Science and Technology Tackling Program Provincial-Ministerial Co-construction Project (SB201901085), and the Henan Provincial Medical Science and Technology Tackling Program Provincial-Ministerial Co-construction Project (SBGJ2018076).
Disclosure
The authors have no conflicts of interest to declare that are relevant to the content of this manuscript.
References
1. Du JP, Fan Y, Liu JJ, et al. Application of gelatin sponge impregnated with a mixture of 3 drugs to intraoperative nerve root block combined with robot-assisted minimally invasive transforaminal lumbar interbody fusion surgery in the treatment of adult degenerative scoliosis: a clinical observation including 96 patients. World Neurosurg. 2017;108:791–797. doi:10.1016/j.wneu.2017.09.075
2. Uddin OM, Haque R, Sugrue PA, et al. Cost minimization in treatment of adult degenerative scoliosis. J Neurosurg Spine. 2015;23:798–806. doi:10.3171/2015.3.SPINE14560
3. Sun XY, Zhang XN, Hai Y. Optimum pelvic incidence minus lumbar lordosis value after operation for patients with adult degenerative scoliosis. Spine J. 2017;17:983–989. doi:10.1016/j.spinee.2017.03.008
4. Yagi M, Kaneko S, Yato Y, et al. Standing balance and compensatory mechanisms in patients with adult spinal deformity. Spine. 2017;42:E584–E591. doi:10.1097/BRS.0000000000001901
5. Chen RQ, Hosogane N, Watanabe K, et al. Reliability analysis of spino-pelvic parameters in adult spinal deformity: a comparison of whole spine and pelvic radiographs. Spine. 2016;41:320–327. doi:10.1097/BRS.0000000000001208
6. Hayden AM, Hayes AM, Brechbuhler JL, et al. The effect of pelvic motion on spinopelvic parameters. Spine J. 2018;18:173–178. doi:10.1016/j.spinee.2017.08.234
7. Silva FE, Lenke LG. Adult degenerative scoliosis: evaluation and management. Neurosurg Focus. 2010;28:E1. doi:10.3171/2010.1.FOCUS09271
8. Zhang HC, Yu HL, Yang HF, et al. Short-segment decompression/fusion versus long-segment decompression/fusion and osteotomy for Lenke-Silva type VI adult degenerative scoliosis. Chin Med J. 2019;132:2543–2549. doi:10.1097/CM9.0000000000000474
9. Kasten MD, Rao LA, Priest B. Long-term results of iliac wing fixation below extensive fusions in ambulatory adult patients with spinal disorders. J Spinal Disord Tech. 2010;23:e37–e42. doi:10.1097/BSD.0b013e3181cc8e7f
10. Schroeder JE, Cunningham ME, Ross T, et al. Early results of sacroiliac joint fixation following long fusion to the sacrum in adult spine deformity. HSS J. 2014;10:30–35. doi:10.1007/s11420-013-9374-4
11. Chen PG, Daubs MD, Berven S, et al.; Degenerative Lumbar Scoliosis Appropriateness Group. Surgery for degenerative lumbar scoliosis: the development of appropriateness criteria. Spine. 2016;41:910–918. doi:10.1097/BRS.0000000000001392
12. Takemoto M, Boissiere L, Vital JM, et al. Are sagittal spinopelvic radiographic parameters significantly associated with quality of life of adult spinal deformity patients? Multivariate linear regression analyses for pre-operative and short-term post-operative health-related quality of life. Eur Spine J. 2017;26:2176–2186. doi:10.1007/s00586-016-4872-y
13. Ogura Y, Shinozaki Y, Kobayashi Y, et al. Impact of sagittal spinopelvic alignment on clinical outcomes and health-related quality of life after decompression surgery without fusion for lumbar spinal stenosis. J Neurosurg Spine. 2019;30:470–475. doi:10.3171/2018.10.SPINE181094
14. Schwab F, Ungar B, Blondel B, et al. Scoliosis Research Society—Schwab adult spinal deformity classification: a validation study. Spine. 2012;37:1077–1082. doi:10.1097/BRS.0b013e31823e15e2
15. Yang Y, Zheng J, Lou S. Medium to long-term curative effects of long-segmental fixation and fusion on degenerative scoliosis. Int J Clin Exp Med. 2015;8:8129–8134.
16. Simon J, Longis PM, Passuti N. Correlation between radiographic parameters and functional scores in degenerative lumbar and thoracolumbar scoliosis. Orthop Traumatol Surg Res. 2017;103:285–290. doi:10.1016/j.otsr.2016.10.021
17. Protopsaltis T, Schwab F, Bronsard N, et al. The T1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Joint Surg Am. 2014;96:1631–1640. doi:10.2106/JBJS.M.01459
18. Zhang J, Hai Y, Yang J, et al. Increased PT/SS may play an important role in the pathogenesis of lumbar spondylolisthesis with degenerative lumbar scoliosis. Clin Neurol Neurosurg. 2018;166:23–30. doi:10.1016/j.clineuro.2018.01.018
19. Sabou S, Tseng TH, Stephenson J, et al. Correction of sagittal plane deformity and predictive factors for a favourable radiological outcome following multilevel posterior lumbar interbody fusion for mild degenerative scoliosis. Eur Spine J. 2016;25:2520–2526. doi:10.1007/s00586-015-4338-7
20. Eguchi Y, Norimoto M, Suzuki M, et al. Diffusion tensor tractography of the lumbar nerves before a direct lateral transpsoas approach to treat degenerative lumbar scoliosis. J Neurosurg Spine. 2019;30:461–469. doi:10.3171/2018.9.SPINE18834
21. Zhang HC, Zhang ZF, Wang ZH, et al. Optimal pelvic incidence minus lumbar lordosis mismatch after long posterior instrumentation and fusion for adult degenerative scoliosis. Orthop Surg. 2017;9:304–310. doi:10.1111/os.12343
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


