Back to Journals » Vascular Health and Risk Management » Volume 10
Coronary microvascular endothelial dysfunction is an independent predictor of development of osteoporosis in postmenopausal women
Authors Prasad M, Reriani M, Khosla S, Gössl M, Lennon R, Gulati R, Prasad A, Lerman L , Lerman A
Received 5 March 2014
Accepted for publication 3 April 2014
Published 26 August 2014 Volume 2014:10 Pages 533—538
DOI https://doi.org/10.2147/VHRM.S63580
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Megha Prasad, Martin Reriani, Sundeep Khosla, Mario Gössl, Ryan Lennon, Rajiv Gulati, Abhiram Prasad, Lilach O Lerman, Amir Lerman
Division of Cardiovascular Diseases, Mayo Clinic, Rochester, MN, USA
Background: A growing body of evidence links coronary artery atherosclerosis and calcification to osteoporosis in women. The endothelium plays a critical role in maintaining vascular integrity and may play a role in bone metabolism. We aimed to determine whether early coronary atherosclerosis, as detected by coronary microvascular endothelial dysfunction (CMED), predicts the development of osteoporosis in postmenopausal women.
Methods: Coronary vascular reactivity was evaluated in 194 postmenopausal women greater than 50 years of age and with non-obstructive coronary arteries by administration of intracoronary acetylcholine during diagnostic angiography. CMED was defined as ≤50% increase in coronary blood flow from baseline in response to maximal dose. After a median follow-up of 7.0±0.3 years, patients were assessed by a questionnaire for development of osteoporosis.
Results: The average age of the cohort was 60.9±7.4 years. Women with CMED were twice as likely to develop osteoporosis compared with women without endothelial dysfunction after adjustment for potential confounders (relative risk, 2.4; 95% confidence interval [CI], 1.1, 5.6, P=0.02). Epicardial endothelial dysfunction was not associated with development of osteoporosis.
Discussion: Early coronary atherosclerosis with endothelial dysfunction is an independent marker for increased risk of developing osteoporosis in postmenopausal women greater than 50 years of age without obstructive coronary artery disease. The current study supports a link between coronary atherosclerosis and osteoporosis.
Keywords: coronary artery disease, endothelial dysfunction, endothelial progenitor cells, low bone mass, screening
Introduction
Cardiovascular disease and osteoporosis are two common age-related conditions that result in significant mortality and morbidity. Growing evidence suggests that there may be an association between coronary artery disease and osteoporosis. Traditionally, both diseases are thought to be concomitantly present due to age-related processes.1,2 However, the link between these two conditions is not entirely understood.
Low bone mineral density has been associated with increased cerebrovascular and cardiovascular morbidity and mortality, especially in women.3–6 The relationship between the early stage of atherosclerosis and osteoporosis is unknown. Endothelial dysfunction is an important early feature of atherosclerosis and coronary artery disease. The endothelium plays a critical role in regulating vascular tone via release of vasodilators such as nitric oxide, which maintain vasodilation, and inhibit platelet aggregation and leukocyte adhesion, thereby impeding the atherosclerotic process. Endothelial dysfunction as a potential link between cardiovascular disease and osteoporosis has previously been suggested by Sanada et al who studied healthy Japanese women and found that postmenopausal women with low bone mineral density have impaired endothelial function in forearm resistance arteries.7 Furthermore, endothelial progenitor cells may also play a role in a link between osteoporosis and coronary artery disease, as they are mobilized from the bone marrow in response to vascular injury.8,9
Due to the association previously described between osteoporosis and coronary artery disease, we aimed to test the hypothesis that women with coronary endothelial dysfunction are more likely to develop osteoporosis than women with normal coronary endothelial function.
Methods
Study design
This prospective single center cohort study was approved by the Institutional Review Board of the Mayo Foundation, and all subjects provided written and informed consent.
Study population
A total of 194 postmenopausal women greater than 50 years of age were enrolled. All patients presented with symptoms of chest pain and underwent cardiac catheterization and comprehensive assessment of coronary vasomotor function, including coronary endothelial function by administration of acetylcholine.8,9
Inclusion criteria included female sex, age greater than 50 years, and postmenopausal status. Exclusion criteria included significant coronary artery stenosis (>50%), ejection fraction <45%, unstable angina, previous myocardial infarction, use of radiographic contrast agents within 12 hours, significant systemic disease, and pregnancy. Medications that may affect cardiovascular hemodynamics were discontinued for at least 48 hours before the study.
Study protocol
All patients underwent diagnostic coronary angiography, and endothelial reactivity was assessed as previously described.8–10 A total of 5,000 units of heparin were infused intravenously, and a Doppler guide wire was positioned in the mid-left anterior descending artery. Acetylcholine was administered in increasing concentrations into the left anterior descending artery. Angiographic, hemodynamic, and coronary Doppler data were recorded as described previously.11–13 Both microvascular and epicardial blood flow were assessed. Microvascular coronary endothelial dysfunction was defined as ≤50% increase in coronary blood flow (CBF) from baseline in response to a maximal dose of acetylcholine. Epicardial dysfunction was defined as a decrease in epicardial coronary artery diameter greater than 20% in response to maximal dosage of acetylcholine.9,13
Follow-up
After a median follow-up of 7.0±0.3 years, patients enrolled in the study answered a standardized questionnaire that inquired about the presence of osteoporosis at the time of catheterization and subsequent development of osteoporosis following cardiac catheterization, either through diagnosis by primary care physician or through bone mineral density testing. The questionnaire also assessed a variety of other parameters including age, sex, medication use, other medical problems, and recurrent chest pain.
Statistical analysis
Statistical analysis was performed using JMP software (SAS Institute Inc., Cary, NC, USA). Continuous variables were presented as mean ± standard deviation, and categorical variables were presented as frequency (%). Student’s t-test was used to compare continuous variables, and categorical data were compared with the chi-square test. Cox proportional hazards regression modeling was used to assess for an independent association between coronary microvascular endothelial dysfunction and epicardial endothelial dysfunction and development of osteoporosis.
Results
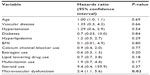
A total of 194 postmenopausal women without evidence of osteoporosis were enrolled in the study. Table 1 lists baseline characteristics of patients with and without osteoporosis. The average age of the cohort was 60.9 years ± 7.4 years. Hypertension was self-reported by 51.2% of the cohort, hyperlipidemia by 62.8%, known vascular disease by 7.7%, and diabetes by 5.6%. The average body mass index of the population was 28.2±6.2.
  | Table 1 Comparison of baseline characteristics between patients who did and did not develop osteoporosis |
Of 194 women, 119 (61.3%) were diagnosed with coronary microvascular endothelial dysfunction on angiography. Thirty-nine patients of the cohort (20.1%) developed osteoporosis during a median follow-up period of 8.4±4.7 years.
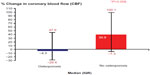
Women who developed osteoporosis had a markedly lower percent change in CBF in response to acetylcholine compared with women who did not develop osteoporosis: median (interquartile range), −4.3 (−29.4, 47.6) versus 39.9 (−7.3, 100.1); P=0.008 (Figure 1). In univariate analysis, coronary microvascular endothelial dysfunction was significantly associated with the development of osteoporosis (relative risk, 2.1; 95% confidence interval [CI], 1.06, 4.12; P=0.02).
Multivariable analysis adjusting for potential confounding variables including age, hyperlipidemia, hypertension, BMI, estrogen use, and steroid use, revealed that microvascular dysfunction remained significantly associated with the development of osteoporosis (relative risk, 2.4; 95% CI, 1.1, 5.6; P=0.02) (Table 2).
Epicardial microvascular dysfunction was not significantly associated with the development of osteoporosis in this cohort in both univariate and multivariable analyses adjusting for the same potential confounding factors (P>0.05).
Discussion
The current study suggests that coronary endothelial function is an independent predictor for development of self-reported osteoporosis in postmenopausal women after adjustment for potential confounders. Thus, endothelial dysfunction may be a common denominator linking increased risk of cardiovascular disease and mortality to low bone mineral density.
The association between cardiovascular disease and osteoporosis has been described extensively in the literature. Patients with osteoporosis have been shown to be more likely to have cardiovascular disease, and vice versa.2,14–17 Yet, there is a paucity of information regarding the link between the early stage of atherosclerosis and osteoporosis. The current study, supported by these previous observations, demonstrates a link between early atherosclerosis and osteoporosis.
Endothelial dysfunction may be a common precursor to both osteoporosis and coronary artery disease, potentially explaining the link noted between the two conditions. Endothelial dysfunction is an early stage of atherosclerosis, but is also considered to be an important regulator of vascular and bone health.8,9,13 The endothelium plays an important role in mediating vascular processes such as inflammation, vasodilatation/vasoconstriction, thrombosis, and oxidation. Endothelial dysfunction prevents appropriate balance of these processes, playing a key role in initiating atherosclerosis.16
Nitric oxide is a possible explanation for the link seen between atherosclerosis and osteoporosis. Nitric oxide may play a role in bone metabolism via osteoblastic activity.16,18,19 High concentrations of nitric oxide can directly inhibit spreading of osteoclasts and bone resorption, and stimulate or inhibit bone resorption depending on cytokine stimulation.20 Cytokines such as interleukin-1, tumor necrosis factor, and interferon may inhibit osteoblast growth since nitric oxide is produced by osteoblast-like cells in response to pro-inflammatory cytokines, inhibiting osteoblast proliferation and suggesting a role for nitric oxide in bone remodeling.21 Isosorbide mononitrate is associated with reduced urine N-telopeptide levels, which is a marker of bone resorption, and increased levels of alkaline phosphatase, a marker of bone formation, further suggesting nitric oxide as a possible mediator of bone formation.22 When endothelial function is impaired, nitric oxide and its physiologic function can also become impaired, potentially limiting the normally beneficial effects of nitric oxide on bone formation.
Another potential mechanism for this link is based on the premise that endothelial progenitor cells (EPCs) residing in the marrow may be mobilized in response to vascular injury.23 EPCs are mobilized from the bone marrow into circulation and migrate to affected areas to aid in tissue recovery. Traditionally, endothelial and osteoblastic cells have been thought to be derived from two separate progenitor lines; however, increasing evidence suggests that there may be an overlap between these two cell lines. This potential role of EPCs in bone formation is further supported by research that shows these cells can be differentiated into osteoblastic cells,9 supporting the notion that endothelial progenitor cells may have a role in vascular calcification.9 Our group suggested a link between these two seemingly different cell lines when it identified a group of EPCs derived from the bone marrow, which are costained using flow cytometry for osteocalcin (OCN+), an osteoblast marker.9
We have previously reported a greater number of EPCs expressing osteocalcin (OCN+ EPCs) in patients with early coronary atherosclerosis as opposed to patients with normal coronary arteries and no endothelial dysfunction.9 We also found that these EPCs can form mineralized deposits. Patients with CMED retain OCN+ EPCs in coronary circulation when compared with patients without coronary endothelial dysfunction. This further supports the potential relationship between endothelial dysfunction and osteoporosis. Increased numbers of circulating OCN+ EPCs in patients with endothelial dysfunction may contribute to vascular insult and initiation of atherosclerosis, especially with vascular calcification.13 These osteogenic cells may contribute to worsened calcification rather than bone formation. Thus, documented presence of EPCs expressing osteocalcin has been established in patients with early atherosclerosis, endothelial dysfunction, and coronary artery disease.9
There may also be an inflammatory component contributing to the pathophysiologic process as well. Our group has also found that patients with endothelial dysfunction have higher levels of inflammatory cytokines such as interleukin-8.9,13 Such cytokines have been shown to attract EPCs to ischemic areas of the myocardium, further contributing to altered repair of the endothelium.13,24
Our finding that CMED may be associated with the development of osteoporosis is thus plausible. Patients with endothelial dysfunction and early atherosclerosis have impaired bone metabolism, leading to osteoporosis. This in turn leads to increasing levels of OCN+ EPCs, further worsening endothelial function. While many studies have shown a link between coronary artery disease and osteoporosis, there is little clinical data suggesting endothelial dysfunction is associated with osteoporosis. Our findings are consistent with a previous study that showed that postmenopausal women with low bone mineral density have impaired endothelial function in the forearm resistance arteries.7
Our study has several inherent limitations. Our conclusions are based on a standardized questionnaire administered several years after angiography. While bone mineral density studies would have utility in better delineating whether microvascular dysfunction predicts osteoporosis, the strong association we note even with simple questionnaires relying only on self-report and chart review is compelling. Furthermore, not all patients completed the survey, and when there is an incomplete follow-up, there is a possibility for inherent resulting bias. Future studies should be directed at assessing this association with bone mineral density studies.
Conclusion
While the association between cardiovascular disease and osteoporosis has been suggested previously, our findings suggest that endothelial dysfunction may be the underlying mechanism linking these two disease processes. Further research is warranted to determine whether women with low bone mass should undergo more extensive screening and management to delay development of osteoporosis, or whether women with known coronary endothelial dysfunction should be treated in an effort to prevent osteoporosis.
Disclosure
The authors report no conflicts of interest in this work.
References
Farhat GN, Cauley JA. The link between osteoporosis and cardiovascular disease. Clin Cases Miner Bone Metab. 2008;5:19–34. | |
Aoyagi K, Ross PD, Orloff J, Davis JW, Katagiri H, Wasnich RD. Low bone density is not associated with aortic calcification. Calcif Tissue Int. 2001;69:20–24. | |
Browner WS, Pressman AR, Nevitt MC, Cauley JA, Cummings SR. Association between low bone density and stroke in elderly women. The study of osteoporotic fractures. Stroke. 1993;24:940–946. | |
Tankó LB, Christiansen C, Cox DA, Geiger MJ, McNabb MA, Cummings SR. Relationship between osteoporosis and cardiovascular disease in postmenopausal women. J Bone Miner Res. 2005;20:1912–1920. | |
von der Recke P, Hansen MA, Hassager C. The association between low bone mass at the menopause and cardiovascular mortality. Am J Med. 1999;106:273–278. | |
Samelson EJ, Kiel DP, Broe KE, et al. Metacarpal cortical area and risk of coronary heart disease: the Framingham Study. Am J Epidemiol. 2004;159:589–595. | |
Sanada M, Taguchi A, Higashi Y, et al. Forearm endothelial function and bone mineral loss in postmenopausal women. Atherosclerosis. 2004;176:387–392. | |
Gössl M, Khosla S, Zhang X, et al. Role of circulating osteogenic progenitor cells in calcific aortic stenosis. J Am Coll Cardiol. 2012;60:1945–1953. | |
Gössl M, Mödder UI, Atkinson EJ, Lerman A, Khosla S. Osteocalcin expression by circulating endothelial progenitor cells in patients with coronary atherosclerosis. J Am Coll Cardiol. 2008;52:1314–1325. | |
Flammer AJ, Gössl M, Li J, et al. Patients with an HbA1c in the prediabetic and diabetic range have higher numbers of circulating cells with osteogenic and endothelial progenitor cell markers. J Clin Endocrinol Metab. 2012;97:4761–4768. | |
Han SH, Bae JH, Holmes DR Jr, et al. Sex differences in atheroma burden and endothelial function in patients with early coronary atherosclerosis. Eur Heart J. 2008;29:1359–1369. | |
Hasdai D, Gibbons RJ, Holmes DR Jr, Higano ST, Lerman A. Coronary endothelial dysfunction in humans is associated with myocardial perfusion defects. Circulation. 1997;96:3390–3395. | |
Gössl M, Mödder UI, Gulati R, et al. Coronary endothelial dysfunction in humans is associated with coronary retention of osteogenic endothelial progenitor cells. Eur Heart J. 2010;31:2909–2914. | |
Vogt MT, Cauley JA, Kuller LH, Nevitt MC. Bone mineral density and blood flow to the lower extremities: the study of osteoporotic fractures. J Bone Miner Res. 1997;12:283–289. | |
Frye MA, Melton LJ III, Bryant SC, et al. Osteoporosis and calcification of the aorta. Bone Miner. 1992;19:185–194. | |
Warburton DE, Nicol CW, Gatto SN, Bredin SS. Cardiovascular disease and osteoporosis: balancing risk management. Vasc Health Risk Manag. 2007;3:673–689. | |
Sinnott B, Syed I, Sevrukov A, Barengolts E. Coronary calcification and osteoporosis in men and postmenopausal women are independent processes associated with aging. Calcif Tissue Int. 2006;78:195–202. | |
Eastell R, Newman C, Crossman DC. Cardiovascular disease and bone. Arch Biochem Biophys. 2010;503:78–83. | |
Manolagas SC. From estrogen-centric to aging and oxidative stress: a revised perspective of the pathogenesis of osteoporosis. Endocr Rev. 2010;31:266–300. | |
MacIntyre I, Zaidi M, Alam AS, et al. Osteoclastic inhibition: an action of nitric oxide not mediated by cyclic GMP. Proc Natl Acad Sci U S A. 1991;88:2936–2940. | |
Ralston SH, Todd D, Helfrich M, Benjamin N, Grabowski PS. Human osteoblast-like cells produce nitric oxide and express inducible nitric oxide synthase. Endocrinology. 1994;135:330–336. | |
Nabhan AF. A randomized clinical trial of the effects of isosorbide mononitrate on bone formation and resorption in post-menopausal women: a pilot study. Hum Reprod. 2006;21:1320–1324. | |
Urbich C, Dimmeler S. Endothelial progenitor cells: characterization and role in vascular biology. Circ Res. 2004;95:343–353. | |
Kocher AA, Schuster MD, Bonaros N, et al. Myocardial homing and neovascularization by human bone marrow angioblasts is regulated by IL-8/Gro CXC chemokines. J Mol Cell Cardiol. 2006;40:455–464. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.