Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 12
Coronal Tooth Discoloration After the Use of White Mineral Trioxide Aggregate
Authors Tripathi R, Cohen S, Khanduri N
Received 16 June 2020
Accepted for publication 9 September 2020
Published 30 September 2020 Volume 2020:12 Pages 409—414
DOI https://doi.org/10.2147/CCIDE.S266049
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Christopher E. Okunseri
Rupam Tripathi,1 Stephen Cohen,2 Nitin Khanduri3
1Department of Conservative Dentistry and Endodontics, UCMS College of Dental Surgery, Bhairahawa, Nepal; 2American Board of Endodontics, San Francisco, CA, USA; 3Department of Pedodontics and Preventive Dentistry, Seema Dental College and Hospital, Rishikesh, Uttarakhand, India
Correspondence: Rupam Tripathi
Department of Conservative Dentistry and Endodontics, UCMS College of Dental Surgery, Bhairahawa, Nepal
Tel +9779856012388
Email [email protected]
Abstract: Mineral trioxide aggregate (MTA) has been used in regenerative procedures but observations have indicated that with its use there is dark staining of the tooth structure. This case report describes the treatment of tooth discoloration caused by white mineral trioxide aggregate (WMTA). Revascularization was performed with the use of WMTA in the upper left central incisor. Grayish discoloration appeared 9 months later, the tooth necessitating internal bleaching of the tooth. A significant improvement was observed in the crown after internal bleaching. The choice of material should not rely solely on biological and functional aspects, but aesthetic considerations should also be taken into account. The patient needs to be advised of risks, benefits, and alternatives to internal bleaching, eg, a veneer or a crown. Coronal discoloration is a significant distraction and embarrassment for many people in achieving an aesthetic smile; thus, it must be corrected at the earliest possible stage of discoloration.
Keywords: discoloration, internal bleaching, revascularization, WMTA, white mineral trioxide aggregate
Introduction
Dental trauma suffered by a child may lead to pulpal necrosis, resulting in a tooth with thin, fragile root canal walls and an open apex, making it more prone to fracture. For many years, the recommended treatment for developing teeth with pulpal necrosis has been apexification with calcium hydroxide or mineral trioxide aggregate (MTA). But this neither promotes significant root development1 nor restores the immunological function of the pulp. Regenerative endodontic therapy is a biologically based procedure in which the treatment of immature permanent teeth with infected root canal systems results in continued root maturation and apical closure. Regenerative endodontics focuses on substituting a traumatized pulp with fully functional pulp tissue. The clinical considerations for regenerative endodontic protocols are disinfection of the root canal system, provision of a scaffold, which often involves laceration of the periapical tissue to induce a blood clot and introduce stem cell activity within the root canal, and an adequate coronal seal to prevent reinfection.2–6
After stimulating intracanal bleeding, the blood clots are covered with calcium hydroxide and MTA. MTA is one of the most versatile materials. Gray MTA was developed in 1993. One of the potential drawbacks of gray MTA is tooth discoloration; this observation led to the development of white mineral trioxide aggregate (WMTA). For the past few years, however, clinical concerns have arisen over discoloration with the use of WMTA too, particularly when used in the aesthetic zone.7,8 So, this case report focuses on coronal discoloration caused by MTA and its management.
Case Report
A 17-year-old male patient was referred to the Department of Conservative Dentistry and Endodontics, UCMS-CODS, with pain while biting in the anterior maxilla region of jaw for the past month. There was a history of trauma 1 year earlier. The patient had a non-contributory medical and dental history. On clinical examination, there was yellowish discoloration in respect to #51 and #61 but he was not concerned by it. Both teeth were tender to percussion. Mobility was within a normal range. Both teeth showed no response on thermal and electric pulp tests. Radiography revealed radiolucent periapical lesions in respect to teeth #51 and #61 and radiolucency in the lateral aspect of #51 as well (Figure 1). The diagnosis of necrotic pulp with symptomatic apical periodontitis was made. Parental informed and written consent was obtained for procedures and to publish all case details and any accompanying images. Institutional approval was not required for publication of data.
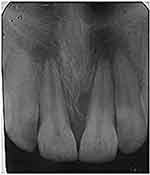 |
Figure 1 Preoperative radiograph with periapical radiolucencies # 51 and 61. |
Root canal treatment was carried out in #51 and a regenerative procedure was performed in #61. Tooth isolation was obtained with a rubber dam and access cavity preparation was performed in #61. The working length was determined using digital radiography and a Root ZX apex locator (J. Morita, Tokyo, Japan) with a no. 15 K file (Dentsply Maillefer, Ballaigues, Switzerland). The root canal system was irrigated with 20 mL of 5.25% NaOCl followed by 20 mL of 17% EDTA. Double antibiotic paste (ciprofloxacin, metronidazole) was used as intracanal medicament for 3 weeks. At the next visit, the patient was asymptomatic. Local infiltration anesthesia was performed with 2% plain lignocaine, without a vasoconstrictor to facilitate bleeding. The antibiotic intracanal medicament was flushed out of the canal with copious irrigation with 5.25% NaOCl. After drying the canal, bleeding was induced inside the canal with a sterile no. 50 K file, which was inserted 1 mm beyond the apical foramen, and the middle and coronal part of the canal was sealed with ProRoot MTA (Dentsply Tulsa Dental, Tulsa, OK, USA) over the blood clot. A moist cotton pellet was placed over the MTA in the access cavity, and the tooth was temporarily restored with Cavit W (3M, Dental Products Division, St Paul, MN). After 24 hours, the cotton was removed and the tooth was restored with composite.
The patient was reviewed at 3, 6, and 9 months. After 9 months, the patient came to the department with grayish discoloration in #61 and now he was concerned by the crown discoloration (Figure 2). The periapical lesion that was present in #61 had healed and continued apical root maturation was radiographically evident. The lesion that was present periapically in #51 was in the state of healing, whereas the lesion in its lateral aspect had healed (Figure 3). The patient was advised of different treatment options such as internal bleaching, a veneer, or a crown. The patient was also advised of the risks of internal bleaching. As internal bleaching is an economical dental treatment, patient was convinced by this option only. Internal bleaching was performed with sodium perborate (Sodium Perborate Teeth Whitening; Sultan Healthcare). A mixture of sodium perborate and saline was placed in the access cavity to internally bleach the crown. Then, the access opening was sealed with Cavit W (3M, Dental Products Division, St Paul, MN). The patient returned 2 weeks later and the same procedure was repeated. After completion of the bleaching procedures, under rubber dam isolation, the tooth was reaccessed, the internal bleaching paste was removed, and the access cavity was subsequently restored with resin composite restoration (Figure 4).
 |
Figure 2 Grayish discoloration #61. |
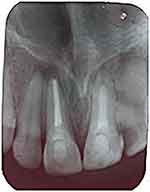 |
Figure 3 Image taken 9 months later revealing significant remineralization in the periapical region. |
 |
Figure 4 Photograph after completion of bleaching procedures. |
Discussion
This case report demonstrates the management of discoloration of tooth #61 after the placement of WMTA. MTA is a material used worldwide in a variety of clinical applications, such as providing an apical barrier for teeth with immature apices, repair of root perforations, as final canal filling material when the tooth is treated by the regenerative endodontic treatment procedure, root-end filling, pulp capping, and pulpotomy procedures.9,10 Pulp revascularization is considered to be the treatment method in order to save the tooth and promote root development.
Color is one of the most important properties to be observed during dental procedures involving teeth in the aesthetic areas. Several studies have confirmed that triple antibiotic paste can discolor teeth.11 Triple antibiotic paste used between appointments is found to be one of the most common reasons for discoloration after the regeneration procedure. The first triple antibiotic paste introduced for bacterial disinfection contained metronidazole, ciprofloxacin, and minocycline,12 and the minocycline that binds to the calcium of hydroxyapatite has been reported to be the main cause of this discoloration.7 The American Association of Endodontics (AAE) guidelines have recommended the use of either calcium hydroxide or a low concentration of triple or double antibiotic paste as the medicament below the cementoenamel junction. A double antibiotic paste was used as an intracanal medicament in the present case, as several studies suggest that calcium hydroxide is insufficient in completely removing bacteria from root canals compared to double or triple antibiotic paste.13
In this case, successful revascularization treatment of an immature maxillary right central incisor was carried out using WMTA. MTA is composed mainly of tricalcium and dicalcium silicates. The radiopacity is provided by the addition of approximately 20% bismuth oxide. The color stability of MTA is a critical property to be considered when treating aesthetic areas. The cause of discoloration is still debatable. There are many theories about the mechanism of tooth discoloration induced by WMTA (Table 1).14–16 Several in vitro and ex vivo studies have shown that the WMTA discolors teeth when it interacts with sodium hypochlorite, the tooth structure, and the blood. Sodium hypochlorite in contact with bismuth oxide results in a black precipitate. There is a chemical interaction of bismuth oxide (Bi2O3) with dentin too, resulting in the formation of reduced black crystals of bismuth atoms.17,18 The amino acids in collagen seem to destabilize the Bi2O3 molecule, leading to its reaction and eventual change in color to black. Metal oxides such as Fe and Mn are also reported to cause discoloration.18 Studies have shown that discoloration can also be caused by the interaction of WMTA with blood. Unset WMTA permits the absorption and subsequent hemolysis of erythrocytes from the adjacent pulpal tissue.19
 |
Table 1 Different Chemical Reactions of WMTA That Lead to Discoloration |
The reason for extensive discoloration, in this case, could be because of WMTA itself. Several case reports have also described coronal tooth discoloration associated with WMTA.20 Naik and Hegde reported that when MTA was used for pulpotomy in primary molars, discoloration occurred in 60% of all cases.21 Belobrov and Parashos also presented a case report of a complicated crown fracture treated by partial pulpotomy with WMTA that resulted in tooth discoloration.22
Endodontically treated and discolored teeth can be whitened using bleaching agents. Bleaching agents composed of hydrogen peroxide, sodium perborate, carbamide peroxide, glycerine or propylene glycol, sodium stannate, phosphoric or citric acid, and flavor additives. In some preparations, carbopol, a water-soluble polyacrylic acid polymer, is added as a thickening agent. In the present case, non-vital bleaching was performed with sodium perborate as it is safe and effective.23,24 More than 90% immediate success has been reported with the conventional “walking bleach” procedure. However, the need for retreatment increased with the observation time. Internal discoloration caused by root canal medicaments, root-filling materials, or metallic restorations such as amalgam have a poor prognosis, as this type of discoloration tends to reappear over time because of the tenacity of the oxidizing products to dental tissues. In one study, a 7% failure rate was reported after 5 years.25 So, the patient needs to be advised of the risks, benefits, and alternatives to internal bleaching, such as a veneer or a crown.
We used a combination of sodium peroxide and water in the present case. Ari and Ungor reported that sodium perborate should be mixed with water rather than with hydrogen peroxide in order to prevent or minimize the occurrence of bleaching-related external root resorption.26 A highly concentrated oxidizing agent, eg, 30–35% hydrogen peroxide, can diffuse via unprotected dentinal tubules, the cervical cementum, and the periodontal ligament, initiating an inflammatory reaction. This process may be enhanced if heat is applied or in the presence of bacteria. In some cases, the presence of papillary swelling and tenderness to percussion was noted.27
In the present case, bismuth oxide, the radiopacifier present in MTA, has been suggested as the chemical compound involved with the discoloration.28 Zirconium oxide may be an alternative to bismuth oxide. A previous study showed that a zirconium oxide-containing MTA induced less discoloration than MTAs containing Bi2O3.29 Material based on tricalcium silicates with alternative radiopacifiers, such as Biodentin, NeoMTA Plus, and Retro-MTA, is available clinically.
Conclusion
MTA appears to be a promising successor to calcium hydroxide for pulpal and periodontal healing, despite the fact that several studies have shown its discoloration. Chemical interaction with dental structures is still not clear and requires further investigation. So, the recommendation to use WMTA in the aesthetic zone should be reconsidered. The dental community should have common knowledge about the materials used in endodontics that may cause discoloration and thus can impair the aesthetic outcome of the treated tooth.
Acknowledgments
We would like to thank Dr Manu Batra, Dr Manisha Nepal, and Dr Chetna Arora for their contributions to this manuscript.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Lin J, Zeng Q, Wei X, et al. Regenerative endodontics versus apexification in immature permanent teeth with apical periodontitis: a prospective randomized controlled study. J Endod. 2017;43(11):1821–1827. doi:10.1016/j.joen.2017.06.023
2. Bezgin T, Sonmez H. Review of current concepts of revascularization/revitalization. Dent Traumatol. 2015;31(4):267–273. doi:10.1111/edt.12177
3. Diogenes A, Henry MA, Teixeira FB, Hargreaves KM. An update on clinical regenerative endodontics. Endod Topics. 2013;28(1):2–23.
4. Galler KM. Clinical procedures for revitalization: current knowledge and considerations. Int Endod J. 2016;49(10):926–936. doi:10.1111/iej.12606
5. Hargreaves KM, Giesler T, Henry M, Wang Y. Regeneration potential of the young permanent tooth: what does the future hold? J Endod. 2008;34(7):51–56. doi:10.1016/j.joen.2008.02.032
6. Kontakiotis EG, Filippatos CG, Tzanetakis GN, Agrafioti A. Regenerative endodontic therapy: a data analysis of clinical protocols. J Endod. 2015;41(2):146–154. doi:10.1016/j.joen.2014.08.003
7. Lenherr P, Allgayer N, Weiger R, Filippi A, Attin T, Krastl G. Tooth discoloration induced by endodontic materials: a laboratory study. Int Endod J. 2012;45(10):942–949. doi:10.1111/j.1365-2591.2012.02053.x
8. Krastl G, Allgayer N, Lenherr P, Filippi A, Taneja P, Weiger R. Tooth discoloration induced by endodontic materials: a literature review. Dent Traumatol. 2013;29(1):2–7. doi:10.1111/j.1600-9657.2012.01141.x
9. Iwaya SI, Ikawa M, Kubota M. Revascularization of an immature permanent tooth with apical periodontitis and sinus tract. Dent Traumatol. 2001;17(4):185–187. doi:10.1034/j.1600-9657.2001.017004185.x
10. Banchs F, Trope F. Revascularization of immature permanent teeth with apical periodontitis: new treatment protocol? J Endod. 2004;30(4):196–200. doi:10.1097/00004770-200404000-00003
11. Akbulut MB, Terlemez A, Akman M, Buyukerkmen B, Guneser MB, Eldeniz AU. Tooth discoloration effects of calcium silicate based barrier materials used in revascularization and treatment with internal bleaching. J Dent Sci. 2017;12(4):347–353.
12. Hoshino E, Kurihara-Ando N, Sato I, et al. In-vitro antibacterial susceptibility of bacteria taken from infected root dentine to a mixture of ciprofloxacin, metronidazole and minocycline. Int Endod J. 1996;29(2):125–130. doi:10.1111/j.1365-2591.1996.tb01173.x
13. Kvist T, Molander A, Dahlén G, Reit C. Microbiological evaluation of one- and two-visit endodontic treatment of teeth with apical periodontitis: a randomized, clinical trial. J Endod. 2004;30(8):572–576. doi:10.1097/01.DON.0000121607.87969.6E
14. Marconyak LJ, Kirkpatrick TC, Roberts HW, et al. A comparison of coronal tooth discoloration elicited by various endodontic reparative materials. J Endod. 2016;42(3):470–473. doi:10.1016/j.joen.2015.10.013
15. Camilleri J. Color stability of white mineral trioxide aggregate in contact with hypochlorite solution. J Endod. 2014;40(3):402–436. doi:10.1016/j.joen.2013.09.040
16. Jang JH, Kang M, Ahn S, et al. Tooth discoloration after the use of new pozzolan cement (Endocem) and mineral trioxide aggregate and the effects of internal bleaching. J Endod. 2013;39(12):1598–1602. doi:10.1016/j.joen.2013.08.035
17. Valles M, Mercade M, Duran-Sindreu F, Bourdelande JL, Roig M. Color stability of white mineral trioxide aggregate. Clin Oral Investig. 2013;17(4):1155–1159. doi:10.1007/s00784-012-0794-1
18. Ioannidis K, Mistakidis I, Beltes P, Karagiannis V. Spectrophotometric analysis of crown discoloration induced by MTA- and ZnOE-based sealers. J Appl Oral Sci. 2013;21(2):138–144. doi:10.1590/1678-7757201302254
19. Felman D, Parashos P. Coronal tooth discoloration and white mineral trioxide aggregate. J Endod. 2013;39(4):484–487. doi:10.1016/j.joen.2012.11.053
20. Jacobovitz M, De Lima RK. Treatment of inflammatory internal root resorption with mineral trioxide aggregate: a case report. Int Endod J. 2008;41(10):905–912.
21. Naik S, Hegde AH. Mineral trioxide aggregate as a pulpotomy agent in primary molars: an in vivo study. J Indian Soc Pedod Prev Dent. 2005;23(1):13–16.
22. Belobrov I, Parashos P. Treatment of tooth discoloration after the use of white mineral trioxide aggregate. J Endod. 2011;37(7):1017–1020. doi:10.1016/j.joen.2011.04.003
23. Plotino G, Buono L, Grande NM, Pameijer CH, Somma F. Nonvital tooth bleaching: a review of the literature and clinical procedures. J Endod. 2008;34(4):394–407. doi:10.1016/j.joen.2007.12.020
24. Attin T, Paque F, Ajam F, Lennon AM. Review of the current status of tooth whitening with the walking bleach technique. Int Endod J. 2003;36:313. doi:10.1046/j.1365-2591.2003.00667.x
25. Dahl JE, Pallesen U. Tooth bleaching – a critical review of the biological aspects. Rev Oral Biol Med. 2003;14(4):292–304. doi:10.1177/154411130301400406
26. Ari H, Ungor M. In vitro comparison of different types of sodium perborate used for intracoronalbleaching of discoloured teeth. Int Endod J. 2002;35:433–436. doi:10.1046/j.1365-2591.2002.00497.x
27. Fearon J. Tooth whitening: concepts and controversies. J Iran Dent Assoc. 2007;53:132–140.
28. Vallés M, Mercadé M, Duran-Sindreu F, Bourdelande JL, Roig M. Influence of light and oxygen on the color stability of five calcium silicate-based materials. J Endod. 2013;39(4):525–528. doi:10.1016/j.joen.2012.12.021
29. Kim SO, Shin Y, Jung IY, et al. Color changes of teeth after treatment with various mineral trioxide aggregate-based materials: an ex vivo study. J Endod. 2015;41:737–741. doi:10.1016/j.joen.2015.01.019
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
