Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 14
COPD treatment pathways in France: a retrospective analysis of electronic medical record data from general practitioners
Authors Meeraus W, Wood R , Jakubanis R, Holbrook T, Bizouard G, Despres J, Correia Da Silva C, Nachbaur G, Landis SH, Punekar Y , Aguilaniu B, Ismaila AS
Received 24 July 2018
Accepted for publication 5 November 2018
Published 18 December 2018 Volume 2019:14 Pages 51—63
DOI https://doi.org/10.2147/COPD.S181224
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Wilhelmine Meeraus,1 Robert Wood,2 Rafal Jakubanis,2 Tim Holbrook,2 Geoffray Bizouard,3 Johanna Despres,3 Camille Correia Da Silva,4 Gaelle Nachbaur,4 Sarah H Landis,1 Yogesh Punekar,5 Bernard Aguilaniu,6 Afisi S Ismaila7,8
1GlaxoSmithKline, Stockley Park West, Uxbridge, UK; 2Adelphi Real World, Bollington, Cheshire, UK; 3IQVIA, Paris, France; 4GlaxoSmithKline, Rueil-Malmaison, France; 5ViiV Healthcare, Brentford, Middlesex, UK; 6Faculty of Medicine, University Grenoble-Alpes, Grenoble, France; 7GlaxoSmithKline, Collegeville, PA, USA; 8Department of Health Research Methods, Evidence and Impact, McMaster University, Hamilton, ON, Canada
Background: Increasing availability of therapeutic options for COPD may drive new treatment pathways. This study describes COPD treatment in France, focusing on identifying initial treatment modifications in patients with COPD who either initiated long-acting bronchodilator (LABD)-based therapy or escalated to triple therapy (long-acting muscarinic antagonist [LAMA] + long-acting β2-agonist [LABA] + inhaled corticosteroid [ICS]).
Methods: This retrospective analysis of patients with COPD in a large general practitioner database (IQVIA Longitudinal Patient Database) in France included two cohorts: Cohort 1 – new initiators of LABD-based therapy (LAMA, LABA, LAMA + LABA, LAMA + ICS, LABA + ICS or LAMA + LABA + ICS); Cohort 2 – patients escalating to triple therapy from mono- or dual-bronchodilator-based maintenance treatment. Both cohorts were indexed on the date of initiation/escalation (January 2008–December 2013), and the first treatment modification (at class level) within the 18-month post-index observational period was described. Five mutually exclusive outcomes were defined: continuous use (no modification), discontinuation (permanent [≥91 days with no restart] or temporary [≥91 days with subsequent restart]), switch, and augmentation (Cohort 1 only). Exploratory analysis of Cohort 1 explored potential drivers of treatment initiation.
Results: Overall, 5,065 patients initiated LABD-based therapy (Cohort 1), and 501 escalated to triple therapy (Cohort 2). In Cohort 1, 7.0% of patients were continuous users, 46.5% discontinued permanently, 28.5% discontinued temporarily, 2.8% augmented (added LAMA and/or LABA and/or ICS), and 15.2% switched therapy. In Cohort 2, 18.2% of patients were continuous users, 7.2% discontinued permanently, 27.9% discontinued temporarily, and 46.7% switched therapy. Exploratory analyses showed that time since COPD diagnosis was first recorded, pre-index exacerbation events, and concomitant medical conditions were potential drivers of initial maintenance treatment choices.
Conclusion: Discontinuation among new initiators of LABD-based therapy was high in France, whereas few switched or augmented treatment. In comparison, permanent discontinuation within 18 months was low in patients escalating to triple therapy.
Keywords: triple therapy, France, treatment pathways, treatment modification, maintenance therapy
Background
COPD is a respiratory disease characterized by chronic obstruction of lung airflow that interferes with normal breathing.1 It is a leading cause of morbidity and mortality and is associated with a high clinical and economic burden.1 COPD is currently listed as the fourth leading cause of death in countries with a middle sociodemographic index (ranked fourth to 20th depending on the sociodemographic index),2 and the World Health Organization estimates that it will become the third leading cause of death worldwide in 2030.3 This high epidemiological and economic burden was also observed in a study of medico-administrative databases in France.4
Currently, the most commonly used maintenance medications for COPD include bronchodilators (eg, long-acting β2-agonist [LABA] and long-acting muscarinic antagonist [LAMA], alone or in combination) and inhaled corticosteroid (ICS; used in combination with a LABA, or a LAMA and a LABA [triple therapy]).1 Studies have shown that LAMA/LABA combinations provide added benefits in terms of improved lung function, health status, and health-related quality of life (HRQoL), and reduce exacerbation rates vs monotherapy components.5–12 Additional studies have shown that triple therapy in multiple and single inhalers provides further benefits (improved lung function, HRQoL and patient-reported outcomes, and reduced morbidity, mortality, and exacerbation rates) vs ICS/LABA combination therapy and LAMA monotherapy.13–21 The Société de Pneumologie de Langue Francaise (SPLF) 2009 French COPD treatment guidelines recommended treatment regimens based on disease severity as measured by lung function (FEV1 and FEV1/FVC ratio).22 Mono- or dual-bronchodilator therapy with LAMA and/or LABA was recommended for patients with moderate COPD, and combination treatment with LABA + ICS was recommended for patients with severe or very severe COPD (post-bronchodilator FEV1 <50% predicted [<60% for salmeterol + fluticasone propionate]) who have a history of exacerbations and remain symptomatic despite treatment with a long-acting bronchodilator (LABD). The most recently published SPLF guidelines (2016) recommend initial monotherapy with LAMA or LABA, and escalation to LAMA + LABA, LABA + ICS, or triple therapy for patients who experience additional symptoms or exacerbations.23
With multiple classes of drugs now available for the pharmacological treatment of COPD in France, the treatment armamentarium available to clinicians has expanded; however, these options have reintroduced instability and uncertainty regarding treatment pathways in COPD. For example, a recently published retrospective cohort study set within UK primary care showed differential patterns of escalation and switch, with multiple pathways for escalating to triple therapy.24
This study aimed to identify the treatment pathways followed by two specific groups of patients in France: patients who are prescribed a maintenance therapy for the first time by their general practitioner (GP), for example, initiators of LABD-based treatment (LAMA, LABA, LAMA + LABA, LAMA + ICS, LABA + ICS, or triple therapy [LAMA + LABA + ICS]), and patients with greater disease severity who are escalating to triple therapy (with multiple inhalers). Specifically, the study describes the types of initial maintenance therapy prescribed, and the first treatment modification in the 18 months following either initiation of LABD-based maintenance therapy or escalation to triple therapy. The study also assessed potential drivers of choice of initial COPD maintenance therapy in exploratory analyses.
Methods
Study design
This was a retrospective analysis of patients with COPD in a large GP database (IQVIA Longitudinal Patient Database) in France from June 2006 to June 2015 (GlaxoSmithKline [GSK] study number: HO-15-16099). The database comprises electronic medical records collected routinely through a panel of GPs. It includes prescription data, medical history, and outpatient diagnosis information for ~1.8 million active patients living in metropolitan France, with data going back to 1994. The overall study sample was divided into two cohorts. Cohort 1 comprised patients with COPD initiating maintenance treatment (ie, newly prescribed, by their GP, LAMA, LABA, LAMA + LABA, LAMA + ICS, LABA + ICS, or triple therapy [LAMA + LABA + ICS]) from January 1, 2008 to December 31, 2013; the index date in this cohort was the date of the first maintenance treatment prescription (Figure 1). New use of a maintenance treatment in the context of this study was defined as not having had a GP prescription for any maintenance treatments during the 18-month pre-index period. Cohort 2 comprised patients with COPD already on maintenance treatment (LAMA, LABA, LAMA + LABA, LAMA + ICS, or LABA + ICS) and escalating to triple therapy (LAMA + LABA + ICS) from January 1, 2008 to December 31, 2013; the index date in this cohort was the date of triple therapy initiation (ie, the date of the first prescription that contained all three components of triple therapy; Figure 1). For the dual therapies (LAMA + LABA, LAMA + ICS, and LABA + ICS), both fixed-dose and multiple-inhaler combinations were considered. Single-inhaler triple therapy was not available in France at the time of the study, so only multiple-inhaler triple therapies were included in this analysis. The study included an 18-month pre-index baseline period and an 18-month post-index observational period (Figure 1). Because information on death and transfer out of the GP practice was unavailable, the earliest and latest recorded events of any type in the database (for a particular patient) were considered the start of availability of pre-index baseline data and end of availability of post-index observational data, respectively.
  | Figure 1 Study design. |
This study was designed, implemented, and reported in accordance with the Guidelines for Good Pharmacoepidemiology Practices of the International Society for Pharmacoepidemiology,25 the Strengthening the Reporting of Observational Studies in Epidemiology guidelines,26 and with the ethical principles laid down in the Declaration of Helsinki. The study involved no interventions or treatment, and no identifiable patient data were collected; therefore, neither informed patient consent nor institutional review board/ethics committee approval was required. This was a retrospective database analysis using existing data. Personal identifiers were not required, and personally identifiable information was removed by the database provider prior to receipt by the study team.
Patient eligibility and subgroups
Eligible patients were adults ≥40 years of age on the date of indexing, with evidence of a clinical diagnosis of COPD according to the International Classification of Disease, 10th edition (ICD-10) prior to or including the index date (ICD-10 codes J41.x, J42, J43.x, J44.x), with at least 18 months of pre-index and post-index data available.
Patients with a diagnosis of asthma or a respiratory disease potentially incompatible with COPD diagnosis in the pre- or post-index period (eg, conditions that are related to lung or bronchial developmental anomalies, degenerative processes [cystic fibrosis, pulmonary fibrosis], bronchiectasis, pulmonary resection, or other significant respiratory disorders other than COPD; Table S1), and who had a prescription of a LABD-based treatment (Cohort 1 [patients initiating maintenance treatment]) or triple therapy (Cohort 2 [patients escalating to triple therapy]) in the pre-index period were excluded from this analysis. Patients initiating maintenance treatment (Cohort 1) were classified into subgroups according to the therapy class they initiated (eg, LAMA, LABA, LAMA + LABA, LAMA + ICS, LABA + ICS, or triple therapy).
Treatment modification outcomes
Five mutually exclusive treatment modification outcomes were defined based on first treatment change (at class level) within the 18-month post-index observational period: continuous users (no modification); permanent discontinuers; temporary discontinuers (ie, with drug hiatus); augmenters (in Cohort 1 [patients initiating maintenance treatment] only); and switchers.
Discontinuation, whether temporary or permanent, was defined based on a break of ≥91 days between prescription issue dates; date of discontinuation was therefore the date of the last prescription before the discontinuation plus 30 days. Permanent discontinuers were classified as patients who met the discontinuation definition and who did not receive any further prescriptions for LABA, LAMA, ICS, or any combination of these treatments during the post-index observational period. Patients who met the discontinuation definition, but later received further prescriptions for their index therapy (or another therapy in the same class) were classified as temporary discontinuers (ie, with a drug hiatus). Patients who initiated a new class of therapy during the post-index observational period were classified as “switchers” if there was no, or minimal (≤30 days), overlap between the index and new therapies, and “augmenters” if there was continued overlap (>30 days) between the index and new therapies.
Statistical analyses
Patient demographics (age, gender, body mass index), comorbidities, and COPD disease characteristics (including symptoms and exacerbations) at baseline, including health care resource utilization (HCRU) in the 12 months prior to and including the index date, were analyzed descriptively and described separately for patients initiating maintenance treatment (Cohort 1) and those escalating to triple therapy (Cohort 2). Baseline characteristics were further stratified by the class of therapy initiated for patients in Cohort 1. In addition, the maintenance therapy class prescribed immediately prior to escalation to triple therapy was described for patients in Cohort 2.
Exacerbations in the pre-index period were identified conservatively based on a prescription for oral/systemic corticosteroids issued on the same day as an antibiotic prescription, or a prescription for oral/systemic corticosteroids or antibiotics issued on the same day as a physician visit with a COPD exacerbation ICD-10 code (J44.0 or J44.1). Only primary care prescriptions issued by GPs and recorded in the database were used to identify exacerbations. Per-patient costs were derived for GP visits (all-cause and COPD-related) and primary care prescriptions for COPD treatments (Supplementary materials) for the 12 months prior to and including the index date.
The first treatment modification (including no modification) occurring during the 18-month post-index observational period was identified for each patient, with the number and proportion of patients experiencing one of the prespecified treatment modifications reported by the cohort, and stratified by index class for patients initiating maintenance treatment (Cohort 1). For patients in both cohorts (initiating maintenance treatment or escalating to triple therapy) who had a switch or augmentation as their first treatment modification, the resulting treatment class after switching/augmenting was described. The mean (SD) and median (interquartile range [IQR]) time to first treatment modification was assessed for each cohort and for each prespecified treatment modification.
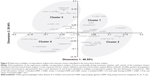
In an exploratory analysis of data for patients initiating maintenance treatment (Cohort 1), we used a segmentation analysis to assess whether specific demographics and clinical characteristics were potential drivers of the choice of initial maintenance therapy. For this segmentation analysis, multiple correspondence analysis (MCA) was performed, followed by hierarchical cluster analysis (HCA) using the Elbow method to identify the optimal number of clusters.27 MCA is a technique used to detect and represent underlying structures in a dataset containing nominal categorical data, whereas HCA is a method used to build the hierarchy of clusters. The final step of the segmentation analysis was to test the statistical association of each variable to its assigned cluster. The variables considered in the segmentation analysis included gender (male/female), age (<50, ≥50 to <60, ≥60 to <70, ≥70 years), vascular comorbidities (ICD-10 codes: I61, I63, I70, I73, I74, I77; yes/no), time interval between the first recorded ICD-10 code for COPD and the index date (0–500/>500 days), record of a blood eosinophils test (yes/no), ischemic and/or cardiac comorbidities (ICD-10 codes: I20, I21, I23, I24, I25, I50; yes/no), exacerbation history in the prior 18 months (0, 1, ≥2), record of a blood neutrophils test (yes/no), and presence of symptoms (yes/no). Presence of symptoms was defined as abnormal sputum (ICD-10 code: R09.3) or atopy (ICD-10 codes: L20.8, L20.9) or cough (ICD-10 code: R05) or fatigue (ICD-10 code: R53) or shortness of breath (ICD-10 code: R06.0) or wheezing (ICD-10 code: R06.2).
A further exploratory analysis of initial maintenance treatment choice used logistic regression models to assess factors associated with the prescription of one COPD therapy over another, in particular LABA vs LAMA, LABA + ICS vs LAMA, and triple therapy vs dual therapy (ie, LAMA + LABA, LAMA + ICS, or LABA + ICS). Potential factors included in these models as covariates were abnormal sputum (yes/no), age, atopy (yes/no), cardiovascular comorbidities (yes/no), cough (yes/no), time interval between the first recorded ICD-10 code for COPD and the index date (years), fatigue (yes/no), diabetes (identified using free text research; yes/no), gastroesophageal reflux disease (GERD [ICD-10 code: K21]; yes/no), gender, ischemic and/or cardiac comorbidities (yes/no), exacerbation history (count in the prior 18 months), shortness of breath (yes/no), and wheezing (yes/no). Selection of covariates was prespecified and based on the literature, clinical knowledge, advice from a French respiratory clinician, and availability of variables with the database. For each covariate, the OR, P-value, and 95% CI were reported.
All statistical analyses were performed using SAS® 9.2 software or a later version (SAS Institute Inc, Cary, NC, USA) via SAS Enterprise Guide version 6.1.
Results
Participants
Of 61,986 individuals with an ICD-10 diagnosis code of COPD in the database, 5,065 patients initiated LABD-based therapy and were eligible for inclusion in Cohort 1. Cohort 2 included 501 individuals who escalated to triple therapy from an existing maintenance therapy (Figure 2). Patient demographics and baseline characteristics for both cohorts, as well as HCRU 12 months prior to and including the index date, are shown in Table 1. Overall, compared with patients initiating maintenance treatment (Cohort 1), patients escalating to triple therapy (Cohort 2) tended to be older, with a longer time between the first recorded ICD-10 code for COPD and index date and a higher number of both all-cause and COPD-related GP visits in the 12 months prior to and including the index date (Table 1).
Treatment pathways for patients initiating maintenance treatment (Cohort 1)
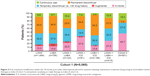
In Cohort 1, LABA + ICS was the most commonly initiated therapy (n=2,196, 43.4%) followed by LAMA alone (n=1,494, 29.5%). Triple therapy was an initial maintenance therapy in 415 (8.2%) patients while LAMA + LABA and LAMA + ICS were the least common therapy classes initiated (n=123, 2.4% and n=81, 1.6%, respectively) (Table 1). Overall, 7.0% of patients initiating maintenance treatment were continuous users for the full 18-month post-index observational period. LAMA + LABA initiators had the highest proportion of continuous use (15.4%), while the proportion was lowest for LABA + ICS therapy (3.9%) (Figure 3). Nearly half (46.5%) of the patients initiating maintenance treatment had a permanent discontinuation, meaning they had no further maintenance therapy prescriptions from their GP for the remainder of the post-index observational period, with a mean (SD) time to discontinuation of 9.5 (11.2) weeks (median [IQR]: 4.3 [4.3–11.1] weeks). Permanent discontinuation was lowest in patients initiated on LAMA + LABA dual-bronchodilator therapy with or without ICS (27.5% and 23.6%, respectively; Figure 3). The proportion of patients discontinuing temporarily (ie, with drug hiatus) was 28.5% overall, ranging from 18.5% (LAMA + ICS) to 35.8% (LAMA + LABA); these patients discontinued treatment after a mean (SD) of 12.6 (13.0) weeks (median [IQR]: 4.3 [4.3–16.3] weeks). Overall, 2.8% of patients initiating maintenance treatment augmented their LABD-based therapy with a similar proportion augmenting from LAMA to triple therapy (55.4%) and from LABA to LABA + ICS (56.0%). The proportion of patients switching to another class of therapy was also low (15.2% overall) with switching highest for LAMA + ICS, triple therapy, and LAMA + LABA (Figure 3). Of the patients switching therapy, those initiating on triple therapy mostly switched to LAMA or LABA + ICS, while those initiating on LAMA + LABA therapy mostly switched to either LABA, LAMA, or LABA + ICS (Figure 4).
Potential drivers of choice of treatment initiated in patients initiating maintenance treatment (Cohort 1)
The factors identified in the segmentation analysis as being potentially associated with the choice of initial maintenance treatment are presented in Table S2. The HCA defined four clusters: cluster 1 included LAMA + LABA, cluster 2 included LAMA and LABA, cluster 3 included LAMA + ICS and triple therapy, and cluster 4 included LABA + ICS (Figure 5). Initiation of LABA and LAMA (independently) was associated with an interval of 0 days between the first recorded COPD ICD-10 code and the index date, a test for eosinophils or for neutrophils having been performed, age of <50 or ≥50 to <60 years, and the presence of vascular comorbidities. Initiation of LABA + LAMA was associated with male gender and a lack of exacerbations. Initiation of LAMA + LABA + ICS and LAMA + ICS (independently) was associated with a time between the first recorded COPD ICD-10 code and the index date of 0–500 days, the presence of ischemic and cardiac comorbidities, and age ≥70 years. Initiation of LABA + ICS was associated with female gender and a history of ≥1 moderate exacerbation, an interval of ≥500 days between the first recorded COPD ICD-10 code and the index date, and the presence of COPD symptoms.
In the series of logistic regression models, the presence of diabetes or shortness of breath increased the odds of initiating LABA over LAMA, whereas the presence of abnormal sputum or ischemic and/or cardiac comorbidities decreased the odds of initiating LABA over LAMA (Table S3). When comparing initiation of LABA + ICS vs LAMA, GERD was associated with initiation of LAMA over LABA + ICS, whereas older age, longer interval between the first recorded COPD ICD-10 code and the index date, cough, female gender, and increase in number of exacerbations in the pre-index period were associated with initiation of LABA + ICS over LAMA (Table S3). The factors associated with the initiation of triple therapy over any dual therapy (LAMA + LABA, LAMA + ICS, or LABA + ICS) were cough, fatigue, female gender, and longer time interval between first recorded COPD ICD-10 code and the index date. Presence of abnormal sputum, ischemic and/or cardiac comorbidities, and shortness of breath were associated with initiation of dual therapy over triple therapy (Table S3).
Treatment pathways for patients escalating to triple therapy (Cohort 2)
Patients in Cohort 2 predominantly escalated to triple therapy from LABA + ICS (53.1%) and LAMA (33.5%). The proportions of patients escalating to triple therapy directly from LAMA + LABA, LABA, and LAMA + ICS were low (7.6%, 3.4%, and 2.4%, respectively). During the 18-month post-index observational period, 18.2% of patients escalating to triple therapy were continuous users and 7.2% discontinued treatment permanently (Figure 3). The mean (SD) time to permanent discontinuation was 20.3 (19.3) weeks (median [IQR]: 12.9 [4.3–36.6] weeks). The proportion of patients who temporarily discontinued (ie, with drug hiatus) was 27.9% and these patients discontinued after a mean (SD) of 21.2 (17.3) weeks (median [IQR]: 16.6 [4.3–30.9] weeks). Nearly half (46.7%) of the patients escalating to triple therapy at index switched therapy, with a comparable likelihood of switching to LABA + ICS or LAMA (Figure 4).
Discussion
We evaluated COPD treatment patterns in two cohorts of patients in the French general practice setting: those who initiated LABD-based therapy and those who escalated to triple therapy. Among patients initiating maintenance treatment for COPD, LABA + ICS was the most commonly initiated LABD-based therapy, prescribed to over 40% of patients, followed by LAMA and LABA monotherapies which were prescribed to ~30% and 15% of patients, respectively. Less than 10% of patients were prescribed triple therapy or LAMA + LABA as their initial maintenance therapy. Given that patients were indexed prior to the launch of fixed-dose combination LAMA/LABA therapy, the low level of LAMA + LABA initiation was not unexpected. It is also interesting to note that a small proportion of patients (<2%) initiated LAMA + ICS combination therapy, which is not currently recommended for the treatment of COPD in France.
These treatment pattern data show that very few patients new to maintenance therapy continuously use their initially prescribed medication over time, and the median time to discontinuation of 4.3 weeks suggests that many patients receive only a single prescription. We also observed that permanent treatment discontinuation in the cohort of patients initiating maintenance treatment (Cohort 1) was high, observed in almost half of the patients, and that switching to another class of COPD therapy or augmentation of the initial regimen was not common, leaving a large proportion of patients without maintenance therapy after the initial prescription. Previous studies have also shown low persistence to COPD treatments, ranging from 19% to 37% over 1 year and from 14% to 25% over 2 years.28–32 However, comparison is difficult owing to differences in COPD populations and health care settings. We did note that ~30% of our study population resumed their initial LABD-based therapy after a gap of at least 91 days (temporary discontinuers [ie, with drug hiatus]) possibly indicating that symptom control was insufficient without the use of long-acting medications or may be related to seasonal or infrequent symptoms. In contrast, among the cohort that escalated to a triple therapy, permanent discontinuation within the 18-month post-index period was much lower (<10% of patients), which may reflect their more frequent interaction with their GPs. We did observe switching therapy in this cohort however, with nearly half of the patients de-escalating to a monotherapy or dual therapy (mostly ICS + LABA or LAMA), suggesting that physicians may be using triple therapy as a temporary or occasional treatment choice to manage symptoms or exacerbations. Low patient adherence to maintenance therapy has been associated with poor health outcomes in patients with COPD, including worsening of symptoms, increased risk of exacerbations and hospitalization, and higher mortality rates.33–35 Although we did not capture reasons for treatment discontinuation in this study, there may be some patients who would be at risk of their disease worsening because of discontinuation of prescription by their GP. However, it is possible that patients who were classified as permanent or temporary discontinuers received further treatment from a specialist, an event that would not be captured in our study using a GP database.
Previous studies have shown that COPD treatment is not always prescribed according to recommendations, possibly reflecting the complexity of COPD management and/or a misunderstanding of the recommendations.36–39 For example, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) report recommends that treatment initiation and escalation should be driven by patients’ exacerbation history and the presence of symptoms, such as dyspnea.1 However, our exploratory analyses observed that these factors did not appear to consistently drive treatment choice; instead, other variables including age and comorbidities seemed to guide prescriptions for COPD medications more often. This finding suggests that the assessment of dyspnea, a cardinal symptom of COPD, may not be well integrated into daily practice, perhaps owing to the difficulty for GPs to clinically appreciate this primary indicator. Other observational studies identified comorbid asthma, high exacerbation rates, airflow obstruction, and comorbidities as determinants of initial maintenance therapy,40 whereas a retrospective database study in UK primary care reported only a minor role of exacerbations in treatment modifications (switching or augmenting maintenance therapy).24 In addition, ~50% of patients who started an initial maintenance treatment with LABD therapy in our study did so in combination with ICS. This finding, in a population of patients with “pure” COPD (with patients identified by ICD-10 codes and exclusion of patients with asthma and other diagnoses incompatible with a COPD diagnosis), indicates a lack of physician adherence to the GOLD report and national guidelines, which recommend that use of ICS in combination with bronchodilators should be limited to patients with repeated exacerbations, or after failure of treatment with LABD monotherapy.1,23 Overall, the observations from the current study indicate an opportunity for improving physician concordance to guidelines, which has also been observed in other studies, including the real-world COLIBRI-COPD cohort study in France.36–39,41,42 These findings may be of value to GPs in understanding how their prescribing patterns measure up to the official guidelines and may improve awareness of the current recommendations. It is also important to note that the introduction of new therapies, such as single-inhaler dual and triple therapies, may change guidelines and treatment patterns going forward, and updated guidelines may provide a better indication of which medications are appropriate for which patient types. Together, these findings suggest a need for better education about COPD and treatment guidelines for GPs.39,41
For patients in Cohort 2 who escalated to triple therapy at index, and then switched from triple therapy to dual therapy or monotherapy (de-escalation) in the 18-month post-index observational period, the consequences, in terms of symptoms and exacerbations, are uncertain owing to the limited evidence investigating de-escalation strategies.1 Based on the evidence from the DACCORD study,43,44 de-escalation from triple therapy is likely not to have negatively impacted disease outcomes in these patients at low risk of exacerbation. The baseline demographic characteristics of the patients who escalated to triple therapy at index also provided interesting insights. Compared with patients initiating maintenance COPD therapy, these patients were on average older and were more likely to experience symptoms such as shortness of breath, cough, and abnormal sputum. They also had a greater number of both all-cause and COPD-related GP visits, which is likely to be related to the increased disease severity and/or comorbidities in this patient subgroup. Greater disease severity has been shown to be associated with increased persistence to therapy in COPD, which could explain the low levels of discontinuation in the cohort of patients who escalated to triple therapy at index.29
Limitations
As with all observational studies, our study has limitations and should be interpreted with these in mind. First, the IQVIA Longitudinal Patient Database captures only prescriptions issued by a GP. Therefore, the analysis only partially captured treatment pathways and estimates of discontinuation may therefore be artificially high, as subsequent prescriptions issued by specialists outside of primary care would not be captured. Conversely, because the database contains no information as to whether a prescription was redeemed, our estimates of continuous prescribing may overestimate true use. Similarly, we may not have identified true initiation or true treatment escalation if these occurred outside of primary care. This is a particularly significant limitation as a recently published study conducted using a French claims database and with similar inclusion criteria to the study presented here found that 36.7% of patients with COPD consulted with a specialist or were seen by a hospital practitioner during the year of follow-up.45 Second, the database does not include spirometry information. FEV1 was measured in only 1.1% of patients, meaning that patients could not be classified by GOLD stage, which would have helped to understand disease severity of patients at baseline and perhaps would have provided additional insight to explore further the rationale for treatment choice. Had these data been available, it would be of interest to formally assess adherence to GOLD and national guidelines that were in place at the time of study (ie, pre-2017 GOLD when FEV1 was recommended as a guide for treatment decision). In addition, the lack of spirometry data in this study means that we are unable to confirm whether the patients had spirometry-confirmed COPD; however, diagnoses of COPD based on ICD codes as used here have been shown to have generally good specificity, sensitivity, and positive predictive value for diagnoses of COPD based on clinical evidence in real-world studies (even in the absence of criteria excluding patients under a certain age or those with diagnoses of asthma or other diseases incompatible with COPD).46–48 Third, no published studies have evaluated the extent to which the physicians included in the IQVIA Longitudinal Patient Database are representative of the French physician population; it is possible that physicians who willingly participate in the panel differ from the general physician population. Finally, the exploratory analyses could account only for observed factors and were based on possibly incomplete information on exacerbations, symptoms, comorbidities, and disease burden. In particular, in this analysis, exacerbations were identified using primary care-based prescriptions and therefore exacerbations treated outside of primary care were not captured, including more severe exacerbations that required emergency department visit or hospitalization. In addition, unreported exacerbations would not be captured. Therefore, exacerbations may have been underestimated and could have been more prominent treatment drivers than what is observed here.
Conclusion
Study findings highlight high discontinuation rates, including extended hiatus periods in treatment cover, among initiators of LABD-based therapy, with much lower discontinuation rates in patients escalating to triple therapy. Exploratory analyses identified that exacerbations and symptoms appeared not to be consistent drivers of the choice of initial therapy and other parameters also played a significant role. This analysis of prescribing patterns revealed a diversity of treatment options and treatment patterns in France and indicates that COPD management choices do not always seem to follow GOLD or national recommendations, particularly regarding how exacerbation history and symptoms should guide treatment choice, as well as the use of ICS in combination with LABDs as initial maintenance therapy.
Availability of data and material
The data that support the findings of this study are available from IQVIA, but restrictions apply to the availability of these data, which were used under license for the current study and so are not publicly available. To request access to patient-level data and documents for this study, please submit an enquiry via www.clinicalstudydatarequest.com.
Acknowledgments
Editorial support (in the form of writing assistance, including development of the initial draft based on author direction, assembling tables and figures, collating authors’ comments, grammatical editing, and referencing) was provided by Chrystelle Rasamison of Fishawack Indicia Ltd, UK. This study was funded by GSK (GSK study HO-15-16099). The funders of the study had a role in study design, data analysis, data interpretation, and writing of the report. The corresponding author had the final responsibility to submit this work for publication. Study conduct and data analysis were performed by Adelphi Real World and IQVIA, and it was funded by GSK. IQVIA were holders of the data; Adelphi Real World and GSK authors had access to the aggregated outputs provided by IQVIA. No funding was provided to the employees of Adelphi Real World or IQVIA for manuscript development.
Author contributions
RJ, RW, TH, and JD were involved in the conception and design of the study, the acquisition of data, and the data analysis and interpretation. ASI, SHL, and GB were involved in the conception and design of the study, and the data analysis and interpretation. WM, CCDS, GN, and BA were involved in the data analysis and interpretation, and YP was involved in the conception and design of the study and the acquisition of data. All authors contributed to drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
WM, CCDS, GN, YP, SHL, and ASI are employees of GSK and own stocks/shares. ASI is also an unpaid faculty member at McMaster University, Hamilton, ON, Canada. RW, RJ, and TH are employees of Adelphi Real World, and GB and JD are employees of IQVIA who were contracted by GSK to conduct the study. BA has received consultant fees and/or research funds from Boehringer Ingelheim, GSK, Chiesi, Astra Zeneca, Pierre Fabre, and Roche. The authors report no other conflicts of interest in this work.
References
Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease. Updated 2018. Available from: https://goldcopd.org/wp-content/uploads/2017/11/GOLD-2018-v6.0-FINAL-revised-20-Nov_WMS.pdf. Accessed November 21, 2018. | ||
GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–1210. | ||
World Health Organization [webpage on the Internet]. Chronic respiratory diseases. Burden of COPD. Available from: http://www.who.int/respiratory/copd/burden/en/. Accessed October 27, 2017. | ||
Laurendeau C, Chouaid C, Roche N, Terrioux P, Gourmelen J, Detournay B. Prise en charge et coûts de la bronchopneumopathie chronique obstructive en France en 2011. [Management and costs of chronic pulmonary obstructive disease in France in 2011]. Rev Mal Respir. 2015;32(7):682–691. French. | ||
Bateman ED, Ferguson GT, Barnes N, et al. Dual bronchodilation with QVA149 versus single bronchodilator therapy: the SHINE study. Eur Respir J. 2013;42(6):1484–1494. | ||
Buhl R, Maltais F, Abrahams R, et al. Tiotropium and olodaterol fixed-dose combination versus mono-components in COPD (GOLD 2–4). Eur Respir J. 2015;45(4):969–979. | ||
Decramer M, Anzueto A, Kerwin E, et al. Efficacy and safety of umeclidinium plus vilanterol versus tiotropium, vilanterol, or umeclidinium monotherapies over 24 weeks in patients with chronic obstructive pulmonary disease: results from two multicentre, blinded, randomised controlled trials. Lancet Respir Med. 2014;2(6):472–486. | ||
Maleki-Yazdi MR, Kaelin T, Richard N, Zvarich M, Church A. Efficacy and safety of umeclidinium/vilanterol 62.5/25 mcg and tiotropium 18 mcg in chronic obstructive pulmonary disease: results of a 24-week, randomized, controlled trial. Respir Med. 2014;108(12):1752–1760. | ||
Oba Y, Sarva ST, Dias S. Efficacy and safety of long-acting β-agonist/long-acting muscarinic antagonist combinations in COPD: a network meta-analysis. Thorax. 2016;71(1):15–25. | ||
Singh D, Ferguson GT, Bolitschek J, et al. Tiotropium + olodaterol shows clinically meaningful improvements in quality of life. Respir Med. 2015;109(10):1312–1319. | ||
Wedzicha JA, Decramer M, Ficker JH, et al. Analysis of chronic obstructive pulmonary disease exacerbations with the dual bronchodilator QVA149 compared with glycopyrronium and tiotropium (SPARK): a randomised, double-blind, parallel-group study. Lancet Respir Med. 2013;1(3):199–209. | ||
Zuwallack R, Allen L, Hernandez G, Ting N, Abrahams R. Efficacy and safety of combining olodaterol Respimat(®) and tiotropium HandiHaler(®) in patients with COPD: results of two randomized, double-blind, active-controlled studies. Int J Chron Obstruct Pulmon Dis. 2014;9:1133–1144. | ||
Fabbri LM, Roversi S, Beghé B. Triple therapy for symptomatic patients with COPD. Lancet. 2017;389(10082):1864–1865. | ||
Lee TA, Wilke C, Joo M, et al. Outcomes associated with tiotropium use in patients with chronic obstructive pulmonary disease. Arch Intern Med. 2009;169(15):1403–1410. | ||
Lipson DA, Barnacle H, Birk R, et al. FULFIL Trial: Once-Daily Triple Therapy for Patients with Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2017;196(4):438–446. | ||
Lipson DA, Barnhart F, Brealey N, et al. Once-Daily Single-Inhaler Triple versus Dual Therapy in Patients with COPD. N Engl J Med. 2018;378(18):1671–1680. | ||
Rojas-Reyes MX, Garcia Morales OM, Dennis RJ, Karner C. Combination inhaled steroid and long-acting beta(2)-agonist in addition to tiotropium versus tiotropium or combination alone for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2016;(6):CD008532. | ||
Singh D, Brooks J, Hagan G, Cahn A, O’Connor BJ. Superiority of “triple” therapy with salmeterol/fluticasone propionate and tiotropium bromide versus individual components in moderate to severe COPD. Thorax. 2008;63(7):592–598. | ||
Singh D, Papi A, Corradi M, et al. Single inhaler triple therapy versus inhaled corticosteroid plus long-acting β2-agonist therapy for chronic obstructive pulmonary disease (TRILOGY): a double-blind, parallel group, randomised controlled trial. Lancet. 2016;388(10048):963–973. | ||
Tabberer M, Lomas DA, Birk R, et al. Once-daily triple therapy in patients with COPD: patient-reported symptoms and quality of life. Adv Ther. 2018;35(1):56–71. | ||
Vestbo J, Papi A, Corradi M, et al. Single inhaler extrafine triple therapy versus long-acting muscarinic antagonist therapy for chronic obstructive pulmonary disease (TRINITY): a double-blind, parallel group, randomised controlled trial. Lancet. 2017;389(10082):1919–1929. | ||
Société de Pneumologie de Langue Francaise (SPLF). Traitement pharmacologique de la BPCO. [Pharmacological treatment of COPD]. Rev Mal Respir. 2010;21(S1):S19–S35. French. | ||
Zysman M, Chabot F, Devillier P, et al. Pharmacological treatment optimization for stable chronic obstructive pulmonary disease. Proposals from the Société de Pneumologie de Langue Française. Rev Mal Respir. 2016;33(10):911–936. | ||
Landis SH, Wurst K, Le HV, Bonar K, Punekar YS. Can assessment of disease burden prior to changes in initial COPD maintenance treatment provide insight into remaining unmet needs? a retrospective database study in UK primary care. COPD. 2017;14(1):80–85. | ||
ISPE. Guidelines for good pharmacoepidemiology practices (GPP). Pharmacoepidemiol Drug Saf. 2008;17(2):200–208. | ||
von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. | ||
Everitt BS. Cluster Analysis. 3rd ed. London: Edward Arnold Publishers; 1993. | ||
Breekveldt-Postma NS, Koerselman J, Erkens JA, Lammers JW, Herings RM. Enhanced persistence with tiotropium compared with other respiratory drugs in COPD. Respir Med. 2007;101(7):1398–1405. | ||
Cramer JA, Bradley-Kennedy C, Scalera A. Treatment persistence and compliance with medications for chronic obstructive pulmonary disease. Can Respir J. 2007;14(1):25–29. | ||
Penning-van Beest F, van Herk-Sukel M, Gale R, Lammers JW, Herings R. Three-year dispensing patterns with long-acting inhaled drugs in COPD: a database analysis. Respir Med. 2011;105(2):259–265. | ||
Wurst KE, Punekar YS, Shukla A. Treatment evolution after COPD diagnosis in the UK primary care setting. PLoS One. 2014;9(9):e105296. | ||
Wurst KE, St Laurent S, Mullerova H, Davis KJ. Characteristics of patients with COPD newly prescribed a long-acting bronchodilator: a retrospective cohort study. Int J Chron Obstruct Pulmon Dis. 2014;9:1021–1031. | ||
Belleudi V, di Martino M, Cascini S, et al. The impact of adherence to inhaled drugs on 5-year survival in COPD patients: a time dependent approach. Pharmacoepidemiol Drug Saf. 2016;25(11):1295–1304. | ||
Montes de Oca M, Menezes A, Wehrmeister FC, et al. Adherence to inhaled therapies of COPD patients from seven Latin American countries: The LASSYC study. PLoS One. 2017;12(11):e0186777. | ||
Simoni-Wastila L, Wei YJ, Qian J, et al. Association of chronic obstructive pulmonary disease maintenance medication adherence with all-cause hospitalization and spending in a Medicare population. Am J Geriatr Pharmacother. 2012;10(3):201–210. | ||
Jochmann A, Neubauer F, Miedinger D, Schafroth S, Tamm M, Leuppi JD. General practitioner’s adherence to the COPD GOLD guidelines: baseline data of the Swiss COPD Cohort Study. Swiss Med Wkly. 2010;140. | ||
Perez X, Wisnivesky JP, Lurslurchachai L, Kleinman LC, Kronish IM. Barriers to adherence to COPD guidelines among primary care providers. Respir Med. 2012;106(3):374–381. | ||
Price D, West D, Brusselle G, et al. Management of COPD in the UK primary-care setting: an analysis of real-life prescribing patterns. Int J Chron Obstruct Pulmon Dis. 2014;9:889–904. | ||
Salinas GD, Williamson JC, Kalhan R, et al. Barriers to adherence to chronic obstructive pulmonary disease guidelines by primary care physicians. Int J Chron Obstruct Pulmon Dis. 2011;6:171–179. | ||
Gruffydd-Jones K, Brusselle G, Jones R, et al. Changes in initial COPD treatment choice over time and factors influencing prescribing decisions in UK primary care: in UK primary care: a real-world, retrospective, observational. NPJ Prim Care Respir Med. 2016;26:16002. | ||
Aisanov Z, Bai C, Bauerle O, et al. Primary care physician perceptions on the diagnosis and management of chronic obstructive pulmonary disease in diverse regions of the world. Int J Chron Obstruct Pulmon Dis. 2012;7:271–282. | ||
Kelkel E, Herengt F, Ben Saidane H, et al. COLIBRI: Improving clinical practice and producing relevant scientific data. Rev Mal Respir. 2016;33(1):5–16. | ||
Buhl R, Criée CP, Kardos P, et al. A year in the life of German patients with COPD: the DACCORD observational study. Int J Chron Obstruct Pulmon Dis. 2016;11:1639–1646. | ||
Vogelmeier C, Worth H, Buhl R, et al. “Real-life” inhaled corticosteroid withdrawal in COPD: a subgroup analysis of DACCORD. Int J Chron Obstruct Pulmon Dis. 2017;12:487–494. | ||
Valentini F, Devouassoux G, Belhassen M. Caractéristiques des patients BPCO initiant un traitement de fond en France: une analyse EGB [Characteristics of COPD patients initiating a long-term therapy in France: an EGB analysis]. Congrès de Pneumologie de Langue Française (CPLF). Rev Mal Respir. 2018;35(Suppl):A10. French. | ||
Kurmi OP, Vaucher J, Xiao D, et al. Validity of COPD diagnoses reported through nationwide health insurance systems in the People’s Republic of China. Int J Chron Obstruct Pulmon Dis. 2016;11:419–430. | ||
Cooke CR, Joo MJ, Anderson SM, et al. The validity of using ICD-9 codes and pharmacy records to identify patients with chronic obstructive pulmonary disease. BMC Health Serv Res. 2011;11:37. | ||
Thomsen RW, Lange P, Hellquist B, et al. Validity and underrecording of diagnosis of COPD in the Danish National Patient Registry. Respir Med. 2011;105(7):1063–1068. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.