Back to Journals » Open Access Emergency Medicine » Volume 12
Continuing Education for Prehospital Healthcare Providers in India – A Novel Course and Concept
Authors Lindquist BD , Koval KW , Acker PC , Bills CB , Khan A, Zachariah S, Newberry JA, Rao GR, Mahadevan SV, Strehlow MC
Received 14 February 2020
Accepted for publication 6 August 2020
Published 17 September 2020 Volume 2020:12 Pages 201—210
DOI https://doi.org/10.2147/OAEM.S249447
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Balakrishnan Nair
Benjamin D Lindquist,1 Kathryn W Koval,2 Peter C Acker,1 Corey B Bills,1,3 Ayesha Khan,1 Sybil Zachariah,1 Jennifer A Newberry,1 GV Ramana Rao,4 Swaminatha V Mahadevan,1 Matthew C Strehlow1
1Department of Emergency Medicine, Stanford University School of Medicine, Palo Alto, CA 94304, USA; 2Department of Emergency Medicine, Medical University of South Carolina, Charleston, SC 29425, USA; 3University of California San Francisco, San Francisco, CA 94143, USA; 4GVK Emergency Management and Research Institute, Secunderabad, Telangana 500078, India
Correspondence: Benjamin D Lindquist Email [email protected]
Background: Emergency medical services (EMS) in India face enormous challenges in providing care to a geographically expansive and diverse patient population. Over the last decade, the public–private-partnership GVK EMRI (Emergency Management and Research Institute) has trained over 100,000 emergency medical technicians (EMTs), with greater than 21,000 currently practicing, to address this critical gap in the healthcare workforce. With the rapid development and expansion of EMS, certain aspects of specialty development have lagged behind, including continuing education requirements. To date, there have been no substantial continuing education EMT skills and training efforts. We report lessons learned during development and implementation of a continuing education course (CEC) for EMTs in India.
Methods: From 2014 to 2017, we employed an iterative process to design and launch a novel CEC focused on five core emergency competency areas (medicine and cardiology, obstetrics, trauma, pediatrics, and leadership and communication). Indian EMT instructors and providers partnered in design and content, and instructors were trained to independently deliver the CEC. Many challenges had to be overcome: scale (> 21,000 EMTs), standardization (highly variable skill levels among providers and instructors), culture (educational emphasis on rote memorization rather than practical application), and translation (22 major languages and a few hundred local dialects spoken nationwide).
Lessons Learned: During the assessment and development phases, we identified five key strategies for success: (1) use icon-based video instruction to ensure consistent quality and allow voice-over for easy translation; (2) incorporate workbooks during didactic videos and (3) employ low-cost simulation and case discussions to emphasize active learning; (4) focus on non-technical skills; (5) integrate a formal training-of-trainers prior to delivery of materials.
Conclusion: These key strategies can be combined with innovation and flexibility to address unique challenges of language, system resources, and cultural differences when developing impactful continuing educational initiatives in bourgeoning prehospital care systems in low- and middle-income countries.
Keywords: prehospital care, emergency medical services, prehospital education, continuing medical education
Background
Growing Global Need for Emergency Medical Services
Lack of timely prehospital care is a critical factor affecting the wellbeing of populations in low- and middle-income countries (LMICs). Emergency medical services (EMS) have been shown to improve patient outcomes in many conditions from obstetric emergencies to traumatic injuries.1–4 A robust EMS system in LMICs with well-trained emergency medical technicians (EMTs) makes life-saving interventions available to populations in the field and transportation to facilities that were previously out of reach. EMS can serve an important role in driving forward key components of the United Nation’s Sustainable Development Goal (SDG) 3, including 3.6: to halve the number of death and injuries from road traffic accidents by 2020.5
EMS in India
In the 1980s and 90s, the prehospital landscape in India was dotted with sporadic private hospital ambulance services. Patient transports were typically between health facilities, rather than from field to facility, and the majority of ambulance providers had no formal training. The cost of accessing and using ambulance services was prohibitive for the average person, especially those in rural communities where the majority of India’s population resides. Due to such financial constraints, local agencies arose to provide prehospital emergency services at no or low-cost.6 Yet, the grassroots nature of these efforts prevented coordination among prehospital care organizations as well as with police and fire services. This disjointed system also lacked standardization.6 The heterogeneity of ambulance services meant different emergency access phone numbers and variable vehicle response. Trust in a consistent EMS response arose as a major concern. In 1984, the Centralized Accidents and Trauma Service was established by the Delhi Government with the toll-free number 102 to address many of these challenges. Yet despite attempts at expansion throughout the country, this service disbanded.7
Into this void stepped the public-private-partnership Emergency Management and Research Institute (EMRI, later GVK EMRI). Launched in August 2005, GVK EMRI began with a single emergency access phone number (108), a centralized call center, and 14 ambulances in the state of Andhra Pradesh. The mission was to provide free access to prehospital EMS for all people in India. Since its inception in 2005, the organization has rapidly grown and now caters primarily to the poor with 85–90% of the beneficiaries living below the poverty level for India (<972–1407 Rs. per capita ~$22/month).8 The service is operational in 15 states and two union territories. Nationwide, GVK EMRI responds to more than 23,000 emergencies daily and boasts a staff of 21,000 EMTs and more than 7000 ambulances. Covering more than 75% of India’s population, it is the largest ambulance system in the world. Further, an additional 8 states are now covered through other centralized EMS providers, meaning that of India’s 29 states, 23 are now serviced by centrally coordinated EMS services.
Each GVK EMRI ambulance is staffed with one basic EMT and one pilot (driver). Currently, EMTs receive 450 hours, or 52 days, of theory and skills training prior to working on the ambulance. For comparison, EMTs in the US require at least 120 hours of training, though with a more limited scope of practice. Despite the longer initial training hours for GVK EMRI EMTs, it is challenging to cover the breadth of relevant emergency care topics during the initial training and even more challenging to prevent attrition of knowledge and skills over time.9,10
EMS Education in LMICs and India
The World Health Organization considers educational accreditation and continuing education to be standard practice for prehospital systems.11 Unfortunately, in contrast to high-income-countries, continuing education or recertification is not typically a requirement in LMICs, even where an EMS governing body exists. Upon review of LMIC ambulance services (including Ghana, Malaysia, Iran, Ethiopia, Zimbabwe, and South Africa), none appear to have robust continuing medical education requirements or established continuing medical education (CME) programs in place.12–18
CME has been shown to be effective for retention of knowledge and skills and in changing behavior in clinical practice.19,20 Like other LMICs, EMS in India is not yet regulated by any centralized governing authority. As a result, prehospital education requirements and training quality are highly variable.6 This includes initial training with more than six different certification levels. Financing and delivering continuing education pose unique challenges, particularly to underfinanced and understaffed entities in LMICs. Excusing employees from their duties to engage in CME courses can place strain on workforces. Further, educational materials, including asynchronous or on-line courses, in native languages are lacking.
Given this need, GVK EMRI and Stanford Emergency Medicine International (SEMI) developed a targeted, standardized, iterative, 5-part continuing education course (CEC), to refresh Indian EMT knowledge and skills. Here we describe the creation and implementation of the CEC program and the many lessons learned.
Setting
India is the second most populous country in the world with 1.32 billion people, spread across 29 states and 7 union territories. Seventy percent of the population lives in rural areas with poor infrastructure. Over the last decade, India has moved from the World Bank’s low-income country category to low-middle-income. With a burgeoning economy, India has made strides in improving key health indicators including infant mortality, under-five mortality, and the incidence of HIV/AIDS. Less progress has been made in combating malaria, though the country is poised to continue addressing these important determinants of health with institution of the SDGs.5,21,22 Many health challenges remain, particularly the rapid rise of non-communicable diseases such as cardiovascular disease and traumatic injury.23
Methods
CEC Topic Selection
Core competency areas to be covered by CECs were identified through prior institutional quality assurance research, focused interviews with local educators, ambulance observations and international guidelines.24 Local EMS experts, EMT instructors and EMTs were interviewed to identify gaps in EMT performance that would benefit from focused educational efforts. From these interviews and observations, the emergency topics chosen for the five CECs were medicine and cardiology, obstetrics, trauma, pediatrics, and leadership and communication. The rationale behind the selection of each topic is discussed below. The timeline for course development is shown in Figure 1.
 |
Figure 1 Timeline of CEC development and delivery. |
Medicine and Cardiology
The impact of non-communicable diseases (NCDs) has increased drastically in India. This group of ailments now accounts for over two thirds of total morbidity and well over half of all deaths in the country, with cardiovascular disease accounting for over a quarter of all deaths.25 For many NCDs, timely access to key interventions can drastically improve outcomes, thereby highlighting the potential beneficial impact of quality prehospital care. Consequently, the initial course was designed to address common medical complaints and reinforce the initial approach to the critically ill patient.
Obstetrics
Obstetric emergencies are the most common reason patients call for a GVK EMRI ambulance.26 In some Indian states, up to 30% of all prehospital calls are for obstetric complaints, many related to normal labor or complications in the third trimester of pregnancy.26 The aim of the obstetric CEC was to train EMTs to manage high-risk scenarios related to both maternal and neonatal care in the prehospital setting. This included a sustained focus on the second and third stages of childbirth, as a significant percentage of pregnant women who call for EMS services will deliver prior to ambulance arrival or during transport to healthcare facilities.27
Trauma
Injury is the second most common chief complaint encountered by EMTs—a trauma-related death occurs in India every 1.9 minutes.28 The absence of integrated trauma care systems, including prehospital care, contributes to the high death and disability rates from injury.29 Trauma is also specifically mentioned in the third goal of the SDGs, further highlighting injury as an essential subject matter.5 The aim of the trauma CEC was to standardize the approach to the trauma patient, utilizing trauma life support algorithms, with an emphasis on early recognition of primary survey injuries and rapid intervention to reduce preventable deaths. Focus on communication with the call center in these high-risk scenarios was also emphasized.
Pediatrics
Twenty percent of worldwide deaths in children under five years of age occur in India.30 Due to time constraints during the GVK EMRI foundational EMT training programs, limited time is allocated for pediatric didactics. Approximately two days of the 52-day curriculum focus on pediatric advanced life support. This approach is not unique to India but mirrors EMT-basic and -paramedic training in the United States, where 8/110 hours and 15/1000 hours are dedicated to pediatric topics, respectively.31 However, due to the substantial number of deaths in children under five in India, more in-depth pediatric and neonatal training is imperative. Therefore, the aims of this CEC were to strengthen EMT knowledge of pediatric complaints, increase their comfort with pediatric medication dosing, and improve their overall confidence with managing pediatric patients.
Leadership & Communication
A common theme that emerged from our faculty’s prior educational interventions for healthcare providers in LMICs was the need for improved leadership and communication skills. Aside from communication with patients, family members, physicians and hospital staff, EMTs are often tasked with coordinating care for multiple victims and leading community outreach events. As a result, the final program focused on nontechnical or “soft” skills. Course design was based on a literature review of EMT communication and leadership skills across various countries.32–36
Training Material Development
Each CEC followed a similar design and implementation pathway (Figure 2). First, emergency medicine faculty from SEMI completed a needs assessment by conducting ambulance ride-alongs and focused interviews with organizational leaders, EMT instructors and the EMTs themselves. Needs assessments incorporated concepts of “asset mapping” to identify local strengths including technological capabilities, instructor skills, and learning center resources.37,38 Following the needs assessment, a pilot program was developed by SEMI faculty and delivered over two or three days to a cohort of EMTs and EMT instructors. Both structured and unstructured feedback was obtained during pilot courses, adjustments were made, and a finalized course was produced.
 |
Figure 2 Three-staged process of CEC development. |
For the initial two CECs, medical and obstetric emergencies, Indian instructors participated in final program delivery by assisting SEMI faculty with course delivery. However, they did not receive a separate training of trainers (TOT) course. To improve instructor confidence and investment into the material, the final three CECs incorporated a separate TOT course. This TOT included specific lectures on teaching techniques and dedicated practice time for leading case discussions and simulations. After the two-day TOT, local instructors were observed teaching the course to EMTs and were provided individualized feedback by SEMI instructors and their Indian peers.
The vehicle for core content delivery also evolved during the program. The initial course utilized lecture slides, while the second added audio recordings from SEMI instructors to slides. The final three courses utilized an animation-based software program (powtoon.com) to create videos using icons instead of text to ease translation.39 Voice recordings for the videos were created using the open-access program Audacity (sourceforge.net/projects/audacity/). To encourage participation, the EMTs were given printed workbooks, as each of the instructional videos contained “built-in” pauses, that prompted EMTs to answer workbook questions on high-yield learning points. Lecture content was reinforced with standardized, facilitated case discussions and skills work stations using simulated patients. EMTs or low-fidelity manikins served as patients, while other EMTs were tasked with serving as the medical provider at various stages of the patient care process (ie, primary survey, secondary survey, interventions, etc.).
To evaluate the immediate effectiveness and feasibility of this program, we chose to assess knowledge gain of the participants. EMTs and instructors were given multiple choice question exams prior to and immediately after each individual course. Questions were evaluated for content validity and quality by SEMI faculty prior to each course and assessed for cultural appropriateness during each pilot course. An equal number of questions were developed for each section to assess strengths and weaknesses in comprehension and curriculum. Questions were translated into the predominant local languages and trialed during the pilot programs.
Training Material Deployment
Medical and Cardiology CEC
The course was co-led by SEMI faculty and a group of the EMT trainers. Demographics are provided in Table 1. Twenty-eight total topics were presented in this module (Table 2). The final course was delivered to 50 EMTs in Hyderabad.
 |
Table 1 Demographics of Participants by CEC |
 |
Table 2 Core Didactics of Medical and Cardiovascular Emergencies CEC |
Obstetric CEC
In total, 18 core obstetric lectures were selected to cover high-yield topics related to the care of mother and newborn in the ambulance. This material was supplemented and reinforced through 11 supporting simulation scenarios and three case-based discussions (Table 3).
 |
Table 3 Core Didactics of Obstetric CEC |
Simulation efforts were taken to create realistic patient encounters. To enhance learning, a low-cost birthing simulator was developed for the course, using entirely locally sourced materials.40
The course was delivered in four Indian states: Telangana and Gujarat in January and Karnataka and Himachal Pradesh in May 2015. In sum, 160 individuals participated in the 2-day course (Table 1).
Trauma CEC
The trauma CEC focused on early prevention of death and disability from trauma (Table 4). Secondary aims included reviewing skills for trauma management and reinforcing the application of prehospital trauma care protocols.41
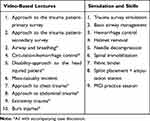 |
Table 4 Core Didactics of Trauma CEC |
In total, 27 instructors were trained on the material and then delivered the content to a total of 118 EMTs in Telangana and Gujarat with coaching and mentorship from SEMI faculty (Table 1).
Pediatric CEC
The pediatric CEC comprised an almost identical format to the trauma course. Since simulation was well received during the trauma CEC, extra emphasis was placed on simulation during the Pediatric CEC to emphasize key concepts that could be applied during real-world clinical scenarios. Based on EMT feedback from the pilot program, content was added for drowning, hypothermia, and overdose (Table 5). More time was allotted to pediatric medication dosing practice during the final program. Pediatric resuscitation video lectures had two different formats, determined by the local availability of automated external defibrillators (AEDs) in the ambulances.
 |
Table 5 Core Didactics of Pediatric CEC |
The final TOT was delivered to 34 EMT instructors from nine states. These providers then delivered the course to 133 EMTs with guidance and feedback from SEMI instructors (Table 1).
Leadership and Communication CEC
This final CEC had two tracks of focused content: leadership and communication (Table 6). The leadership track reinforced the idea of EMTs as leaders in the field. Interactive sessions incorporated practice setting goals, professional reflections, and stress relief.
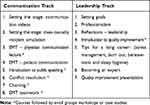 |
Table 6 Core Didactics of Leadership and Communication CEC |
The communication track focused on strengthening the communication between EMTs and their patients, the other members of their team, and physicians. These sessions highlighted the concepts of empathy, reflective listening, and public speaking skills. EMT-to-physician communication was emphasized as EMTs often receive online medical direction from physicians at a centralized call center; thus, communication with physicians must be clear, concise, and accurate. A standardized tool designed for ambulance to emergency department hand-offs, IMIST-AMBO, was adapted and taught to the EMTs to facilitate thorough and organized handovers to physicians and other healthcare providers following patient transport.35,36
The concept of quality improvement was also introduced during this CEC. Small groups of students were encouraged to develop and present their own quality improvement project ideas. This exercise allowed the EMTs to synthesize multiple aspects of the leadership and communication course, including (1) empowering EMTs as leaders to recognize their experiential expertise with regard to their own country’s EMS system; (2) developing a reflective practice; (3) practicing public speaking and communication skills; and, (4) advancing professionalism. The exercise was thoroughly embraced by the participants, and a couple of notable quality improvement project ideas emerged from this exercise, including the use of call center data to identify regional hot spots to guide the repositioning of ambulances.
The final course was delivered in Hyderabad, India, to 34 instructors from 8 states in April 2017 (Table 1). Over the next 2 days, these instructors then taught 63 EMTs.
Lessons Learned
Without formal credentialing and CME requirements, ensuring that Indian EMTs maintain their knowledge and technical skills over time is challenging and uncertain. To address this need, we employed an iterative process to design and launch novel continuing education courses (CECs) focused on five core prehospital care competency areas. The 3-step model of needs assessment, pilot, and training-of-trainers was critical to the success of this program. Throughout the entire process, buy-in from key stakeholders was essential to design an effective instructional program that would be embraced and utilized for years to come. Below, we discuss invaluable lessons learned throughout the implementation process that led to significant evolution of the program between each individual CEC course.
First, we adapted the presentation medium to better meet the needs of our partner organization and the EMTs as learners. As discussed, the initial courses utilized traditional lecture slides, the next iteration progressed to using video recordings of lecture slides, and the final format employed animation with audio voice over.39 The intention for using animation was threefold. Similar to pre-recorded slide sets, the animation-based lectures ensured consistency of the core content for each of the potential 21,000 EMTs taking the course. Additionally, animation-based lectures, using icons with minimal text, made it easier to translate the lectures into multiple languages. Finally, the pre-made animated videos allowed local instructors to focus their energy on other aspects of each CEC, such as facilitating group discussions, simulations and procedural skills stations. Ultimately, this technique was well received by EMTs and instructors.
Second, based on observation, as well as formal and informal feedback, pairing workbooks with individual lectures seemed to improve EMT engagement and participation during the final three CECs. By filling out the workbook’s fill-in-the-blanks, tables and diagrams during each video lecture, the EMTs were able to engage with each lesson in a manner that was similar to attending a live interactive lecture.
Third, the time allotted for didactic lectures was reduced, and an intentional emphasis was placed on case discussions, procedural skills stations and simulation. During our pilot programs, we observed that EMT instructors were less familiar with and comfortable leading case discussions and conducting simulation. While global use of simulation for prehospital education has become increasingly mainstream,42 using simulation as an educational modality proved to be a new and challenging skill for the Indian EMT instructors. In general, EMTs were adept at reciting information from lectures; however, they would often forget important steps in medical management when placed in a simulated setting or group case discussion. Hence, the later programs focused on active learning exercises including simulation and case discussions.
Fourth, throughout the course implementation, we gained an appreciation for the importance of enhancing communication and leadership skills amongst EMTs. Through quality assurance research and direct observation, we observed how a lack of training on systematic approaches to communication during EMT foundational training adversely impacted the quality of care provided. These observations prompted the development of the fifth and final course on nontechnical “soft” skills.
Fifth, we also reaffirmed the importance of a formal TOT followed by direct observation, evaluation and feedback for instructors. Initial CECs (medical and obstetric emergencies) included EMT instructors for training and delivery of the courses but did not include a separate TOT designed solely for instructors. The final three courses included a formalized instructor’s manual and devoted two full days of teaching to the instructors with particular focus on new skills, such as moderating case discussions and simulations. The final CECs also evolved to include an extra week where SEMI faculty observed local instructors teaching the EMTs. As a result, the instructors were more invested in the course, as they knew their own performance was being evaluated. This also allowed the Indian instructors to learn teaching techniques from each other and develop increased confidence in the subject matter. We feel this addition was incredibly important for the success of the program and will be an essential component of all future TOT courses.
Finally, as with all global health initiatives, flexibility was paramount. On several occasions, EMT instructors or course participants suggested changes to educational content during piloting of each program. While at times, this meant completely revamping course content, such flexibility allowed all partners to tailor the course to the exact needs of the learners, and in particular, the clinical context in which they work. For example, during the development of the trauma curriculum, plans included utilization of Advanced Trauma Life Support algorithms for initial patient evaluation (eg, ABCDE) as opposed to the International Trauma Life Support protocols the EMTs had previously learned. To reduce confusion and improve instructor support, the curriculum was overhauled to ensure that it more closely mirrored ITLS pathways.
Challenges and Next Steps
Logistically there remain a number of challenging steps to course dissemination. Translation into the local language continues to remain a time-intensive and costly endeavor. At this time, only one CEC has been translated into Hindi, India’s national language. While GVK EMRI has adhered to an organization-wide policy regarding mandatory CME requirements, such requirements may be viewed as extra time and expense by state governments who are tasked with ensuring completion of training programs. Currently, a few CECs are being delivered in the states of Gujarat, Uttarkhand, and Meghalaya. Moving forward, EMTs in all states will be excused from clinical duties to complete a required two-day CEC every six months. GVK EMRI plans for broad dissemination of the CECs beginning in the near future, in collaboration with state leadership.
We plan to assess knowledge gain and practice-improvement when the courses are delivered by Indian trainers in the local language. Ideally, improvement in EMT medical practice could be measured through an ongoing GVK EMRI-SEMI quality assurance initiative, which evaluates EMT performance metrics for the most common chief complaints seen by GVK EMRI’s ambulance service. Further details about this novel quality assurance effort are available elsewhere.26
Finally, we often found it difficult to encourage female instructors and EMTs to participate in the courses. As the demographic data from each course reveals, attendees were predominantly male, reflective of the employee rosters at GVK EMRI and to our understanding, the profession in India as a whole.
Conclusions
Lifelong learning is imperative to healthcare provider practice. This is the first description of the design and implementation of EMS continuing education courses in LMICs. We identified key lessons that address the unique challenges of language, system resources, and cultural differences found in developing nations. When combined with innovation, flexibility and careful planning, these strategies can guide implementation of continuing education courses for prehospital care providers in developing nations.
Abbreviations
LMIC, low- and middle-income countries; EMS, emergency medical services; EMTs, emergency medical technicians; SDG, sustainable development goal; EMRI, Emergency Management and Research Institute; CME, continuing medical education; SEMI, Stanford Emergency Medicine International; CEC, continuing education course; TOT, training of trainers; NCDs, non-communicable diseases; AEDs, automated external defibrillators.
Ethical Approval
Not applicable.
We would like to acknowledge the Indian EMTs and EMT instructors for their participation in the educational programs and their tireless effort to provide expeditious emergency care to their patients.
Author Contributions
All authors participated in designing the course, developing the educational curriculum, delivering the course content, executing the project and drafting the manuscript. All authors contributed significantly to the writing of manuscript, including all revisions. All authors have agreed on this journal for publication. All authors approved the final version to be published, and take responsibility for the contents of this article.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Murad MK, Larsen S, Husum H. Prehospital trauma care reduces mortality. Ten-year results from a time-cohort and trauma audit study in Iraq. Scand J Trauma Resusc Emerg Med. 2012;20(1):1–10. doi:10.1186/1757-7241-20-13
2. Mock CN, Jurkovich GJ. nii-Amon-Kotei D, Arreola-Risa C, Maier R V. Trauma mortality patterns in three nations at different economic levels: implications for global trauma system development. J Trauma. 1998;44(5):804. doi:10.1097/00005373-199805000-00011
3. Henry JA, Reingold AL. Prehospital trauma systems reduce mortality in developing countries. J Trauma Acute Care Surg. 2012;73(1):261–268. doi:10.1097/TA.0b013e31824bde1e
4. Tayler-Smith K, Zachariah R, Manzi M, et al. An ambulance referral network improves access to emergency obstetric and neonatal care in a district of rural Burundi with high maternal mortality. Trop Med Int Heal. 2013;18(8):993–1001. doi:10.1111/tmi.12121
5. World Health Organization. World Health Statistics- Monitoring Health for the SDGs. Geneva, Switzerland; 2016.
6. Sharma M, Brandler ES. Emergency medical services in India: the present and future. Prehosp Disaster Med. 2014;29(3):307–310. doi:10.1017/S1049023X14000296
7. Subhan I, Jain A. Emergency care in India: the building blocks. Int J Emerg Med. 2010;3(4):207–211. doi:10.1007/s12245-010-0223-7
8. Report of the expert group to review the methodology for measurement of poverty. 2014. Available from: http://planningcommission.nic.in/reports/genrep/pov_rep0707.pdf.
9. Strehlow M, Newberry J, Bills C, et al. Characteristics and outcomes of women utilizing emergency medical services for third-trimester pregnancy-related complaints in India: a prospective observational study. BMJ Open. 2016;2016.
10. Mahadevan S, Strehlow M, Newberry J, Bills C, Pirrotta E, Rao SJ Seizure 2013: a summary report by Stanford Emergency Medicine International for GVK Emergency Management Research Institute. 2015.
11. World Health Organization. Prehospital Trauma Care Systems. Geneva, Switzerland; 2005.
12. Martel J, Oteng R, N-K M-M, et al. The development of sustainable emergency care in Ghana: physician, nursing and prehospital care training initiatives. J Emerg Med. 2014;47(4):462–468.
13. Hisamuddin NA, Hamzah MSHC. Prehospital emergency medical services in Malaysia. J Emerg Med. 2007;32(4):415–421. doi:10.1016/j.jemermed.2006.08.021
14. Far AS, Zargar M. Mohammad Reza Kalantar Motamedi S, Karbakhsh M, Mohammad Ghodsi S,et al. Trauma care system in Iran. Chin J Traumatol. 2011;14(143):131–136.
15. Pozner CN, Bayleygne TM, Davis MA, Benin-Goren O, Noble VE, Halpern P. Emergency medical services capacities in the developing world: preliminary evaluation and training in Addis Ababa, Ethiopia. Prehosp Emerg Care. 2003;7(3):392–396. doi:10.1080/10903120390936635
16. Azazh A, Teklu S, Woldetsadi A, et al. Emergency medicine and its development in Ethiopia with emphasis on the role of Addis Ababe University, School of Medicine, Emergency Medicine Department. Ethiop Med J. (Supp 2):2014.
17. MacFarlane C. van Loggerenberg CKW. International EMS systems: South Africa—past, present and future. Resuscitation. 2005;64(2):145–148. doi:10.1016/j.resuscitation.2004.11.003
18. Thomson N. Emergency medical services in Zimbabwe. Resuscitation. 2005;65(1):15–19. doi:10.1016/j.resuscitation.2005.01.008
19. Marinopoulos SS, Dorman T, Ratanawongsa N, et al. Effectiveness of continuing medical education: evidence report/technology assessment, no. 149. Evid Rep Technol Assess. 2007;149:1–69.
20. De Lorenzo RA, Abbott C. Effect of a focused and directed continuing education program on prehospital skill maintenance in key resuscitation areas. J Emerg Med. 2007;33(3):293–297. doi:10.1016/j.jemermed.2007.02.060
21. United Nations. India and the MDGs Towards a Sustainable Future for All; 2015.
22. The World Bank. Maternal mortality ratio (modeled estimate, per 100,000 live births). 2015. Available from: http://data.worldbank.org/indicator/SH.STA.MMRT.
23. WHO. India: WHO statistical profile. 2012. Available from:http://www.who.int/gho/countries/ind.pdf.
24. Mercer MP, S V M, Pirrotta E, et al. Epidemiology of shortness of breath in prehospital patients in Andhra Pradesh, India. J Emerg Med. 2015;49(4):448–454. doi:10.1016/j.jemermed.2015.02.041
25. World Health Organization. WHO country cooperation strategies and briefs: India. Available from: http://www.who.int/country-cooperation/what-who-does/strategies-and-briefs/en/?ua.1. Accessed
26. Strehlow MC, Newberry JA, Bills CB, et al. Characteristics and outcomes of women using emergency medical services for third-trimester pregnancy-related problems in India: a prospective observational study. BMJ Open. 2016;6(7):e011459. doi:10.1136/bmjopen-2016-011459
27. Bills CB, Newberry JA, Darmstadt G, et al. Reducing early infant mortality in India: results of a prospective cohort of pregnant women using emergency medical services. BMJ Open. 2018;8(4):e019937. doi:10.1136/bmjopen-2017-019937
28. Joshipura MK. Trauma care in India: current scenario. World J Surg. 2008;32(8):1613–1617. doi:10.1007/s00268-008-9634-5
29. Wesson HKH, Kwong M. Trauma care in India: a review of the literature. Surgery. 2017;S0039-6060(17):30093–30094.
30. Wang H, Liddell CA, Coates MM, et al. Global, regional, and national levels of neonatal, infant, and under-5 mortality during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9947):957–979. doi:10.1016/S0140-6736(14)60497-9
31. Ngo TL, Belli K, Shah MI. EMSC program manager survey on education of prehospital providers. Prehosp Emerg Care. 2014;18(3):424–428. doi:10.3109/10903127.2013.869641
32. Iedema R, Ball C, Daly B, et al. Design and trial of a new ambulance-to-emergency department handover protocol: “IMIST-AMBO”. BMJ Qual Saf. 2012;21(8):627–633. doi:10.1136/bmjqs-2011-000766
33. Shah Y, Alinier G, Pillay Y. Clinical handover between paramedics and emergency department staff: SBAR and IMIST-AMBO acronyms. Int Paramed Pract. 2016;6(2):37–44. doi:10.12968/ippr.2016.6.2.37
34. Tavares W, Bowles R, Donelon B. Informing a Canadian paramedic profile: framing concepts, roles and crosscutting themes. BMC Health Serv Res. 2016:16.
35. Mercer D, Haddon A, Loughlin C. Leading on the edge: the nature of paramedic leadership at the front line of care. Health Care Manage Rev. 2016.
36. Shields A, Flin R. Paramedics’ non-technical skills: a literature review. Emerg Med J. 2013;30(5):350–354. doi:10.1136/emermed-2012-201422
37. Weiner SG, Totten VY, Jacquet GA, et al. Effective teaching and feedback skills for international emergency medicine “train the trainers” programs. J Emerg Med. 2013;45(5):718–725. doi:10.1016/j.jemermed.2013.04.040
38. Morgan A, Ziglio E, Davies M, eds. Health Assets in a Global Context. Verlag New York: Springer; 2010.
39. Powtoon. 2017. powtoon.com.
40. Dennison T, Bills C, Acker P, Mahadevan S Development of a low cost, low-fidelity birthing model for EMS instruction in India. Manuscript In Progress
41. Roy N, Veetil DK, Khajanchi MU, et al. Learning from 2523 trauma deaths in India- opportunities to prevent in-hospital deaths. BMC Health Serv Res. 2017;17(1):142. doi:10.1186/s12913-017-2085-7
42. Abelsson A, Rystedt I, Suserud B-O LL. Mapping the use of simulation in prehospital care – a literature review. Scand J Trauma Resusc Emerg Med. 2014;22(1):22. doi:10.1186/1757-7241-22-22
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
