Back to Journals » International Medical Case Reports Journal » Volume 11
Congenital infiltrating lipomatosis of the face with hyperplastic mandibular, maxillary and pterygoid bones: case report and a review of literature
Authors Asafu Adjaye Frimpong G , Aboagye E, Amamoo M, Obiri-Yeboah S , Tettey Olesu J
Received 9 May 2018
Accepted for publication 10 July 2018
Published 18 September 2018 Volume 2018:11 Pages 233—238
DOI https://doi.org/10.2147/IMCRJ.S172735
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas

George Asafu Adjaye Frimpong,1,2 Evans Aboagye,2,3 Mansa Amamoo,4 Solomon Obiri-Yeboah,5 Jonathan Tettey Olesu6
1Department of Radiology, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana; 2Spectra Health Imaging and Interventional Radiology, Kumasi, Ghana; 3Department of Molecular Medicine, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana; 4Department of Radiology, Komfo Anokye Teaching Hospital, Kumasi, Ghana; 5Department of Oral and Maxillofacial Sciences, Kwame Nkrumah University of Science and Technology Dental School, Kumasi, Ghana; 6Department of Oral and Maxillofacial Surgery, Komfo Anokye Teaching Hospital, Kumasi, Ghana
Abstract: Congenital infiltrating lipomatosis of the face (CILF) is a rare lipomatous lesion, commonly seen in childhood, and it is characterized by collections of mature, unencapsulated adipose tissues that infiltrate facial soft and hard tissues. The lesion is seen as an overgrowth of bone and soft tissue and is generally present clinically as slow-growing painless masses. In this case report, we described one case of CILF, which is one of the first cases reported in Ghana and Africa as a whole, along with a literature review on the diagnosis and current treatment strategies.
Keywords: congenital infiltrating lipomatosis of face, facial asymmetry analysis, hemifacial hyperplasia, macrodontism
Introduction
Congenital infiltrating lipomatosis of the face (CILF) is a very rare lipomatous lesion with <60 reported cases in literature.1–3 CILF is nonhereditary and usually seen in childhood, causing unilateral facial skeletal hyperplasia, and it is histologically characterized by collections of mature, unencapsulated adipose tissues that infiltrate facial soft and hard tissues.1,4–7 The primary concern in CILF is usually esthetics and the high rate of recurrence after surgical excision, as patients present with normal psychomotor development, and there is no sex predilection.7,8 In this case report, we present an additional case of CILF, which is one of the first cases reported in Ghana and Africa as a whole, along with a discussion on the diagnosis and treatment of CILF, with the aim of providing information toward the management of this rare condition.
Case report
A 9-year-old male patient presented with a painless right facial swelling, which had been present since birth and had progressively been increasing in size. Examination revealed facial asymmetry with a right hemifacial swelling spanning from the lower border of the right mandible to the inferior right lower eyelid measuring ~10×15 cm. There was enlargement of the right ear and a bulge on the right parietal scalp. The lesion was soft, non-tender and mobile with hyperpigmentation of the postauricular skin. There was deviation of the lip and nose to the left with obliteration of the right nasolabial sulcus indicating a right facial palsy. Oral examination revealed right-sided lip and tongue enlargement, right palatal bulge, right-sided dental anarchy with anterior open bite and calculus deposition.
Computed tomography (CT) of the head region showed a large lipomatous transformation of the right side of the face, involving the subcutaneous layer and the right parotid gland, with extension into the right masticator space. The tragus of the right ear also showed lipomatous infiltration. The lesion covered an area of ~13.8×8.5 cm. Evidence of significant hyperplasia of the right mandible was found with the width of the body of the mandible been 1.9 cm, while the contralateral side had a width of up to 0.9 cm. The lateral plate of the right pterygoid bone was also significantly hyperplastic, having a width of up to 0.9 cm compared to 0.2 cm of the contralateral side. The right maxilla was also significantly hyperplastic with a width of up to 2 cm compared to 1 cm on the contralateral side. There was also asymmetry of the face with disorganized dentition on the right side. No other asymmetric parts of the body were involved.
Written informed consent was obtained from the parent to have the case details and accompanying images published.
Discussion
Congenital infiltrating lipomatosis rarely affects the face and has been reported to have a predilection for the trunk and extremities.9 The term congenital infiltrating lipomatosis of the face was initially proposed by Slavin et al,7 who were the pioneers to report on proliferating and infiltrating lesions of lipocytes that involved only the facial region. The main characteristics of CILF elucidated by Slavin et al included: 1) nonencapsulated tumors containing mature lipocytes; 2) fat infiltration of adjacent muscles and soft tissues; 3) absence of malignant characteristics; 4) absence of lipoblasts; 5) presence of fibrous elements and increased number of nerve bundles and vessels and 6) adjacent bone hypertrophy. CILF is classified under lipoma, and it is distinguished from liposarcoma by the absence of mitosis, lipoblastic proliferation and pleomorphism.7 In CILF, mature lipocytes invade into adjacent tissues in the facial region, manifesting as hypertrophy of both hard and soft structures on the affected side of the face and usually presenting clinically as slow-growing painless masses.1,4–7 The manifestation is always unilateral, and reported cases that described the site of the facial mass have shown that ~64% occur on the left.10 In CILF patients who present for treatment at the adult stage, the condition progresses with gradual hyperplasia, while there is extensive hyperplasia in childhood patients (≤1 year of age).11
Several studies have traced the etiology of CILF to postzygotic mutation, as pluripotent cells of embryonic origin are known to precipitate somatic defect under the influence of trauma, muscle metaplasia, hormones and irradiation.12–16 This triggers and accelerates the lipomatous change seen in CILF. The postzygotic mutation occurs in the PIK3CA gene in the affected tissues, as PI3K, which is encoded by PIK3CA, plays a critical role in regulating cell survival, motility, adhesion and proliferation.17 A study done by Maclellan et al17 showed that subcutaneous adipose tissue from affected areas of patients with CILF contains somatic activating mutations in PIK3CA. A further study that sought to determine if the overgrowth in subjects with CILF was caused by a postzygotic mutation in only the subcutaneous adipose tissue (one tissue type) or by the presence of mutant cells in each of the subject’s overgrown tissues also reported that all tissues (including stroma, adipose, muscle, bone, nerves, etc.) on the side of the face affected with CILF contained PIK3CA mutations.18
It must however be noted that the same postzygotic mutations have been identified in vascular malformations, cancers and other disorders with overgrowth, collectively termed together with CILF as PIK3CA-related overgrowth spectrum (PROS), hence not surprising that several mosaic disorders are in the differential diagnosis of CILF.19 Conditions like Parry–Romberg syndrome (progressive hemifacial hyperplasia atrophy) and hemifacial microsomia, which cause contralateral hypoplasia, need to be considered.20 In addition, although hemifacial hyperplasia does not involve mucosal neuromas and mature lipocytic infiltration, it shares common features with CILF and must be noted.19,20 In conditions like facial angioma and angiolipoma, cutaneous capillary brush implicated in some patients with CILF has also been found.21,22 Lymphangioma has also been associated with diffuse swelling in the facial and neck area, although this is easily resolved with an MRI scan.20,22 Encephalocraniocutaneous lipomatosis (ECCL) and proteus syndrome also have infiltrating lipomatosis as a feature. However, CILF unlike proteus syndrome usually presents at birth and does not involve areas outside the head and neck region. ECCL on the other hand manifests in the central nervous system in contrast to CILF.22 Well-differentiated liposarcoma and lipoblastomatosis that involve fat tissue infiltration also need to be ruled out. Liposarcoma is associated with the presence of lipoblastic proliferation and large number of cell mitosis and pleomorphism, with lipoblastomatosis having the presence of fetal adipose tissue, which is absent in the histopathological examination of CILF tissue.7,22–24 Facial location, congenital presentation, early eruption of deciduous and permanent teeth, macrodontism, adjacent dentoskeletal manifestations, proliferation of parotid gland on the affected side, macroglossia and specific histological features are possible results for CILF.7,23,25–27
The diagnosis of CILF in our case was based on the patient’s medical records, clinicopathological manifestations and imaging features from CT (Figures 1–5). The CT scan was particularly useful in demonstrating the lipomatous nature of mass, osseous changes and their exact anatomic location and relationship to surrounding structures prior to surgery. Diagnosis of CILF was however confirmed by histopathology. The lesion was histologically characterized by sheets or lobules of mature normal adipocytes infiltrating trabecular bone, muscle fibers and salivary glands.28,29
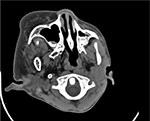  | Figure 1 Lipomatous infiltration of the right side of the face, including the parotid gland and masticator space. |
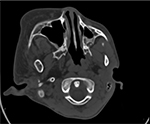  | Figure 2 CT scan showing the enlarged pterygoid. Abbreviation: CT, computed tomography. |
  | Figure 4 CT scan showing the enlarged maxilla. Abbreviation: CT, computed tomography. |
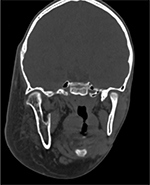  | Figure 3 CT scan showing the enlarged right mandible. Abbreviation: CT, computed tomography. |
  | Figure 5 Volume rendering technique showing radiolucent fat and facial deformity. |
Bone changes reported in CILF cases include hypertrophy of the skull, hypertrophy of the zygomatic bone, cervical vertebrae, acceleration of dentoskeletal growth, hemimandibular hypertrophy and sclerosis.30–33 These changes in bone appear to be associated with periosteal irritation associated with the overlying mass, regional malformation of mesenchyme affecting bone and soft tissues or increased vascularity.30,33,34 Li et al35 in their review of 59 reported cases of CILF noted that the bony asymmetry appears to increase with age, with the adipose tissue infiltrating into surrounding tissues and causing pterygoid gland and muscles (such as pterygoid plate and massetter and temporalis muscles) involvement, as reported in our cases.
The major concern in the treatment of CILF is the high rate of recurrence after surgical excision although the tumor is benign, with a recent study reporting as high as 79% rate of recurrence.1,8,35 As a result, multiple surgeries are needed for cosmetic reasons, and when necessary, osseous reduction operations of the maxilla and mandible are performed.21,35,36 Based on the esthetic requirement of the patient, a multidisciplinary approach that involves surgeons, clinicians, dentists, psychologists and geneticists may be ideal.22,29,37 The high rate of recurrence may be the result of incomplete resection, as these fatty lesions are histologically benign, and as such, the value of aggressive extirpation needs to be weighed against the facial nerve damage and the likelihood of the resultant deformity.38
Tracy et al in 2013 reported a conservative approach involving targeted chemotherapy and surgical resection in the management of CILF. The use of celecoxib and imatinib in personalized targeted chemotherapy was associated with improved facial symmetry without evidence of disease progression, thus paving the way for the exploration of this synergistic approach toward the management of this rare condition.41 Conservative approach has also been reinforced by several authors on the backdrop of the benign nature and critical location of CILF despite the associated high rate of recurrences.23,28,39
A recent study in 2017 by Kalantary et al40 proposed a new multistep surgical approach toward the management of CILF. This involves initial debulking to correct the soft tissue asymmetry, followed by orthognathic surgery to correct the skeletal asymmetry, dental problems and associated malocclusion, cautioning however that each patient needs to be evaluated for this additional surgery on the bony level before carrying out this step, and finally bimaxillary procedure and genioplasty. The surgery was successfully performed when the patient was 14 years (after puberty), with no record of clinical recurrence at the time of publication (patient was 18 years then).
In addition, considering the implication of PIK3CA gene mutation in the pathogenic theory of CILF, inhibitors of PI3K, which are currently been used in clinical trials involving cancer patients, may play a role in CILF patients.17 PI3K inhibitors may therefore be tested for CILF patients in clinical trials in the near future.35
An area of contention in the treatment of CILF is the timing of surgical excision. Slavin et al7 in their earlier studies encouraged early aggressive surgery in a bid to improve facial appearance and control the overgrowth. Van Wingerden et al41 disagreed with this approach on the basis of possible risk to nerve, which is compounded by multiple procedures and the likelihood of recurrence. They however admitted that the postponement of surgery may make the procedure more extensive, along with associated psychosocial issues. They further argued that the delay in surgery lowers the chances of damaging the facial nerve, may require fewer procedures and there will be more mature contralateral cheek for comparison during the procedure. Padwa and Mulliken21 also sided with Van Wingerden et al, observing that growth hormone most probably has a role in recurrences and that any effort to reduce the mass before the end of adolescence is bound to fail due to recurrences. Based on our study, we advocate that extensive resection should be delayed as long as possible, with due consideration to psychosocial issues. Elevation of the ptotic upper lip, liposuction and the excision of mucosal neuromas are among the temporary measures that can be taken to improve asymmetry in young patients with minimal risk.21
Conclusion
CILF is a rare congenital disorder, histologically characterized by sheets or lobules of mature normal adipocytes infiltrating trabecular bone, muscle fibers and salivary glands. The proximity of vital anatomic structures and the diffuse nature of the disease pose a greater challenge to surgical resection. In this article, we reported an additional case of CILF and did an extensive review of the diagnosis and treatment of the condition, providing information toward the management of this rare disorder.
Disclosure
The authors report no conflicts of interest in this work
References
Rajeswaran R, Murthy J, Chandrasekharan A, Joseph S. Case Report: Congenital infiltrating lipomatosis of face. Indian J Radiol Imaging. 2008;18(4):306. | ||
Kamal D, Breton P, Bouletreau P. Congenital infiltrating lipomatosis of the face: Report of three cases and review of the literature. J Craniomaxillofac Surg. 2010;38(8):610–614. | ||
Urs AB, Augustine J, Kumar P, Arora S, Aggarwal N, Sultana N. Infiltrating lipomatosis of the face: A case series. J Nat Sci Biol Med. 2013;4(1):252–257. | ||
Enzinger FM, Weiss SW. Benign lipomatous tumors. In: Soft Tissue Tumors. Vol. 199. St Louis, MO: CV Mosby; 1983. | ||
Keramidas T, Lagogiannis G, Vlachou V, Katsikeris N. Congenital infiltrating lipomatosis of the face with associated involvement of the TMJ structures. Case report and review of the literature. J Craniomaxillofac Surg. 2012;40(8):750–7566. | ||
Flores-Sarnat L. Congenital infiltrating lipomatosis of the face: recognition and pathogenesis. Neuropediatrics. 2012;43(06):346–348. | ||
Slavin SA, Baker DC, Mccarthy JG, Mufarrij A. Congenital infiltrating lipomatosis of the face: clinicopathologic evaluation and treatment. Plast Reconstr Surg. 1983;72(2):158–164. | ||
Heymans O, Ronsmans C. Congenital infiltrating lipomatosis of the face. Eur J Plast Surg. 2005;28(3):186–189. | ||
Scherl MP, Som PM, Biller HF, Shah K. Recurrent infiltrating lipoma of the head and neck. Case report and literature review. Arch Otolaryngol Head Neck Surg. 1986;112(11):1210–1212. | ||
Li Y, Chang G, Si L, et al. Congenital Infiltrating Lipomatosis of the Face: Case Report and Literature Review. Ann Plast Surg. 2018;80(1):83. | ||
Kang N, Ross D, Harrison D. Unilateral hypertrophy of the face associated with infiltrating lipomatosis. J Oral Maxillofac Surg. 1998;56(7):885–887. | ||
Görken C, Alper M, Bilkay U, Çelik N, Songür E. Congenital infiltrating lipomatosis of the face. J Craniofac Surg. 1999;10(4):365–368. | ||
Haloi AK, Ditchfield M, Penington A, Phillips R. Facial infiltrative lipomatosis. Pediatr Radiol. 2006;36(11):1159–1162. | ||
Chen CM, Lo LJ, Wong HF. Congenital infiltrating lipomatosis of the face: case report and literature review. Chang Gung Med J. 2002;25(3):194–200. | ||
Donati L, Candiani P, Grappolini S, Klinger M, Signorini M. Congenital infiltrating lipomatosis of the face related to cytomegalovirus infection. Br J Plast Surg. 1990;43(1):124–126. | ||
Patel RV, Gondalia JS. Congenital infiltrating lipomatosis of the face. Br J Plast Surg. 1991;44(2):157–158. | ||
Maclellan RA, Luks VL, Vivero MP, et al. PIK3CA activating mutations in facial infiltrating lipomatosis. Plast Reconstr Surg. 2014;133(1):12e–19e. | ||
Couto JA, Konczyk DJ, Vivero MP, et al. Somatic PIK3CA mutations are present in multiple tissues of facial infiltrating lipomatosis. Pediatr Res. 2017;82(5):850–854. | ||
Keppler-Noreuil KM, Rios JJ, Parker VE, et al. PIK3CA-related overgrowth spectrum (PROS): diagnostic and testing eligibility criteria, differential diagnosis, and evaluation. Am J Med Genet A. 2015;167A(2):287–295. | ||
Kamal D, Breton P, Bouletreau P. Congenital infiltrating lipomatosis of the face: report of three cases and review of the literature. J Craniomaxillofac Surg. 2010;38(8):610–614. | ||
Padwa BL, Mulliken JB. Facial infiltrating lipomatosis. Plast Reconstr Surg. 2001;108(6):1544–1554. | ||
Kim JE, Gottschall JA, Bachman RP, Nemzer L, Puligandla B, Schauer G. Facial infiltrating lipomatosis: physical, radiological, and histopathological findings. Arch Otolaryngol Head Neck Surg. 2010;136(3):301–303. | ||
Malik A, Jagmohan P, Thukral BB, Khanna G, Rajni. Congenital infiltrating lipomatosis of the face and neck. Acta Radiol. 2004;45(5):556–560. | ||
Ünal O, Cirak B, Bekerecioglu M, Kutluhan A, Ugraş S, Tali T. Congenital infiltrating lipomatosis of the face with cerebral abnormalities. Eur Radiol. 2000;10(10):1610–1613. | ||
de Rosa G, Cozzolino A, Guarino M, Giardino C. Congenital infiltrating lipomatosis of the face: report of cases and review of the literature. J Oral Maxillofac Surg. 1987;45(10):879–883. | ||
Keramidas T, Lagogiannis G, Vlachou V, Katsikeris N. Congenital infiltrating lipomatosis of the face with associated involvement of the TMJ structures. Case report and review of the literature. J Craniomaxillofac Surg. 2012;40(8):750–756. | ||
Flores-Sarnat L. Congenital infiltrating lipomatosis of the face: recognition and pathogenesis. Neuropediatrics. 2012;43(6):346–348. | ||
Shenoy AR, Nair KK, Lingappa A, Shetty KS. Congenital infiltrating lipomatosis of face: case report and review of literature. J Indian Soc Pedod Prev Dent. 2015;33(2):156. | ||
Pires Fraga MF, Mello D, Jorge D, Perin LF, Helene A, Fraga MF. Congenital infiltrating lipomatosis. J Plast Reconstr Aesthet Surg. 2009;62(12):e561–e564. | ||
Bollinger B. Bone changes in diffuse congenital lipomatosis. Neuroradiology. 1987;29(1):104. | ||
Bouletreau P, Breton P, Freidel M. Congenital infiltrating lipomatosis of the face: case report. J Oral Maxillofac Surg. 2000;58(7):807–810. | ||
Macmillan AR, Oliver AJ, Reade PC, Marshall DR. Regional macrodontia and regional bony enlargement associated with congenital infiltrating lipomatosis of the face presenting as unilateral facial hyperplasia. Brief review and case report. Int J Oral Maxillofac Surg. 1990;19(5):283–286. | ||
Wylie EJ, Kendall B. Cranio-vertebral bony changes in a case of congenital lipomatosis. Neuroradiology. 1989;31(4):352–353. | ||
Lachman RS, Finklestein J, Mehringer CM, Maenza R. Congenital aggressive lipomatosis. Skeletal Radiol. 1983;9(4):248–254. | ||
Li Y, Chang G, Si L, et al. Congenital Infiltrating Lipomatosis of the Face: Case Report and Literature Review. Ann Plast Surg. 2018;80(1):83. | ||
Kang N, Ross D, Harrison D. Unilateral hypertrophy of the face associated with infiltrating lipomatosis. J Oral Maxillofac Surg. 1998;56(7):885–887. | ||
Mahadevappa A, Raghavan VH, Ravishankar S, Manjunath GV. Congenital infiltrating lipomatosis of the face: a case report. Case Rep Pediatr. 2012;2012:1–3. | ||
Ha TV, Kleinman PK, Fraire A, et al. MR imaging of benign fatty tumors in children: report of four cases and review of the literature. Skeletal Radiol. 1994;23(5):361–367. | ||
Tracy JC, Klement GL, Scott AR. Interdisciplinary management of congenital infiltrating lipomatosis. Int J Pediatr Otorhinolaryngol. 2013;77(12):2071–2074. | ||
Kalantary S, van de Casteele E, Nadjmi N. Congenital Infiltrating Lipomatosis of the Face: Case Report With Presentation of a New Multistep Surgical Approach. J Oral Maxillofac Surg. 2018;76(6):1334–1343. | ||
van Wingerden JJ, Erlank JD, Becker JH. Liposuction for congenital infiltrating lipomatosis of the face. Plast Reconstr Surg. 1988;81(6):989. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
