Back to Journals » Risk Management and Healthcare Policy » Volume 14
Configuration Analysis of Influencing Factors of Technical Efficiency Based on DEA and fsQCA: Evidence from China’s Medical and Health Institutions
Authors Li Z , Zhang W, Kong A, Ding Z , Wei H , Guo Y
Received 15 September 2020
Accepted for publication 3 December 2020
Published 8 January 2021 Volume 2021:14 Pages 49—65
DOI https://doi.org/10.2147/RMHP.S282178
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Marco Carotenuto
Zhiguang Li,1 Wanying Zhang,1 Aijie Kong,1 Zhiyuan Ding,1 Hua Wei,1 Yige Guo2
1School of Economics and Management, Anhui University of Chinese Medicine, Hefei, Anhui, People’s Republic of China; 2King’s Business School, King’s College London, London, UK
Correspondence: Hua Wei
School of Economics and Management, Anhui University of Chinese Medicine, 350 Longzihu Road, Xinzhan District, Hefei 230012, People’s Republic of China
Tel +86-551-68129224
Email [email protected]
Purpose: This paper aims to measure the technical efficiency of China’s medical and health institutions from 2012 to 2017 and outline the path to achieve high-quality development.
Methods: The DEA-Malmquist was used to evaluate the total factor productivity of medical and health institutions in 31 provinces. A fuzzy set Qualitative Comparative Analysis (fsQCA) was used for configuration analysis of determinants affecting technical efficiency.
Results: The average total factor productivity (TFP) of those institutions was 0.965, namely TFP declined averagely by 3.5% annually. The efficiency change and the technical change were 0.998 and 0.967, respectively. The realization paths of high technical efficiency are composed of high fatality rate and high financial allocation-led, high population density and high GDP-led. Low dependency ratio and low financial allocation-led, low fatality rate and low financial allocation-led are the main reasons for low technical efficiency.
Conclusion: Due to advanced medical technology and economic development, major cities like Beijing, Shanghai, and Guangdong have attracted a large number of high-level health personnel, achieving long-term and stable health business growth. Hubei, Anhui, and Sichuan also have made rapid development of health care through appropriate financial subsidies and policy supports. The technical changes in Qinghai, Yunnan, and Inner Mongolia are higher than the national average, but the operation and management level of the medical and health institutions is relatively weak. Henan, Jiangxi, and Heilongjiang have a prominent performance in the efficiency change, but the technical change is weaker than the national average.
Keywords: China’s medical and health institutions, DEA-malmquist, fsQCA, efficiency, configuration
Introduction
The national health service system planning outline (2015–2020) points out that China has established a medical and health service system covering urban and rural residents after long-term development. The system is composed of hospitals, primary medical and health institutions and professional public health institutions, etc. However, the shortage of medical and health resources, unreasonable structure and layout, and fragmentation of the service system is still a knotty problem.1 Especially, the COVID-19 outbreak has not only caused a major impact on China’s economic and social sectors, but also posed a major challenge to China’s medical and health system. Thus, under the new circumstance, this paper attempts to review and evaluate the operation of medical and health institutions in China. This study can not only provide a basis for China’s overall reasonable allocation and planning of medical resources, but also provide a reference for the high-quality development of regional health services.
In this case, efficiency measurement becomes an effective way to evaluate the performance of the target configuration in healthcare. In recent years, Data Envelopment Analysis (DEA) has been recognized as one of the most frequent approaches for measuring the efficiency of Decision Making Units (DMUs), such as hospitals. DEA is a multiple-input multiple-output non-parametric evaluation method, which has been proposed by Charnes, Cooper, and Rhodes and then extended by Banker, Charnes, and Cooper as a method to evaluate the performance of homogenous units.2 At present, the DEA method is widely used in the field of healthcare around the world. Scholars evaluate hospital efficiency and propose improvement measures to help governments optimize the allocation of medical and health resources.3–7 It is noteworthy, however, that the current literature on medical and health institutions still lacks a systematic and integrated approach to analyze the influences of the policy and external institutional environment on the operating efficiency, and explain the internal logic and path for the medical and health institutions to achieve the high operating efficiency from the perspective of configuration.
In this paper, the DEA-Malmquist model is used to measure the total factor productivity of medical and health institutions in 31 provinces from 2012 to 2017, and A fuzzy set Qualitative Comparative Analysis (fsQCA) is used to summarize the paths for improving the technical efficiency. This aims to reveal the internal mechanism of the efficient operation of Chinese medical and health institutions and provide empirical and theoretical evidence for the causal complexity. This paper makes two main contributions to the literature. First, to our knowledge, this is the first study that focuses on technical efficiency improvement in medical and health institutions by using fsQCA. Our paper thus verifies the asymmetric view of complexity theory. Second, the combination of antecedent conditions for realizing high and low efficiency of resource allocation of medical and health institutions in China are analyzed by means of fsQCA; thus, our paper makes up for the deficiency of the literature and efficiency methods on the improvement of technical efficiency in medical and health institutions, particularly the specific paths of improving the technical efficiency. The rest of this paper is organized as follows. The following section briefly reviews the literature. Data and Methods will consider both the sources and methods. The fourth section is about the empirical result. In Improvement Scheme of Operation Efficiency of Medical and Health Institutions, we discuss the improvement scheme of the technical efficiency of medical and health institutions. Summary and discussion are arranged in Summary and Discussion.
Literature Review
According to the economic strength and development level, this paper integrates the literature about the DEA method to study hospital efficiency in both high-income countries and low- and middle-income countries. In terms of the research of hospital efficiency in high-income countries, DEA and second-stage regression analysis was commonly used. Thai and Noguchi (2019) argued that better management of patient flow and bed utilization might be expected to improve hospital efficiency during the institutional reform of the English health-care sector.6 Besides, Hunt and Link (2020) used a two-stage semi-parametric DEA to conclude that in areas with high per capita public health expenditure, the efficiency of hospitals can be improved, and medical expenses can be reduced.7 In the study of hospital efficiency in the United States, Miller et al (2017) established an integral-valued non-radial Russell DEA model.8 It solved the non-linear problem of the integer value model by using parametric integer linear programming, directly calculated the efficiency score before and after the medical reform of the Massachusetts Medical Reform Act, and evaluated the reform results. Furthermore, Khushalani and Ozcan (2017) examined the efficiency of producing quality in hospitals between 2009 and 2013 using Dynamic Network DEA and the hospital characteristics that contributed to this efficiency.9 Multinomial logistic regression was performed to determine hospital and market characteristics, and they found urban and teaching hospitals were less likely to improve high-quality production efficiency.
Simultaneously, the DEA method is also widely used in hospital efficiency research in low- and middle-income countries. In previous studies, Samsudin et al (2016) used DEA to determine the efficiency score and Tobit model to identify the possible determinants of inefficiency.10 The results showed that the average daily number of inpatients, the number of outpatients per doctor, and the classification of hospitals affected the efficiency of public hospitals in Malaysia. Additionally, Marrakchi and Essid (2019) hold different opinions on hospital efficiency in Tunisia, an African country. They aimed to assess the technical efficiency of a sample of Tunisian public hospitals using the non-parametric approach of DEA.11 Based on the difference of the regional level, the decision-making process was analyzed, and it was concluded that the most efficient hospitals in Tunisia were in the North East and Center East. Compared with African countries, there were more studies on hospital efficiency in the Middle East, especially in Saudi Arabia and Iran. Omrani, Shafaat and Emrouznejad (2018) proposed an integrated fuzzy clustering cooperative game DEA method to solve the problem of lack of homogeneity among decision-making units.12 The 288 hospitals in 31 provinces of Iran were evaluated successfully. The results show that each province’s characteristics can affect the efficiency of hospitals due to the differences in economic growth, population, and GDP. Also, Aldalbahi et al (2020) discussed how to use the single-stage DEA model to measure the technical efficiency of hospitals in Saudi Arabia.13 They first discussed the applicability of the DEA method in the field of health care in Saudi Arabia and demonstrated that the DEA method was very important in evaluating the efficiency of medical institutions.
Like many countries, there are also some challenges in the development of China’s medical and health institutions. This is exemplified by the uneven distribution of resources and unbalanced regional development. To evaluate the equity and efficiency of maternal and child health (MCH) resources allocation in Hunan Province, Huang et al (2020) used Gini coefficient method and DEA to conclude that the equity of MCH resources by population size is superior by geographic area and the disproportionate distribution of the number of medical equipment and midwives between different regions were the main source of inequity.14 Jia and Yuan (2017) were the first to report the application of DEA window analysis model to assess the operational efficiencies of multi-branched public hospitals in China.15 The purpose of the study was to explore whether the strategy of establishing branch hospitals in Shanghai is correct or not. The results showed that various ways of establishing branched hospitals may lead to the difference in operational efficiencies, and the way of merging and reorganization may have some advantages in efficiency optimization. Guo et al (2018) discussed the efficiency change of the Hong Kong Hospital Authority from 2000 to 2013 and the impact of exogenous factors such as population density on the efficiency of the Hong Kong Hospital Authority.16 The empirical results showed that there are significant differences in the efficiency of different hospitals and clusters, especially when public hospitals serving in rich areas are relatively low.
To sum up, DEA has several advantages that make it a reliable tool in measuring hospital technical efficiency, and the measurement and evaluation is still a major area of interest within the field of efficiency research. However, our study is different from previous studies in the following aspects. Firstly, based on the perspective of complexity theory, this study is the first to use the fsQCA method to explore the actual cause and effect relationship in the efficiency of resource allocation of medical and health institutions. And we summarize the commonness between similar cases and propose an operational path to improve the technical efficiency of Chinese medical and health institutions, which is of great guiding value to the actual government decision-making. Therefore, our focus is on the configuration analysis of external institutional factors of technical efficiency in China’s medical and health institutions.
Data and Methods
Data
Data for this study were obtained from the 2012–2017 “China Health and Family Planning Statistical Yearbook” and “China Statistical Yearbook”. The research objects are medical and health institutions in 31 provinces, autonomous regions, and municipalities (excluding Taiwan, Hong Kong, and Macau).
Methodology
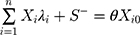
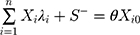
DEA is a non-linear model introduced by Charnesm, Cooper, and Rhodes in 1978. According to the basic principles of DEA, the model set in this paper is as follows. Let us suppose the number of China’s Medical and Health Institutions (MHI) is n, and every DMU has a type of inputs and b type of outputs. a-dimensional vector Xi and b-dimensional vector Yi respectively represent the input and output of the i-th MHI. On the basis of relative efficiency, the slack variable S+, the residual variable S− and non-Archimedean infinitesimal ε are introduced. The CCR model of a MHI based on constant return to scale is as follows.
where, λi≧0, i = 1, 2,..., n; S+≧0, S-≧0. In equation (1), VTE represents technical efficiency; X0 and Y0 respectively represent the input vector and output vector of the MHI i0. The VTE obtained by solving the linear programming is the total operating efficiency. If VTE=1, the MHI is generally efficient; if VTE< 1, the operation for the MHI is inefficient.
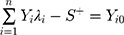
In order to further explore whether the overall operating inefficiency of the MHI is caused by pure technical inefficiency or scale inefficiency, we add a constraint condition to the CCR model and obtain the BCC model based on the assumption of variable scale return.
where, λi≧0, i = 1, 2,..., n; S+≧0, S-≧0. In equation (2), VPTE represents pure technical inefficiency, and technical efficiency is equal to pure technical efficiency times scale efficiency. Therefore, scale efficiency is equal to technical efficiency divided by pure technical efficiency. In this paper, the DEA-Malmquist model proposed by Fare et al (1994) is used to measure the total factor productivity of China’s medical and health institutions.17 It overcomes the shortcomings of the traditional DEA model’s static evaluation. It dynamically reflects the total factor productivity of China’s medical and health institutions in different periods through panel data, making the results more accurate and reliable. According to the basic principles of DEA, we establish the following model.
where  is the Malmquist index,
is the Malmquist index,  and
and  represent the efficiency levels of medical and health institutions under the technical level of period t and t+1 respectively,
represent the efficiency levels of medical and health institutions under the technical level of period t and t+1 respectively,  is the efficiency level of period t+1 under the technical level of period t whilst
is the efficiency level of period t+1 under the technical level of period t whilst  is the efficiency level of period t under the technical level of period t+1. If the Malmquist index is greater than 1, it means that the medical and health institution’s productivity increases during period t and t+1. If the Malmquist index is equal to 1, it means that the medical and health institution’s productivity level remains unchanged at period t and t+1.
is the efficiency level of period t under the technical level of period t+1. If the Malmquist index is greater than 1, it means that the medical and health institution’s productivity increases during period t and t+1. If the Malmquist index is equal to 1, it means that the medical and health institution’s productivity level remains unchanged at period t and t+1.
The American sociologist Ragin proposed qualitative comparative analysis (QCA) in the 1980s, which combines qualitative and quantitative research methods based on case studies. Carrying out this theoretical transformation is of great significance in understanding the relationship between strategy, organizational design, and environmental context, so it is valuable to broader organizational design and strategy. Compared with traditional quantitative research, QCA is based on set theory and Boolean operation and explores a non-linear causality of multiple concurrent condition combinations based on complexity theory. Because QCA has obvious advantages in solving the complex causality of multiple factors, it is widely used in many fields such as society, medical treatment, and entrepreneurship.
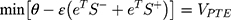
Fuzzy set qualitative comparative analysis (fsQCA) is a new research method combining fuzzy mathematics with qualitative comparative analysis. One of the advantages of fsQCA is the combination of fuzzy set and truth table analysis. This feature makes the classification of case conditions and results in qualitative comparative analysis no longer limited to simple binary division, and greatly expands the application scope and applicability of qualitative comparative analysis. At the same time, fsQCA organically combines the advantages of quantitative analysis and qualitative analysis by allowing membership scores in the internal between 0 and 1. In this method, we can regard a case as a combination of a series of conditions and results, and analyze whether the condition for the result is necessary or sufficient by comparing the influence of conditions on the results. The condition can be one of the reasons for the result, if it is sufficient. As for necessary conditions, we can test the consistency of these conditions to determine if any condition is logically necessary for the outcome. Consistency of the necessary fuzzy subset relationship can be evaluated as the following formula:
Indicators Selection
Input indicators reflect the human resources, material, and financial resources required by the medical and health institutions during their operation. Output indicators denote the ability of the medical and health institution to transform the input resources, and the specific manifestations are mostly the number of visits, hospital admissions, and medical income. In this study, by reviewing the relevant literature (see Table 1), we selected the actual number of staff, the actual number of beds, and total assets as the input indicators. We used outpatient visits, inpatient cases, and medical and health service income as indicators of output.18–22
 |
Table 1 Analysis of Input and Output Indicators of Operational Efficiency of Medical and Health Institutions |
Descriptive Statistics of Inputs and Outputs
As can be observed in Table 2, there is a continuous increase of medical and health resources in China from 2012 to 2017, and the average annual growth rate of total assets, the actual number of beds, and the actual number of staff are 15.02%, 6.76%, and 6.13%, respectively. Corresponding to this is the significant improvement in medical service capabilities, inpatient cases, outpatient visits, and medical and health service income, increasing steadily at an average annual growth rate of 3.52%, 6.49%, and 1.13%. It can be seen that the growth rate of the element input of medical and health institutions in China is slightly higher than the level of service output.
 |
Table 2 Descriptive Analysis of Inputs and Outputs from 2012 to 2017 |
Empirical Results
Correlation Analysis
When using the DEA-Malmquist model to analyze, it is necessary to perform a correlation test on the inputs and outputs to determine whether the two influence each other. From the results of the estimated correlation coefficients, the correlations between all input indicators and output indicators are greater than 0.75. They are significantly correlated at the 0.01 significance level, indicating that inputs and outputs have a high correlation, which meets the DEA model’s requirements for data equivariance. Table 3 shows the Pearson relevance matrix of input-output indicators.
 |
Table 3 Correlation Analysis of Inputs and Outputs |
Efficiency and Return to Scale of Medical and Health Institutions in China
As can be seen from Table 4, from 2012 to 2017, the overall operation of China’s medical and health institutions was relatively good, with an average technical efficiency value of 0.918, fluctuating in the range of 0.91 to 0.923. Pure technical efficiency and scale efficiency in China remained high. The average pure technical efficiency and scale efficiency were 0.947 and 0.970, respectively. The fluctuation range was small, indicating that the overall operation of medical and health institutions in China’s 31 provinces was stable. In addition, there were about ten provinces with the constant return to scale (scale efficiency=1), accounting for 32.58%, indicating that the above ten provinces have reached the optimal scale state, and there is no need to adjust the scale. In the meantime, 21 provinces have not yet reached the optimal production scale. Among them, about 14 provinces have increasing returns to scale, accounting for 45.16%, suggesting that appropriate expansion of local production inputs can bring a higher proportion of output, while the rest seven provinces were in a state of diminishing returns to scale, accounting for 22.58%. The increase in the input of medical and health institutions in these provinces was higher than the increase in output, which means the existing scale has redundant input and waste of resources, and increase input quantity will not bring a larger proportion of output.
 |
Table 4 Efficiency and Returns to Scale of Medical and Health Institutions in China from 2012 to 2017 |
Changes and Trends in the Efficiency of Medical and Health Institutions in Various Regions of China
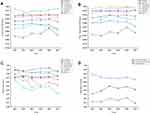
In this section, we comprehensively evaluate China’s medical and health institutions’ operation status from 2012 to 2017 based on the regional perspective. Figure 1 depicts the changes in technical efficiency, pure technical efficiency, and scale efficiency in China’s seven major regions, including Northeast China (Liaoning, Jilin, Heilongjiang), East China (Shanghai, Jiangsu, Zhejiang, Anhui, Fujian, Jiangxi, Shandong), North China (Beijing, Tianjin, Hebei, Shanxi, Inner Mongolia), Central China (Henan, Hubei, Hunan), South China (Guangdong, Guangxi, Hainan), Southwest China (Chongqing, Sichuan, Guizhou, Yunnan, Tibet) and Northwest China (Shaanxi, Gansu, Qinghai, Ningxia, Xinjiang).
From a vertical perspective, the technical efficiency of national medical and health institutions increased first and then decreased from 2012 to 2017, and reached a peak in 2016; pure technical efficiency peaked in 2014, and the overall trend was increasing, indicating that the management level of medical and health institutions is in need of improvement; scale efficiency has been fluctuating around 0.970, that is, the level of return to scale was relatively high, and service output was stable. Further analysis of the technical efficiency of medical and health institutions in various regions in China found that the overall trend in Central and East China continued to rise, the Northeast and Northwest regions increased first and then declined, North and Southwest regions showed a downward trend overall, and South China first declined and then increased, presenting a continuous trend of catching up. In regard to pure technical efficiency changes, Central China has shown a clear upward trend, and it surpassed Southwest China in 2017, ranking first in the country. East China and South China have been on a staggered upward trend, and the pure technical efficiency value has stabilized at around 0.975. At the same time, the Northwest, North China, and Northeast regions fluctuated greatly. In particular, North China’s pure technical efficiency and Northeast China dropped rapidly to below 0.9 in 2016. The data on the changes in the scale and efficiency of China’s medical and health care from 2012 to 2017 shows that only Central China and East China saw growth in 2017, while other regions have shown significant declines. At the same time, the scale efficiency of Central China has maintained steady growth in recent years, and it surpassed Northeast China to rank first in the country in 2017. But Northeast China’s scale efficiency has always been at the forefront of the country, as high as 0.986. This indicates that the low technical efficiency of medical and health institutions in Northeast China is limited by pure technical efficiency, not scale efficiency, which means that Northeast China needs to further optimize its management level, and introduce a team of high-tech talents.
Changes in Total Factor Productivity of China’s Medical and Health Institutions
Based on DEAP2.1 software, we analyze and evaluate the total factor productivity (TFP) of medical and health institutions in 31 provinces in China from 2012 to 2017 using an output-oriented DEA-Malmquist model. The specific total factor productivity changes and their decomposition are given in Table 5. The changes in the Malmquist index of Chinese medical and health institutions from 2012 to 2017 show that the average TFP is 0.965, namely TFP decline averagely by 3.5% annually. Moreover, the average Effech and Techch are 0.998 and 0.967, respectively, namely, technical efficiency drops by 3.3% annually, suppressing the growth of total factor productivity. We further decompose the comprehensive TFP and find that the average Pech and Sech are 1.001 and 0.997, respectively, which shows that the overall organization and management level of China’s medical and health institutions is relatively high. Still, the return to scale has not yet reached the optimal level, and the scale deviates from the appropriate state.
 |
Table 5 Malmquist Index of Operational Efficiency of Medical and Health Institutions in China |
Based on the distribution of total factor productivity in China’s medical and health institutions (see Table 6), we take the change in comprehensive technical efficiency as the horizontal axis and technical change as the vertical axis, and take the average of the comprehensive technical efficiency and technological change in 31 provinces as the dividing line, to divide 31 provinces into four types, namely type I (Effech>0.998, Techch>0.967), type II (Techch>0.967, Effech<0.998), type III (Effech>0.998, Techch<0.967), type IV (Effech<0.998, Techch<0.967).
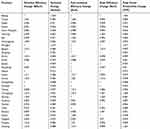 |
Table 6 Malmquist Index of Medical and Health Institutions in Different Provinces of China from 2012 to 2017 |
We also conducted a statistical analysis on the technical efficiency and pure technical efficiency of China’s medical and health institutions from 2012 to 2017. Our findings show that the distribution of the efficiency of resource allocation was differentiated and generally normal. The specific distribution is shown in Figure 2.
 |
Figure 2 Efficiency distribution of resource allocation (A) and total factor productivity scores for decision-making matrix (B). |
In addition to Beijing, Shanghai, Guangdong, Zhejiang, and Jiangsu, typical representatives of type I include Hubei, Anhui, Sichuan, Xinjiang, Jilin, Hainan, and other places. Through case comparison, it is found that Beijing, Shanghai, and Guangdong have attracted a large number of high-level health technicians by their high economic development and advanced medical and health technology, thus ensuring their long-term stable output. Furthermore, they positively motivate medical staff through active performance appraisal and finally form a triple combination of human, material, and financial resources. Hubei, Anhui, Sichuan and other provinces have also achieved rapid development of health care through appropriate financial subsidies and policy supports, which is mainly reflected in the significant increase in health indicators, the substantial increase in the number of medical and health institutions, the continuous increase in bed resources, and the rapid development and continuous improvement of health manpower and service capabilities. Specifically, the average annual growth rate of the actual number of beds, number of healthcare technicians, and total assets was 7.49%, 6.31%, and 15.67%. The annual average number of outpatient visits, inpatient Cases, and medical income steadily increased by 3.13%, 6.96%, and 13.5%. Type II provinces include Hainan, Yunnan, Fujian, Inner Mongolia, and Qinghai, and their technical change rate is higher than the national average level. Still, the management and operation of hospitals are relatively weak. Hunan, Liaoning, Heilongjiang, Jiangxi, Guangxi, Gansu, and Henan provinces are classed as type III. They have outstanding performance in comprehensive technical efficiency, but the technological changes are relatively weak, especially in Henan Province, which shows that their overall operation of medical and health institutions is acceptable, but the technical level is relatively backward. It is necessary for them to further innovate the talent introduction model, increase talent support, actively build an inter-provincial medical community, and realize technological innovation. Finally, only Shaanxi, Shanxi, Shandong, Hebei, Guizhou, and Tibet provinces belong to type IV, but Shaanxi, Shandong, Hebei, and Shanxi are, respectively, at the boundary of type II and type III, as long as their organization management and system innovation are strengthened, they can step into type I. In general, there is still much room for improvement in the total factor productivity of China’s medical and health institutions.
Improvement Scheme of Operation Efficiency of Medical and Health Institutions
Qualitative Comparative Analysis
This paper adopts a fuzzy-set qualitative comparative analysis (fsQCA), which explicitly conceptualizes cases as a combination of attributes and emphasizes that these combinations give the uniqueness of the case so that the classification of case analysis conditions and results is no longer limited to binary. The combinations make the calibration of variables more flexible, greatly reduce the occurrence of contradictory configurations, and expand the application scope and applicability of QCA. The use of this method will help companies provide more specific innovation and efficiency improvement programs. Therefore, this study adopts the fsQCA method to test how the five external environmental explanatory factors, including urban population density,16 regional GDP,19,20 and total dependency ratio,6 fatality rate,21 and financial allocation,22,23 can affect and interact with the operational efficiency of medical and health institutions.
Variable Calibration
Calibration is the process of assigning set membership to cases.24 In this paper, the direct calibration method is used to convert the original data into a fuzzy set value between 0 and 1,25 and the quartile method is used to determine the anchor points of the condition variable and the result variable.26 The results and conditional calibration are based on the 75% quantile value as the threshold for full membership, the 50% quantile value as the crossover point, and the 25% quantile value as the threshold for complete non-membership. The anchor point distribution of antecedent conditions and outcome variables is shown in Table 7.
 |
Table 7 Summary of the Calibration of All Variables |
Analysis of Necessary Conditions
Before constructing the truth table, the necessary conditions need to be checked, which helps to make appropriate assumptions about the logical remainder in the logic minimization process. In QCA analysis, consistency and coverage tests are used to determine whether a sufficient and necessary relationship exists between conditions and results. Generally speaking, if a certain condition variable is deemed necessary for the outcome variable, then the consistency score of the condition is not less than 0.9.27 It can be seen from Table 8 that none of the various antecedent conditions has a necessary impact on the technical efficiency of 0.9, so it does not constitute a necessary condition, indicating that each antecedent condition cannot explain the operating efficiency well. It also proves from the side that the efficiency of medical and health institutions is not affected by a single factor, but by a variety of factors. Next, we will continue to explore configurations that produce high operation efficiency and low operational efficiency.
 |
Table 8 Analysis Summary of Necessary Conditions |
Path to Improve the Operational Efficiency of Medical and Health Institutions
Based on the above research, a truth table is constructed to express the logic of the result that the condition combination meets. The truth table summarizes the cases in logarithmic units, and all combinations of antecedent variables and outcome variables are obtained. By observing the breaking point,28 this paper chooses 0.8 as the consistency threshold, the case threshold is set to 1, and detects the proportional reduction of inconsistency (PRI). After analyzing the data through fsQCA3.0 software analysis, it is found that there is no contradictory configuration in the obtained results, as shown in Table 9.
 |
Table 9 Configurations of Operating Efficiency of Medical and Health Institutions |
H1: High Fatality Rate and High Financial Allocation-Led
H1= GDP × total dependency ratio × case fatality rate × financial appropriation. It indicates that regardless of the urban population density, as long as the total dependency is relatively low, and the regional GDP, fatality rate and financial appropriation of medical and health institutions are higher, the technical efficiency will be higher. Representatives of this configuration are Type I regions such as Beijing, Shanghai, and Guangdong. Take Shanghai as an example, the superior city status and economic development level attract a large number of the high-quality labor force, making the labor force population base large. The total dependency ratio is low, and the government supports medical and health institutions with high financial allocation. In addition, due to its higher medical and health development level, more patients suffering from diseases with high fatality rate will be treated. These factors together affect Shanghai’s medical and health institutions’ operation efficiency, making its Effech, Pech, and Sech all remain at the level of 1, while Techch and TFP are 1.17.
H2: High Population Density, High GDP-Led
H2= population density × GDP × total dependency ratio × financial appropriation. It indicates that regardless of the case fatality rate, higher urban population density, regional GDP, total dependency ratio and financial subsidies from medical and health institutions are all conducive to the improvement of technical efficiency, and the first two environmental factors occupy a central position. This configuration is represented by Henan, Hunan, Hubei, and other places. Take Henan Province as an example, the high population base makes the urban population denser and increases the number of outpatients. In the meantime, due to the large economy of Henan province, the regional GDP is correspondingly higher. Compared with the situation in the H1 type region, the total dependency ratio and the financial allocation of medical and health institutions are not so ideal considering that there are not enough medical and health personnel and government financial investment in the province. However, it can still promote the improvement of technical efficiency. The Effech, Pech, and Sech of Henan are all equal to 1.
L1 and L2: Low Dependency Ratio and Low Financial Allocation-Led
L1= ~GDP × ~total dependency ratio × ~financial appropriation. It indicates that regardless of the urban population density and mortality rate, lower regional GDP, total dependency ratio, and financial appropriation will lead to low technical efficiency, and the latter two are the core factors. To give a clear example, Heilongjiang Province is one of the three northeastern provinces, but its GDP is not high due to its single economic structure and backward industrial mode, which makes the government face huge financial pressure. The government’s policy support for medical institutions is insufficient. At the same time, due to the impact of family planning, the problem of population aging in Heilongjiang Province is serious, the death rate is rising while the birth rate of newborns is falling, making the total dependency ratio low. The combination of the three factors makes Heilongjiang Province’s Techch, Sech, and TFP less than 1.
L2= ~population density × ~total dependency ratio × case fatality rate × ~financial appropriation. It indicates that regardless of the level of regional GDP, the other four external environmental factors are low, making technical efficiency insufficient. Take Inner Mongolia as an example, with its large area and low population density, the total dependency ratio is low due to L1, leading to the insufficient number of health technicians and a dearth of labourers. The low case fatality rate means that the number of outpatients is inadequate, and the ability to treat patients with high case fatality rate is insufficient. Finally, the government’s insufficient medical and health investment led to the low technical efficiency of Inner Mongolia, making the five Malmquist indexes shown in Table 6 all lower than 1.
Both L1 and L2 configurations are based on low dependency ratio and low financial allocation. Unlike regions with H1 configuration, they cannot attract a large number of the excellent labor force and are greatly affected by the aging of the population, which makes their total dependency ratio low. Moreover, the government is under great financial pressure because of the insufficient economic development, and the low financial input to the medical and health system is also a major reason.
L3: Low Fatality Rate, Low Financial Allocation-Led
L3= ~population density × ~GDP × ~case fatality rate × ~financial appropriation. It indicates that regardless of the total dependency ratio, the other four environmental factors are low as the characteristics of this configuration. Among them, low fatality rates and low financial appropriation are the main elements. Representatives of this configuration are Tibet and Ningxia provinces. Take the Tibet Autonomous Region as an example, due to its geographical location and poor livable environment, Tibet is sparsely populated. Its regional GDP is far lower than other more developed regions. And the low fatality rate and low financial allocation of medical and health institutions leave much room for the improvement of technical efficiency in Tibet. Specifically, the other four Malmquist indexes in Table 6 except for Pech are less than 1, especially TFP, which is only 0.898.
Summary and Discussion
This study uses the DEA-Malmquist method to analyze the total factor productivity of Chinese medical and health institutions for 2012–2017. In addition, the fsQCA method is used to discuss the path combination that may improve the efficient operation of medical and health institutions in different regions. The results are shown as follows.
First of all, the efficiency of resource allocation in China has made great progress after new health-reform, but the regional allocation of efficiency is unbalanced, which is consistent with the findings of Zheng et al.19 The average technical efficiency of Chinese medical and health institutions in the six years from 2012 to 2017 was 0.918. The average pure technical efficiency and scale efficiency values were 0.947 and 0.970, respectively. Provinces with constant returns to scale accounted for about 32.58%, while 21 provinces have not yet reached the optimal production scale, and provinces with increasing returns to scale and diminishing returns to scale accounted for 45.16% and 22.58%, respectively. In general, the scale and efficiency of China’s medical and health institutions need to be improved. The appropriate scale should be allocated according to each province’s economic level, the size of the population, and the operational conditions of medical and health institutions to avoid waste of resources and blind expansion.29
Secondly, similar to the research of relevant scholars, the development of China’s medical and health institutions shows the imbalance and deficiency of “strong in the South and weak in the north” and “superior in the West and inferior in the East”.30,31 There are significant differences in the scale of health care institutions in China from 2012 to 2017. The pure technical efficiency of Central China showed a clear upward trend in this time period, and it surpassed Southwest China in 2017, ranking first in the country. Northwest China, North China, and Northeast China fluctuated greatly, and the pure technical efficiency of North China and Northeast China declined rapidly in 2016 to below 0.9. The scale and efficiency of medical and health institutions in Central and East China increased in 2017, while other regions showed a significant decline. The scale and efficiency of Northeast China have always been in the forefront of the country but limited by pure technical efficiency. The operation level of medical and health institutions is not high, and it is necessary to introduce talents to improve their management level.
Thirdly, the total factor productivity of medical and health institutions in China decreased by 3.5% annually from 2012 to 2017, mainly due to insufficient technological progress, which is slightly different from the research conclusion of Yu et al and Chen et al.32,33 Effech and Techch were 0.998 and 0.967, respectively, with an average annual decrease of 1.2% and 3.3%. Meanwhile, none of the provinces with falling TFP has achieved technological progress. Additionally, we decompose Effech and find that Pech and Sech are 1.001 and 0.997, respectively, indicating that the management level of China’s medical and health institutions is relatively high. The return to scale has not yet reached the optimal scale, which slightly deviates from the optimal scale.
Fourthly, the results of fsQCA show that the paths affecting the operational efficiency of medical and health institutions include different combinations of conditions, which means that the operational efficiency of medical and health institutions is affected by many factors. In addition, through the study of typical cases, this paper analyzes two ways to achieve high technical efficiency and the causes of two types of low technical efficiency. These four approaches verified by representative provinces can provide decision-making references for improving the operational efficiency of medical and health institutions in China.
To comprehensively improve the total factor productivity of China’s medical and health institutions, we propose the following suggestions. From the hospital level, we recommend Chinese hospitals to fully implement the employment system and post-management system, improve the assessment and reward mechanism, innovate the talent introduction model, and mobilize technical personnel, management personnel, and skilled service personnel to participate in hospital governance with enthusiasm, initiative, and creativity. It is possible to narrow the capacity gap between hospitals by coordinating financial transfers to allocate more health resources to medical institutions in economically underdeveloped areas, especially quality health workers.34 To encourage the flow of medical talents to economically underdeveloped areas, these hospitals should improve their management level, encourage new technologies and new projects. Also, they should optimize the service quality of different departments and control operating costs rationally.
From the level of provincial and municipal governments, we recommend that the government increase hospital support, improve personnel mobility policies, promote the reform of the title system, and encourage the development of new technologies and new projects, so as to create a good external operating environment. The current situation is that the hospital has introduced a market-oriented management model and focused on shaping its brand image while improving medical equipment. Although the effect was considerable, it also virtually increased the cost of medical resources, causing the blind operation of medical institutions. It is necessary to restrict the rationality of the use of equipment from the national level, clarify the number and scale of the construction of various public medical institutions at all levels, enhance the construction of the connotation, and strengthen the link between the upper and lower levels and labor division. At the same time, it is necessary to integrate the service functions of medical and health institutions at all levels, combining prevention and treatment, optimize the hierarchical medical model, and provide the masses with systematic, continuous, and comprehensive medical and health services. All provinces should try their best to narrow the gap in health service between people at different levels. The implementation of regional health planning could promote a more reasonable inter-provincial health resource allocation, improve medical security in accordance with local conditions, and prevent blind expansion.35 Implementing the new medical reform policy and popularizing the hierarchical medical system are also the main tasks. Hospitals at all levels can take advantage of their respective strengths, and cooperate with third-grade class-A hospitals to improve the efficiency of resource utilization. In this way, hospitals can enhance their brand image, transform their understanding of market demand, and develop in an all-around way while creating economic benefits.
The contribution of this paper is that we first applied the fsQCA method to the study of efficiency improvement in the medical and health field, which can provide a reference for related scholars. Besides, fsQCA is used to analyze the antecedents of the allocation efficiency of regional medical and health resources in China. Four feasible ways to improve the technical efficiency of medical and health institutions are discussed, and the lack of literature on the efficiency improvement of medical institutions is filled. However, this paper is limited by the availability of output indicators, and the lack of medical income may lead to the deviation of the results. Further theoretical research and applications should focus on incorporating time-series variations into QCA.
Data Sharing Statement
Please contact author for data requests.
Ethical Approval
All data are based on previous published studies; thus, no ethical approvals are required. The outcomes of the analysis do not allow re-identification and the use of data cannot result in any damage or distress.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by Anhui Social Science under Grant No. AHSKQ2019D110.
Disclosure
The authors declare that they have no competing interests.
References
1. Li ZG, Wei H. A comprehensive evaluation of China’s TCM medical service system: an empirical research by integrated factor analysis and TOPSIS. Front Public Health. 2020;8:532420. doi:10.3389/fpubh.2020.532420
2. Li ZG, Li YK, Long D. Research on the improvement of technical efficiency of China’s property insurance industry: a fuzzy-set qualitative comparative analysis. Int J Emerging Markets. 2020;ahead-of-print(ahead–of–print). doi:10.1108/IJOEM-01-2020-0091
3. Chowdhury H, Zelenyuk V. Performance of hospital services in Ontario: DEA with truncated regression approach. Omega Int J Manag Sci. 2016;63:111–122. doi:10.1016/j.omega.2015.10.007
4. Flokou A, Aletras V, Niakas D. A window-DEA based efficiency evaluation of the public hospital sector in Greece during the 5-year economic crisis. PLoS One. 2017;12(5):e0177946.
5. Chen Y, Wang J, Zhu J, Sherman HD, Chou SY. How the Great Recession affects performance: a case of Pennsylvania hospitals using DEA. Ann Oper Res. 2019;278(1–2):77–99. doi:10.1007/s10479-017-2516-1
6. Thai KQ, Noguchi M. Evaluating efficiency of English acute foundation trusts under system reform: a two-stage DEA approach. Health Serv Outcomes Res Methodol. 2019;19(4):215–240. doi:10.1007/s10742-019-00203-6
7. Hunt DJ, Link CR. Better outcomes at lower costs? The effect of public health expenditures on hospital efficiency. Appl Econ. 2020;52(4):400–414. doi:10.1080/00036846.2019.1646405
8. Miller F, Wang J, Zhu J, Chen Y, Hockenberry J. Investigation of the impact of the Massachusetts Health Care Reform on hospital costs and quality of care. Ann Oper Res. 2017;250(1):129–146. doi:10.1007/s10479-015-1856-y
9. Khushalani J, Ozcan YA. Are hospitals producing quality care efficiently? An analysis using Dynamic Network Data Envelopment Analysis (DEA). Socioecon Plann Sci. 2017;60:15–23. doi:10.1016/j.seps.2017.01.009
10. Samsudin S, Jaafar AS, Applanaidu SD, Ali J, Majid R. Are public hospitals in Malaysia efficient? An application of DEA and Tobit analysis. Southeast Asian J Econ. 2016;4(2):1–20.
11. Marrakchi MD, Essid H. Efficiency Assessment of Tunisian Public Hospitals Using Data Envelopment Analysis (DEA). Giza: Economic Research Forum; 2019.
12. Omrani H, Shafaat K, Emrouznejad A. An integrated fuzzy clustering cooperative game data envelopment analysis model with application in hospital efficiency. Expert Syst Appl. 2018;114:615–628. doi:10.1016/j.eswa.2018.07.074
13. Aldabahi AG, Juni MH, Rosliza AM, Ying LP, Faisal I. Studying the efficiency of hospitals in the Riyadh region of Saudi Arabia using data envelopment analysis (DEA): a conceptual approach. Int J Public Health Clin Sci. 2019;6(6):1–19.
14. Huang MY, Luo D, Wang ZH, et al. Equity and efficiency of maternal and child health resources allocation in Hunan Province, China. BMC Health Serv Res. 2020;20(1):300. doi:10.1186/s12913-020-05185-7
15. Jia TY, Yuan HY. The application of DEA (Data Envelopment Analysis) window analysis in the assessment of influence on operational efficiencies after the establishment of branched hospitals. BMC Health Serv Res. 2017;17(1):265. doi:10.1186/s12913-017-2203-6
16. Guo H, Zhao Y, Niu T, Tsui KL. Hong Kong Hospital Authority resource efficiency evaluation: via a novel DEA-Malmquist model and Tobit regression model. PLoS One. 2018;13(2):e0193266. doi:10.1371/journal.pone.0193266
17. Färe R, Grosskopf S, Lovell CAK. Production Frontiers. Cambridge University Press; 1994.
18. Jiang N, Andrews A. Efficiency of New Zealand’s District Health Boards at providing hospital services: a stochastic frontier analysis. J Prod Anal. 2020;53(1):53–68. doi:10.1007/s11123-019-00550-z
19. Zheng W, Sun H, Zhang P, Zhou G, Jin Q, Lu X. A four-stage DEA-based efficiency evaluation of public hospitals in China after the implementation of new medical reforms. PLoS One. 2018;13(10):e0203780. doi:10.1371/journal.pone.0203780
20. Liu J, He BB, Xu XL, et al. Determinants of efficiency growth of county-level public hospitals-evidence from Chongqing, China. BMC Health Serv Res. 2019;19(1):858. doi:10.1186/s12913-019-4609-9
21. Herwartz H, Strumann C. Hospital efficiency under prospective reimbursement schemes: an empirical assessment for the case of Germany. Eur J Health Econ. 2014;15(2):175–186. doi:10.1007/s10198-013-0464-5
22. Samut PK, Cafri R. Analysis of the efficiency determinants of health systems in OECD countries by DEA and Panel Tobit. Soc Indic Res. 2016;129(1):113–132. doi:10.1007/s11205-015-1094-3
23. Sultan WIM, Crispim J. Measuring the efficiency of Palestinian public hospitals during 2010–2015: an application of a two-stage DEA method. BMC Health Serv Res. 2018;18(1):381. doi:10.1186/s12913-018-3228-1
24. Schneider CQ, Wagemann C. Doing justice to logical remainders in QCA: moving beyond the standard analysis. Polit Res Q. 2013;66(1):211–220.
25. Ragin CC. How to lure analytic social science out of the doldrums: some lessons from comparative research. Int Sociol. 2006;21(5):633–646. doi:10.1177/0268580906067834
26. Coduras A, Clemente JA, Ruiz J. A novel application of fuzzy-set qualitative comparative analysis to gem data. J Bus Res. 2016;69(4):1265–1270. doi:10.1016/j.jbusres.2015.10.090
27. Wu J, Li YK, Zhang D. Identifying women’s entrepreneurial barriers and empowering female entrepreneurship worldwide: a fuzzy-set QCA approach. Int Entrep Manag J. 2019;15(3):905–928. doi:10.1007/s11365-019-00570-z
28. Fiss PC. Building better causal theories: a fuzzy set approach to typologies in organization research. Acad Manag J. 2011;54(2):393–420. doi:10.5465/amj.2011.60263120
29. Zhang XY, Zhao L, Cui Z, Wang YG. Study on equity and efficiency of health resources and services based on key indicators in China. PLoS One. 2015;10(12):e0144809. doi:10.1371/journal.pone.0144809
30. Jin J, Wang JX, Ma XY, Wang YD, Li RY. Equality of medical health resource allocation in China based on the Gini coefficient method. Iran J Public Health. 2015;44(4):445–457.
31. Sun J, Luo HY. Evaluation on equality and efficiency of health resources allocation and health services utilization in China. Int J Equity Health. 2017;16(1):127. doi:10.1186/s12939-017-0614-y
32. Yu JN, Liu Z, Zhang TT, Hatab AA, Lan J. Measuring productivity of healthcare services under environmental constraints: evidence from China. BMC Health Serv Res. 2020;20(1):673. doi:10.1186/s12913-020-05496-9
33. Chen XL, Valdmanis V, Yu TT. Productivity growth in Chinese medical institutions during 2009–2018. Sustainability. 2020;12(8):3080. doi:10.3390/su12083080
34. Zhang T, Xu YJ, Ren JP, Sun LQ, Liu CJ. Inequality in the distribution of health resources and health services in China: hospitals versus primary care institutions. Int J Equity Health. 2017;16(1):42. doi:10.1186/s12939-017-0543-9
35. Liu W, Liu Y, Twum P, Li SX. National equity of health resource allocation in China: data from 2009 to 2013. Int J Equity Health. 2016;15(1):68. doi:10.1186/s12939-016-0357-1
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.