Back to Journals » International Journal of General Medicine » Volume 14
Comprehensive Assessment of Fetal Bilateral Ventriculomegaly Based on Genetic Disorders, Cytomegalovirus Infection, Extra Prenatal Imaging and Pregnancy Outcomes in a Tertiary Referral Center
Authors Guo D, He D, Shen Q, Lin N, He S, Dai Y, Li Y, Xu L , Wu X
Received 19 August 2021
Accepted for publication 11 October 2021
Published 5 November 2021 Volume 2021:14 Pages 7719—7728
DOI https://doi.org/10.2147/IJGM.S335011
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Danhua Guo,1 Deqin He,1 Qingmei Shen,1 Na Lin,1 Shuqiong He,1 Yifang Dai,1 Ying Li,1 Liangpu Xu,1 Xiaoqing Wu1,2
1Medical Genetic Diagnosis and Therapy Center of Fujian Provincial Maternity and Child Hospital, Affiliated Hospital of Fujian Medical University, Fujian Provincial Key Laboratory for Prenatal Diagnosis and Birth Defect, Fuzhou City, Fujian Province, People’s Republic of China; 2Department of Laboratory Medicine, Fujian Medical University, Fuzhou, 350002, Fujian, People’s Republic of China
Correspondence: Liangpu Xu; Xiaoqing Wu
Medical Genetic Diagnosis and Therapy Center of Fujian Provincial Maternity and Child Hospital, Affiliated Hospital of Fujian Medical University, Fujian Provincial Key Laboratory for Prenatal Diagnosis and Birth Defect, Fuzhou City, Fujian Province, 350001, People’s Republic of China
Email [email protected]; [email protected]
Objective: This retrospective study aimed to systematically evaluate the genetic disorders, cytomegalovirus (CMV) infection, extra ultrasound findings and outcomes of fetuses with bilateral ventriculomegaly (BVM).
Methods: Data from pregnancies with fetal BVM were obtained between 2014 and 2020. The cases were divided into groups of isolated bilateral ventriculomegaly (IBVM) and non-isolated bilateral ventriculomegaly (NIBVM) according to the presence of extra prenatal imaging. Subgroups of mild, moderate, and severe were determined according to lateral ventricle widths. The NIBVM group was further classified into pregnancies with soft markers, non-structural abnormalities, and structural abnormalities.
Results: A total of 353 pregnancies were enrolled, including 153 cases of IBVM and 200 cases of NIBVM. Conventional karyotyping was performed on 192 samples, and 15 cases of numerical abnormalities and 3 cases of unbalanced structural abnormalities were identified. Chromosomal microarray analysis (CMA) was concurrently performed on 108 of them and revealed additional 5 cases (4.7%) of copy number variants with clinical significance. CMV DNA testing was performed on 154 of the 192 cases that underwent invasive prenatal diagnosis, and a positive result was found in 2 (1.3%) cases. In the IBVM group, the percentage of favorable prognosis in the mild, moderate and severe pregnancies were 94.4%, 79.2%, and 4.8%, respectively, and the termination of pregnancy (TOP) rates were 4.6%, 20.8%, and 85.7%, respectively. In both the mild and moderate NIBVM, the TOP rates progressively increased and the favorable prognosis survival rates progressively decreased relative to the soft markers, non-structural abnormalities, and structural abnormalities, respectively. Approximately 94.1% of severe NIBVM ended in termination.
Conclusion: Genetic disorders and fetal infection are important etiology of BVM. CMA is highly recommended for genetic disorders’ evaluation. Pregnancies with severe BVM always ended in TOP, while in mild-to-moderate NIBVM, prenatal imaging by ultrasound and/or MRI plays important roles in the pregnancy outcomes.
Keywords: bilateral ventriculomegaly, genetic disorders, cytomegalovirus infection, prenatal imaging
Introduction
Fetal ventriculomegaly (VM) is an ultrasound diagnosis which refers to enlargement of the cerebral ventricular diameter (≥10 mm).1,2 It is one of the most common abnormalities of central nervous system with a prevalence of 0.3–2.0 per 1000 pregnancies.1,3 For clinical counseling, fetal VM is commonly categorized into mild (≥10 mm, <12 mm), moderate (≥12 mm, <15 mm), or severe (≥15 mm).4,5 Mild fetal VM is always considered benign and incidental, especially in the setting of isolation, with the likelihood of survival and normal neurodevelopment being greater than 90%.2,6 Severe VM or VM accompanied by structural abnormalities were more frequently described to be associated with low live-birth rates7,8 and poor outcomes9 in previous literatures.
Fetal VM can manifest as either unilateral VM or bilateral VM (BVM). BVM presents in approximately 40–50% of VM cases.10,11 Counseling and management of fetal BVM can be difficult due to widely variable prognoses that depend on many factors. When BVM is observed prenatally, detailed assessment of extra prenatal imaging, emanation of genetic abnormalities and congenital infection are essential for prognosis evaluation and clinical consultant. With regard to prenatal imaging, most reports focused on structural abnormalities.12,13 However, in clinical practice, BVM with soft markers and non-structural abnormalities are also frequently encountered. Limited data are available on the outcomes regarding such cases. Besides prenatal imaging, testing for genetic disorder and congenital infection are of great value for prognosis evaluation. In recent years, fetal chromosomal anomalies and copy number variants have gained more attention.12,14 Amniocentesis and cordocentesis should be generally suggested according to gestational age when BVM is detected. Cytomegalovirus (CMV) infection is a major cause of neurodevelopmental deficits and non-genetic sensorineural hearing loss,15,16 and is a non-specific, but important cause of VM.17,18 Once a prenatal diagnosis of BVM is made, the specimen such as amniotic fluid or cord blood should be tested for CMV DNA using polymerase chain reaction to evaluate congenital fetal infection.
In the current study, we provide a comprehensive analysis of BVM based on the genetic etiology, CMV infections etiology, ultrasound and/or MRI findings and pregnancy outcomes, in order to provide evidence-based information for better prenatal counseling and perinatal management.
Patients and Methods
Patients
A total of 421 singleton pregnancies with fetal BVM were referred to our center between May 1, 2014 and December 31, 2020. The diameters of both lateral ventricles were ≥10 mm, which was determined by fetal ultrasound and/or Magnetic Resonance Imaging (MRI) performed in our or other tertiary A-level hospitals. Sixty-eight cases were excluded from the study due to follow-up missing, as a result, a total of 353 cases were enrolled. According to the width of lateral ventricle, they were categorized into mild (≥10 mm, <12 mm), moderate (≥12mm, <15 mm) and severe (≥15 mm) groups. According to whether there are extra abnormalities in addition to VM found by detailed ultrasound and/or MRI examination or not, they were classified into non-isolated bilateral ventriculomegaly (NIBVM) and isolated bilateral ventriculomegaly (IBVM). Among the cases of NIBVM, the extra abnormalities were subgrouped as follows: soft markers, structural abnormalities and non-structural abnormalities. Fetal soft markers mainly including increased nuchal translucency, absence or hypoplasia of fetal nasal bone, echogenic intracardiac focus and echogenic bowel, short long bones, mild renal pelvis dilatation, single umbilical artery, choroid plexus cyst. Structural abnormalities refers to malformation of various systems, such as ventricular septal defect, Dandy–Walker malformation, neural tube defects, cortical defects horseshoe kidney, cerebellar vermis dysplasia, intracranial hemorrhage, and so on. Non-structural abnormalities mainly including fetal growth restriction, oligohydramnios and polyhydramnios. For some cases, invasive prenatal diagnosis was not performed due to patients’ declination or too late trimester, as a result, conventional karyotyping was available from 192 (54.9%) cases, and chromosomal array analysis (CMA) was available from 108 of them. Data on congenital CMV infection was available in 154 cases.
Conventional Karyotyping
Conventional karyotyping consisted of cell culture and G-banded karyotyping was conducted according to the standard protocols in our laboratory. Cultured amniotic fluid, or fetal cord blood then arrested in metaphase and finally Wright’s stain was used for G-banding at a resolution of 320–500 bands.
CMA
Genomic DNA was extracted from uncultured amniotic fluid, fetal cord blood using a QIAGEN kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions. Single nucleotide polymorphism array (SNP array) was performed using Affymetrix CytoScan 750K array (Affymetrix Inc., Santa Clara, CA, UA).To analyse the results, Chromosome Analysis Suite software (Affymetrix) and human genome version GRCh37 (hg19) were used. All detected CNVs were compared with in-house and national public CNV databases as follows: Database of Genomic Variants (DGV), Database of Chromosome Imbalance and Phenotype in Humans Using Ensemble Resources (DECIPHER), International Standards for Cytogenomic Arrays Consortium, and Online Mendelian Inheritance in Man (OMIM).
Incremental yield of CMA was defined as the yield of CMA over conventional karyotyping. The CMA results were classified into pathogenic, benign, likely pathogenic, likely benign, and variants of unknown significance (VOUS), based on the American College of Medical Genetics (ACMG) definitions, as well as our inner database. Clinically significant aberrations refer to pathogenic and likely pathogenic results. Parental CMA was recommended to determine the inheritance of CNVs.
Testing for Congenital CMV Infection
DNA was extracted from 100μL amniotic fluid or fetal cord blood on the Magna Pure LC Instrument (RocheMolecular Biochemicals, Meylan, France) using the Total NA serum-plasma kit (Roche Diagnostic). CMV DNA was amplified from these extracted DNA samples using the ABI Prism 7000 apparatus (Applied Biosystems, Courtaboeuf, France). CMV DNA load ≥1×105 copies/mL was considered as high load and positive result.
Follow-Up Assessments
Ultrasound examinations and/or MRI were suggested 2–4 weeks after first detection or several weeks before delivery, and even after birth. The clinical outcomes including termination of pregnancy (TOP), postnatal assessments focused on motor, language and intellectual development were collected via medical records or telephonic communication; the period of follow-up varied from 6 months to 6 years after birth. The study was approved by the Ethics Committee of Fujian Provincial Maternity and Child Hospital. Written informed consent to participate in the study was obtained from each patient.
Statistical Analysis
Statistical analysis was performed using the SPSS Statistics software v26.0 (IBM SPSS, Armonk, NY, USA). Comparisons between groups were conducted using the Chi-square test or the Fisher’s exact test, and P<0.05 was considered statistically significant.
Results
Descriptive Results
The enrolled cases were comprised of 153 cases of IBVM and 200 cases of NIBVM. In total, 61.4% of the IBVM pregnancies and 63.5% of the NIBVM pregnancies were diagnosed after 24 weeks of gestation. Mild VM was observed in 70.6% of IBVM group and 61.0% of NIBVM group. Details of the pregnancy characteristics are summarized in Table 1.
 |
Table 1 The Clinical Characteristics of 353 Pregnancies with Bilateral Ventriculomegaly |
Etiology Analysis: Chromosomal Aberrations and CMV Infection
Among 192 cases that underwent conventional karyotyping, a total of 18 (9.4%) had aberrations with clinical significance. The rate of karyotyping aberrations was 6.2% (5/81) in the IBVM group and 11.9% (13/109) in the NIBVM group. Approximately 20.0% (2/10) of severe BVM pregnancies had karyotyping aberrations, much higher than 5.1% (7/137) in mild and 6.0% (4/67) in moderated BVM pregnancies. The most frequently encountered aberration was trisomy 21, which was detected in 12 cases (6.3%). Among 108 cases for which conventional karyotyping and SNP array analyses were performed in parallel, clinically significant findings were detected in 14 fetuses (13.0%), involving nine clinical syndromes. Additional Microdeletion/microduplication syndromes were identified by SNP-array analysis in 5 (4.6%) fetuses involving 1p36 microdeletion syndrome (Case 1, Case 17), Sotos syndrome (Case 3), 16p13.11 microduplication syndrome (Case 2) and 16p13.11 microdeletion syndrome (Case 4). Detailed results are presented in Table 2.
 |
Table 2 Details of the Cases with Genetic Abnormalities of Clinical Significance |
With respect to CMV infection, 2 of the 154 cases tested (1.3%) were positive for CMV DNA. One fetus exhibited moderate VM and the other fetus showed mild VM and fetal growth restriction (FGR). Both CMV-positive cases ended in TOP due to progressive dilation during follow-up ultrasound examinations.
Ultrasound/MRI Findings and Outcomes of Pregnancies with BVM
Among 108 cases of mild IBVM, 102 (94.4%) showed favorable prognosis after birth, 5 (4.6%) opted for TOP due to chromosomal abnormalities (Table 3), and 1 study participant (0.9%) complained of language and attention defects at 6-year-old follow-up of the child. In the moderate IBVM group, 19 of the 24 cases (79.2%) had normal development after birth, 5 cases (20.8%) ended in TOP due to progressive VM observed during ultrasound monitoring. In severe IBVM, 18 of the 21 participants (85.7%) opted for TOP attributed to patients’ worries about abnormal neurodevelopment; two surviving cases (9.5%) had poor prognoses: one presented with language and mental retardation at the 4-year-old follow-up, the other one manifested as intellectual developmental disorder as well as severe hydrocephalus and dysplasia of the corpus callosum revealed by MRI.
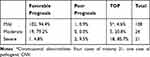 |
Table 3 Pregnancy Outcomes for Different Severity of Isolated Bilateral Ventriculomegaly |
In the NIBVM pregnancies, poor prognosis after birth was recorded in 14 (7.0%) cases. Among them, two cases of developmental delay were finally diagnosed as trisomy 21, and other fetuses mainly manifested as mental retardation, language development disorder, or poor muscle strength. The rate of favorable prognosis in mild and moderate BVM together with soft marker were 87.9% and 61.5%, respectively. In both the mild and moderate NIBVM, the TOP rates progressively increased and the favorable prognosis survival rates progressively decreased relative to the soft markers, non-structural abnormalities, and structural abnormalities, respectively. Approximately 94.1% of severe NIBVM ended in termination. Summary of the pregnancy outcomes is shown in Table 4. Extra intracranial abnormalities were observed in 55 (16.6%) fetuses, mainly including agenesis of corpus callosum, intracranial hemorrhage, and cerebellum dysplasia. Of them, 48 (87.3%) cases were ended in TOP; 5 (9.1%) cases showed normal neurological development during no more than 3-year-old follow-up. Regarding the rest two cases, one infant displayed severe neuromotor developmental delay and died at 1 year old, the other one manifested language development disorders at the time of the last follow-up assessment.
 |
Table 4 Pregnancy Outcomes of NIBVM with Different Subgroups of Prenatal Imaging |
Discussion
In the majority of previous studies, unilateral VM and BVM cases were not discussed separately12,19 To the best of our knowledge, the current study is one of the few large-cohort single-center studies focusing on BVM.
The Society of Obstetricians and Gynecologists of Canada (SOGC) recommends amniocentesis be offered to patients when fetal VM is detected so that karyotype and congenital infection assessments can be performed, regardless of whether other ultrasound anomalies are observed.20 Similar to some previous studies,9,21 the gestation age when VM was first detected in our series ranged from 13 to 40 weeks. However, nearly two-thirds of all cases are initially detected after 24 weeks of gestation, which impacts the prenatal diagnosis analysis of VM. On one hand, a portion of patients are reluctant to undergo cordocentesis due to surgical risk, while on the other hand, the gestation age of some pregnancies may be too late to perform invasive prenatal diagnostic procedures. The detection rate of karyotyping abnormalities reported by Chang et al22 was 12.1%, similar to 9.4% in our study. In previous reports,23,24 the chromosomal abnormality rates in severe VM pregnancies was higher than those in mild-to-moderate VM. In our research, which also revealed in our research, but the rate (20.0%) of karyotyping aberrations was much higher than that reported in previous reports.23,24 Consistent with previous reports,23,25,26 Down syndrome was the most common abnormality with an overall detection rate of 6.3%. Furthermore, an incremental diagnosis yield of 4.6% was revealed by CMA in 108 cases for which karyotyping and CMA were performed. The 1p36 deletion syndrome has been frequently reported in cases of VM. It is associated with language defects, behavioral symptoms, intellectual disabilities, epilepsy, and motor delays and usually a contributing factor in TOP decisions.27–31 The 16p13.11 microdeletion syndrome and 16p13.11 microduplication syndrome related to neurosusceptibility sites were detected in two fetuses with mild BVM. They had normal development during short-term follow-up and long-time follow-up was required for prognosis assessment. Case 17 was a fetus with mild BVM accompanied with echogenic intracardiac foci and had a microdeletion in 5q35.2q35.3. This microdeletion is related to Sotos syndrome, which may contribute to multisystem malformations, as well as growth and mental retardation.32,33 The above noted pathogenic/likely pathogenic CNVs identified in the mild-to-moderate BVM cases of our study would have been misdiagnosed if karyotyping alone was performed. Therefore, CMA should be strongly recommended for prenatal diagnosis of fetal BVM, regardless of the degree of VM and the status of extra prenatal imaging.
Screening for CMV infection is frequently recommended in cases of fetal VM,34–36 especially for cases in which amniocentesis or cordocentesis was performed. Pasquini et al and Abdel-Fattah et al suggested that testing for suspected congenital fetal infections on the basis of ultrasound features can be limited to CMV rather than a complete TORCH test.36,37 CMV infections affects nervous tissue development resulting in severe hearing impairment, delayed neurodevelopment, and/or visual impairment.38,39 The data on the incidence of CMV infection in VM varied greatly due to different screening strategies on different specimens. In our study, CMV infection was confirmed in two of the 154 cases tested, resulting in a positivity rate of 1.3%. One CMV-positive fetus had moderate IBVM, while the other positive fetus had mild BVM and FGR. Progressive lateral dilation was observed in both fetuses during ultrasound follow-up.
In the IBVM group, TOP rate increased and favorable prognosis rate decreased in concordance with the degree of VM severity. Five mild IBVM cases ended in TOP due to chromosomal abnormalities. In addition, 20.8% of the cases with moderate IBVM chose TOP due to progressive VM and 85.7% of those with severe IBVM selected TOP for the concerns about abnormal neurological development. Although severe VM is associated with an increased risk of prenatal and neonatal neurodevelopmental problems and death,9 in the study by Letouzey et al, the majority of children with apparently severe IBVM show normal neurodevelopmental outcome and no prenatal risk factors identify cases at higher risk for severely abnormal neurologic outcome,40 thus some fetuses in the TOP cases might be able to have favorable prognosis. It is necessary to accumulate more prognostic data about severe IBVM for a better clinical consultation.
In the NIBVM group, pregnancy outcome is largely affected by the nature of extra prenatal imaging (Supplementary Table 1) especially in mild and moderate NIBVM pregnancies. Most pregnancies of mild-to-moderate BVM accompanied by soft markers result in favorable prognosis. When non-structural abnormalities were found, the TOP rate increased and the rate of good prognosis decreased. The presence of extra-structural abnormalities has been reported to increase the morbidity/mortality and the likelihood of neurologic delay.41,42 The pregnancies of VM together with structural abnormalities had the highest TOP rate in our study. Specifically, agenesis of corpus callosum, intracranial hemorrhage, and cerebellum dysplasia were the frequently observed intracranial abnormalities. Of them, 87.3% ended in TOP, and only 9.1% displayed normal development. Therefore, when BVM is observed, the evaluation of extra prenatal imaging is of great influence on the pregnancy outcomes.
There are some limitations to our study. First, only cases with follow-up available were enrolled, thus the frequency of extra prenatal imaging could not be assessed. Second, fetal genetic evaluation and CMV infection assessment were not performed for all of the pregnancies. Third, the follow-up time was not sufficiently long, which may have affected the accuracy of the neurological development assessments.
In conclusion, genetic disorders and fetal infection are important etiology of BVM. CMA is highly recommended for genetic disorders’ evaluation. Pregnancies with severe BVM always ended in TOP, while in mild-to-moderate NIBVM, prenatal imaging by ultrasound and MRI plays important roles in the pregnancy outcomes.
Data Sharing Statement
The data described in this study are available upon reasonable request from the corresponding authors.
Ethics Approval and Consent to Participate
The present study was approved by the Protection of Human Ethics Committee of Fujian Provincial Maternity and Children’s Hospital, affiliated Hospital of Fujian Medical University. Written informed consent was obtained from individual or guardian participants. This study was conducted in accordance with the Declaration of Helsinki.
Acknowledgments
We would like to thank Min Zhang, Yan Wang, Lingji Chen and Bin Liang for their technical support on SNP-array analysis.
Funding
Fujian provincial health technology project (2019-ZQN-19) and The Science Foundation of the Fujian Province, China (Grant No. 2021J01415).
Disclosure
The authors declare they have no conflicts of interest.
References
1. Cardoza JD, Goldstein RB, Filly RA. Exclusion of fetal ventriculomegaly with a single measurement: the width of the lateral ventricular atrium. Radiology. 1988;169(3):711–714. doi:10.1148/radiology.169.3.3055034
2. Salomon LJ, Bernard JP, Ville Y. Reference ranges for fetal ventricular width: a non-normal approach. Ultrasound Obstet Gynecol. 2007;30(1):61–66. doi:10.1002/uog.4026
3. Benacerraf BR, Birnholz JC. The diagnosis of fetal hydrocephalus prior to 22 weeks. J Clin Ultrasound. 1987;15(8):531–536. doi:10.1002/jcu.1870150805
4. Griffiths PD, Reeves MJ, Morris JE, et al. A prospective study of fetuses with isolated ventriculomegaly investigated by antenatal sonography and in utero MR imaging. AJNR Am J Neuroradiol. 2010;31(1):106–111. doi:10.3174/ajnr.A1767
5. Chiu TH, Haliza G, Lin YH, et al. A retrospective study on the course and outcome of fetal ventriculomegaly. Taiwan J Obstet Gynecol. 2014;53(2):170–177. doi:10.1016/j.tjog.2014.04.008
6. Fox NS, Monteagudo A, Kuller JA, et al.; Society for Maternal-Fetal M, Electronic Address PSO. Mild fetal ventriculomegaly: diagnosis, evaluation, and management. Am J Obstet Gynecol. 2018;219(1):B2–B9. doi:10.1016/j.ajog.2018.04.039
7. Gaglioti P, Danelon D, Bontempo S, et al. Fetal cerebral ventriculomegaly: outcome in 176 cases. Ultrasound Obstet Gynecol. 2005;25(4):372–377. doi:10.1002/uog.1857
8. Hannon T, Tennant PW, Rankin J, et al. Epidemiology, natural history, progression, and postnatal outcome of severe fetal ventriculomegaly. Obstet Gynecol. 2012;120(6):1345–1353. doi:10.1097/AOG.0b013e3182732b53
9. Breeze AC, Alexander PM, Murdoch EM, et al. Obstetric and neonatal outcomes in severe fetal ventriculomegaly. Prenat Diagn. 2007;27(2):124–129. doi:10.1002/pd.1624
10. Griffiths PD, Brackley K, Bradburn M, et al. Anatomical subgroup analysis of the Meridian cohort: ventriculomegaly. Ultrasound Obstet Gynecol. 2017;50(6):736–744. doi:10.1002/uog.17475
11. Falip C, Blanc N, Maes E, et al. Postnatal clinical and imaging follow-up of infants with prenatal isolated mild ventriculomegaly: a series of 101 cases. Pediatr Radiol. 2007;37(10):981–989. doi:10.1007/s00247-007-0582-2
12. Tugcu AU, Gulumser C, Ecevit A, et al. Prenatal evaluation and postnatal early outcomes of fetal ventriculomegaly. Eur J Paediatr Neurol. 2014;18(6):736–740. doi:10.1016/j.ejpn.2014.07.002
13. Patel SK, Zamorano-Fernandez J, Nagaraj U, et al. Not all ventriculomegaly is created equal: diagnostic overview of fetal, neonatal and pediatric ventriculomegaly. Childs Nerv Syst. 2020;36(8):1681–1696. doi:10.1007/s00381-019-04384-w
14. Hu T, Tian T, Zhang Z, et al. Prenatal chromosomal microarray analysis in 2466 fetuses with ultrasonographic soft markers: a prospective cohort study. Am J Obstet Gynecol. 2021;224(5):516 e1–516 e16. doi:10.1016/j.ajog.2020.10.039
15. Kenneson A, Cannon MJ. Review and meta-analysis of the epidemiology of congenital cytomegalovirus (CMV) infection. Rev Med Virol. 2007;17(4):253–276. doi:10.1002/rmv.535
16. Alarcon A, Martinez-Biarge M, Cabañas F, et al. A prognostic neonatal neuroimaging scale for symptomatic congenital cytomegalovirus infection. Neonatology. 2016;110(4):277–285. doi:10.1159/000446690
17. Davis NL, King CC, Kourtis AP. Cytomegalovirus infection in pregnancy. Birth Defects Res. 2017;109(5):336–346. doi:10.1002/bdra.23601
18. Lombardi G, Garofoli F, Stronati M. Congenital cytomegalovirus infection: treatment, sequelae and follow-up. J Matern Fetal Neonatal Med. 2010;23(sup3):45–48. doi:10.3109/14767058.2010.506753
19. Hidaka N, Ishii K, Kanazawa R, et al. Perinatal characteristics of fetuses with borderline ventriculomegaly detected by routine ultrasonographic screening of low-risk populations. J Obstet Gynaecol Res. 2014;40(4):1030–1036. doi:10.1111/jog.12298
20. Van Den Hof MC, Wilson RD; Diagnostic Imaging Committee, Society of Obstetricians and Gynaecologists of Canada, Genetics Committee, Society of Obstetricians and Gynaecologists of Canada. Fetal soft markers in obstetric ultrasound. J Obstet Gynaecol Can. 2005;27(6):592–636.
21. Kennelly MM, Cooley SM, Mcparland PJ. Natural history of apparently isolated severe fetal ventriculomegaly: perinatal survival and neurodevelopmental outcome. Prenat Diagn. 2009;29(12):1135–1140. doi:10.1002/pd.2378
22. Chang Q, Yang Y, Peng Y, et al. Prenatal detection of chromosomal abnormalities and copy number variants in fetuses with ventriculomegaly. Eur J Paediatr Neurol. 2020;25:106–112. doi:10.1016/j.ejpn.2020.01.016
23. Gezer C, Ekin A, Ozeren M, et al. Chromosome abnormality incidence in fetuses with cerebral ventriculomegaly. J Obstet Gynaecol. 2014;34(5):387–391. doi:10.3109/01443615.2014.896885
24. Huang Y, Huang D, Zhong W, et al. Fetal lateral ventricular dilatation complicated with malformation diagnosed by ultrasound and its relationship with chromosome abnormalities. Chin J Med Imaging. 2017;25:617–622.
25. Donnelly JC, Platt LD, Rebarber A, et al. Association of copy number variants with specific ultrasonographically detected fetal anomalies. Obstet Gynecol. 2014;124(1):83–90. doi:10.1097/AOG.0000000000000336
26. Wang Y, Hu P, Xu Z. Copy number variations and fetal ventriculomegaly. Curr Opin Obstet Gynecol. 2018;30(2):104–110. doi:10.1097/GCO.0000000000000439
27. Guterman S, Beneteau C, Redon S, et al. Prenatal findings in 1p36 deletion syndrome: new cases and a literature review. Prenat Diagn. 2019;39(10):871–882. doi:10.1002/pd.5498
28. Toshimitsu M, Nagaoka S, Kobori S, et al. Exome-first approach in fetal akinesia reveals chromosome 1p36 deletion syndrome. Case Rep Obstet Gynecol. 2019;2019:6753184.
29. Yang CY, Kao CC, Chang SD, et al. 1p deletion syndrome: a prenatal diagnosis characterized by an abnormal 1st trimester combined screening test, yet a normal NIPT result. Taiwan J Obstet Gynecol. 2018;57(1):106–109. doi:10.1016/j.tjog.2017.12.017
30. Seo GH, Kim JH, Cho JH, et al. Identification of 1p36 deletion syndrome in patients with facial dysmorphism and developmental delay. Korean J Pediatr. 2016;59(1):16–23. doi:10.3345/kjp.2016.59.1.16
31. Campeau PM, Ah Mew N, Cartier L, et al. Prenatal diagnosis of monosomy 1p36: a focus on brain abnormalities and a review of the literature. Am J Med Genet A. 2008;146a(23):3062–3069. doi:10.1002/ajmg.a.32563
32. Manor J, Lalani SR. Overgrowth syndromes—evaluation, diagnosis, and management. Front Pediatr. 2020;8:574857. doi:10.3389/fped.2020.574857
33. Moirangthem A, Mandal K, Saxena D, et al. Genetic heterogeneity of disorders with overgrowth and intellectual disability: experience from a center in North India. Am J Med Genet A. 2021;185(8):2345–2355. doi:10.1002/ajmg.a.62241
34. Pilu G, Hobbins JC. Sonography of fetal cerebrospinal anomalies. Prenat Diagn. 2002;22(4):321–330. doi:10.1002/pd.310
35. Gaglioti P, Oberto M, Todros T. The significance of fetal ventriculomegaly: etiology, short- and long-term outcomes. Prenat Diagn. 2009;29(4):381–388. doi:10.1002/pd.2195
36. Pasquini L, Masini G, Gaini C, et al. The utility of infection screening in isolated mild ventriculomegaly: an observational retrospective study on 141 fetuses. Prenat Diagn. 2014;34(13):1295–1300. doi:10.1002/pd.4470
37. Abdel-Fattah SA, Bhat A, Illanes S, et al. TORCH test for fetal medicine indications: only CMV is necessary in the United Kingdom. Prenat Diagn. 2005;25(11):1028–1031. doi:10.1002/pd.1242
38. Hui L, Wood G. Perinatal outcome after maternal primary cytomegalovirus infection in the first trimester: a practical update and counseling aid. Prenat Diagn. 2015;35(1):1–7. doi:10.1002/pd.4497
39. Picone O, Vauloup-Fellous C, Cordier AG, et al. A series of 238 cytomegalovirus primary infections during pregnancy: description and outcome. Prenat Diagn. 2013;33(8):751–758. doi:10.1002/pd.4118
40. Letouzey M, Chadie A, Brasseur-Daudruy M, et al. Severe apparently isolated fetal ventriculomegaly and neurodevelopmental outcome. Prenat Diagn. 2017;37(8):820–826. doi:10.1002/pd.5095
41. Wax JR, Bookman L, Cartin A, et al. Mild fetal cerebral ventriculomegaly: diagnosis, clinical associations, and outcomes. Obstet Gynecol Surv. 2003;58(6):407–414. doi:10.1097/01.OGX.0000070069.43569.D7
42. Lee CS, Hong SH, Wang KC, et al. Fetal ventriculomegaly: prognosis in cases in which prenatal neurosurgical consultation was sought. J Neurosurg. 2006;105(4 Suppl):265–270.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
