Back to Journals » Patient Preference and Adherence » Volume 13
Compliance with care and poor sleep quality among hypertensive adults in a mountainous area of Hubei Province, People’s Republic of China
Received 14 April 2019
Accepted for publication 7 July 2019
Published 23 July 2019 Volume 2019:13 Pages 1221—1227
DOI https://doi.org/10.2147/PPA.S212241
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Yuting Zhang, Xiaodong Tan
Department of Occupational and Environmental Health, School of Health Sciences, Wuhan University, Wuhan 430071, People’s Republic of China
Background: Little information is available concerning the relationship between compliance with hypertensive care and poor quality of sleep among Chinese adults in rural areas. This study aimed to evaluate the association between the compliance with hypertensive care and sleep quality for hypertension of adults in a mountainous area in People’sRepublic of China.
Methods: A total of 551 hypertensive patients (30–96 years of age) living in a remote mountainous area were recruited. Poor sleep quality was assessed using the standard Pittsburgh Sleep Quality Index (PSQI), and compliance with care was measured based on the Compliance of Hypertensive Patients Scale (CHPS). Hypertension was defined as blood pressure ≥140/90 mmHg or treated with antihypertensive medication. The associations between sleep quality and compliance variables were examined using Pearson’s correlation. Multiple linear regressions were established to verify significant variables associated with respondents’ compliance with care and poor sleep quality.
Results: The average age of the sample was 67.15 years (SD=10.20), and 56.44% of the participants were female. The mean CHPS total score was 41.97 (SD=5.91), and the PSQI total score was 7.91 on average (SD=4.10). Correlation analysis revealed that patients with higher intention, healthier lifestyle, positive attitude and total compliance were more likely to have an increased risk of poor sleep quality. According to the results of multiple linear regression analyses, hypertension compliance was significantly associated with being female, married, non-rural residence and years of hypertension, while poor sleep quality had a significant association with living in rural areas, having concomitant disease and poor hypertension compliance.
Conclusions: There is a significant association between hypertension compliance and poor sleep quality. Future intervention programs should focus on improving compliance behavior as a modifiable background factor for sleep quality.
Keywords: People’s Republic of China; rural area, hypertension, compliance, poor sleep quality
Introduction
Hypertension is known as a leading risk factor of cardiovascular morbidity and mortality worldwide.1 It has been estimated that the number of adults with hypertension will increase to 1.56 billion by 2025 and most of the cases will occur in low- and middle-income countries.2 The risk factors of hypertension have aroused increasing attention,3 and the major risk factors have been well established, whereas poor sleep quality is one unconventional and often overlooked risk factor.4
High sleep quality is necessary to maintain body function, and it can reduce the risk of cardiovascular diseases.5 However, a previous study demonstrated that up to 40% of the elderly suffered from poor sleep initialization and maintenance.6 According to the statistics from the Centers for Disease Control and Prevention, 11% of the adults in the United States get insufficient sleep.7 In recent years, several prospective studies have revealed a robust relationship between sleep quality and the risk of hypertension.8–11 Though sleep quality is of high implication,5 studies about the relationship between poor sleep quality and negative health behaviors are surprisingly limited.12
Self-care is vital to chronic disease management, and both changes in behavior and lifestyle have exhibited significant reductions in blood pressure (BP). However, despite the availability of evidence-based guidelines, numerous hypertensive patients do not comply with the suggested recommendations. This is probably because many individuals with hypertension, even among patients who are aware of their condition, do not have severe symptoms to compel them to seek help, leading to poor compliance with care.13,14 Previous studies revealed that hypertension compliance remained significantly low due to the lack of information and support, poverty, difficulty obtaining the medication and side effects of the medication, low education, and poor access to health care.15–17 According to the World Health Organization, non-compliance for hypertension is a common issue that may lead to serious economic consequences (eg compromised health benefits and waste of money).18 Besides, the existing studies provided the overwhelming evidence that the greatest potential for facilitating the control of BP reflected in the improvement of the compliance with care.19–21
Despite the risen prevalence of hypertension with poor control, the characteristic of individuals in remote mountainous areas regarding hypertension compliance behaviors and the correlation of their sleep quality have been rarely studied. Determining how hypertension compliance effect sleep quality would inform the design of more effective interventions for this population in remote mountainous areas. This study aimed to identify factors associated with the hypertension compliance and its relationship between the poor sleep quality.
Materials and methods
Ethical statement
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional research committee and the guidelines of the Declaration of Helsinki. The present study was approved by research ethics committees of Wuhan University (2018-1602000-03-02) and the local institutional review board of Xuanen, Hubei. All participants provided written informed consent. No human or animal subjects, human cell lines or human tissues were performed.
Participants
Data for this study were extracted from a Self-Monitoring Intervention Programme for Hypertension Control in remote mountainous areas in Hubei province. In July 2018, a population-based and cross-sectional study was conducted. The program recruited participants meeting the following criteria: 1) living in the Xuanen Area, 2) aged over 18 years, 3) systolic BP≥140 mmHg and/or diastolic BP≥90 mmHg or treated with antihypertensive medication, and 4) exhibiting communication proficiency to perform study tasks. The exclusion criteria were as follows: 1) had cognitive dysfunction; and 2) too old to complete the investigation.
Procedures
Before data collection, six investigators participated in workshops conducted by Wuhan University. The investigators explained the objectives and procedures of the study to potential participants face-to-face, with unified language expression.
To consult on the implementation of the program, our research team partnered with local community leaders and township health centers personnel. We started to collect data after our study was approved by the local institutional review board. A total of 600 potential participants were identified through intensive community outreach activities in various settings (eg, village clinics, social clubs, grocery stores and house-to-house visitation). Eligible participants were given informed consent and interviewed face to face by trained research assistants. Among the 551 participants, 91.83% completed this survey.
Measurement
Assessment of sociodemographic
Participants’ sociodemographic characteristics included age, gender, ethnic group, marital status, occupation, residence, years of schooling, years of hypertension, family income and concomitant disease.
Assessment of compliance
The compliance was measured based on a 14-item Compliance of Hypertensive Patients Scale (CHPS) developed by Lahdenpera.22 The 14 questions concerning compliance were split into the following 6 areas: Intention (4 items), Lifestyle (3 items), Attitude (3 items), Responsibility (2 items), Smoking (1 item) and Medication use (1 item). Each item is scored on a 4-point Likert scale, with 1 indicating “not at all compliance” to 4 indicating “totally compliance”. Higher scores indicate higher levels of compliance. The Cronbach’s Alpha was 0.69 in this sample.
Assessment of poor sleep quality
Sleep quality was assessed using the standard Pittsburgh Sleep Quality Index (PSQI) by its seven dimensions (eg, subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleeping medication and daytime dysfunction).23 The score ranges from 0 to 21 points, with ‘0ʹ indicating no difficulty and ‘21ʹ indicating severe difficulties in all areas. Higher scores indicate higher levels of poor sleep quality. The coefficient of the PSQI ranged from 0.82 to 0.83 at different population, and acceptable reliability coefficient reached 0.77–0.85 among Chinese population.24
Data analysis
Demographic characteristics and scores of scales were calculated. Continuous variables are expressed as mean and standard deviation. Categorical variables are expressed as percentages. The associations between sleep quality and compliance variables were first examined using Pearson’s correlation. Subsequently, multiple linear regressions were established to verify whether demographic characteristics are associated with respondents’ compliance with care. In addition, the associating effect of compliance on poor sleep quality was assessed in multiple linear regressions with sleep quality as the outcome variable, and then that effect of demographic characteristics was assessed.
SPSS software version 21.0 was used to analyze the data. Values of two-sided P<0.05 were considered statistically significant.
Results
Characteristics of the sample
The sample characteristics are summarized in Table 1. Of the 551 subjects, 311 (56.44%) were female, with a mean age of 67.15 years (standard deviation: 10.20, range: 30–96). Over half of the participants (52.09%) ethnicity group was Tujia, followed by Han. Most of the participants (72.78%) were married and a large majority (90.02%) were farmers. Almost all (94.19%) of the participants lived in a rural area, and most of the participants dropped out from their primary school. More than half of the participants (54.26%) reported one or more concomitant diseases, and years of hypertension ranged from <1 year to more than 10 years. The family monthly income of most of the participants (70.24%) was <2000 Yuan. The mean total score of compliance was 41.97 (SD=5.91), and the mean total PSQI was 7.91 (SD=4.10).
 |
Table 1 Demographic characteristics of sample (N=551) |
The correlations among key study variables
As indicated in Table 2, the results show that participants’ higher intention toward hypertension, healthier lifestyle, positive attitude toward care and total compliance was significantly correlated with higher subjective sleep quality (P<0.01). Likewise, a stronger sense of responsibility had a significant association with lighter difficulties in sleep latency, duration and total PSQI score (P<0.01). Milder daytime dysfunction was significantly associated with higher intention, positive attitude and total compliance. Furthermore, participants’ intention, responsibility and total compliance were negatively correlated with difficulties in total sleep quality (P<0.05).
 |
Table 2 Correlations between patients’ hypertension compliance and poor sleep quality (N=551) |
Factors associated with CHPS scores
To further explore the degree of bias associated with our sample, Table 3 presents the regression results for compliance. The overall model of compliance was significant (R2=0.113, F(10, 540) =6.874, P<0.001). Gender, marital status, residence and years of hypertension had a significant association with CHPS scores, while age, ethnic group, occupation, years of schooling, family income and concomitant diseases were omitted to account for the variation.
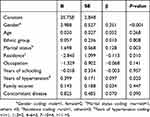 |
Table 3 Multiple linear regression analysis of socio-demographics with hypertension compliance of participants (N=551) |
Factors associated with PSQI scores
Table 4 demonstrates the regression results for poor sleep quality scores. Residence, concomitant disease and total CHPS scores were emerged as significant association factors of PSQI score, while other variables were all omitted to account for significant variance in this model. The overall model was significant (R2=0.057, F(11, 539) =2.947, P=0.001).
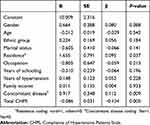 |
Table 4 Multiple linear regression analysis of socio-demographic and total CHPS with hypertension compliance of participants (N=551) |
Discussion
Despite the high prevalence and burden on public health caused by hypertension, the factors associated with its development and progression have not been completely identified. Previous experimental and epidemiologic study25,26 has shown that poor sleep quality and insufficient sleep exacerbate the incidence rate of hypertension. That is, sleep quality may be an indirect factor responsible for cardiovascular damage. Understanding the effect of compliance with hypertension care on sleep quality could give an accurate insight into design of psychosocial interventions to reduce risk of poor sleep quality. This study contributes to be the first research to explore correlates of hypertension compliance with sleep quality among adults with hypertension.
We found that higher hypertension compliance pays a significant role in decreasing risk of poor sleep quality. As Ko27 noted earlier, when faced with multiple health problems, a high level of self-efficacy may lead to successful manage care, symptoms and lifestyle adherence to living with a chronic disease condition, thus, they may maintain better physical and psychosocial consequences. Schmieder28 also found that patients with treatment-resistant hypertension had increase stress and anxiety, and had a poor overall health condition. Sleep is an integral part of daily life, our finding, together with previous studies, underscores the importance of compliance behaviors to improve physical condition.
To date, there exists no general definition of compliance. Compared with the studies on the control of hypertension, few studies focused on the factors associated with the compliance of hypertensive patients. In this study, we adopted the conception from Lahdenpera,22 who defined compliance as the hypertensive patients work in collaboration with the health care personnel proactively and change their lifestyle according to the recommendations. We found years of hypertension to be a significant factor in the regression model associated with compliance behavior. This is probably because years of hypertension can affect patients’ attitude toward the care. The effect of an individual’s hypertension awareness has a critical impact on self-care management practices and it was associated with reduced hypertensive compliance.29 On the one hand, manifestation of symptoms promoted their hypertensive compliance. On the other hand, with the extension of disease time, some patient might feel it unnecessary to continue with care when they were feeling well. Thus, our finding implies that future studies must establish a cohort that track the relationship between years of hypertension and compliance among Chinese people.
Meanwhile, we found family income to be insignificant factors associated with hypertension compliance. This result is inconsistent with Osamor30 who pointed out that when people feel hungry, only food matters them. Similar findings regarding socioeconomic status and its effect on hypertension compliance can also be found in other settings.31,32 In South Africa, previous study31 indicated that compared with people in the low socioeconomic index, those with greater economic resources were more likely to pay for all types of health services. Similar in Nigeria, a prior study by Akpa32 reported that poor socioeconomic status had negative effect on health seeking behaviors for hypertension and compliance to treatment. Whether the lack of other variables reflecting the true relationship between family income and compliance was uncertain, or it might be the practice effects of New Rural Cooperative Medical System33 in remote areas that made it possible for people in remote mountain district to get adequate medical resources. The result of this study, however, point to a need for a more rigorously designed sample to tease out the correlates of family income with hypertension compliance as hypothesized.
Given the impact of socio-demographic on sleep quality, our present study indicated that residence and concomitant disease were significantly associated with sleep quality among hypertensive patients. This result might be explained that our sample consisted of 94.19% people living in rural areas and 90% were farmers, they engaged in farm work in the daytime, this living environment leads to maintain the ability to develop sleep habits to the other days’ labor work. Other variables were not associated with sleep quality. However, these findings were inconsistent with other existed findings, demonstrating that gender,34 marital status,35 education level36 and employment37 were all linked to poor sleep quality. We consider that these indicators may have some potential relationship with sleep quality, which requires further studies.
Hypertensive adults living in remote mountain areas are a vulnerable group in People's Republic of China, thus studying their sleep quality is of high implication. The strength of this study is that it is the first to evaluate the relationship between compliance and sleep quality. Besides, our data are considered very reliable since it was based on face-to-face interviews instead of telephone interviews. However, several limitations of this study are noteworthy. First, the cross-sectional design cannot determine a causal relationship between self-reported compliance and sleep quality. Second, the present study did not include all background variables (eg, body mass index, smoking, alcohol consumption, chronic obstructive pulmonary disease and milder forms of exercise), which may affect sleep quality or BP as well. Third, our settings are only involved in Xuanen Country, and our results cannot be generalized to include all adults in rural areas of People's Republic of China. Furthermore, since most educated people and young people migrate to the cities to earn a living, our study population cannot represent all the general population in rural areas. Lastly, all measurements were obtained from self-report, leading to reporting bias (eg, recall error, social desirability and other types of misreporting). Future studies adopting polysomnograms are warranted. More generally, the present study only provided information about inter-individual differences in sleep quality, and further longitudinal research is required to draw conclusions regarding the risk of poor sleep quality in a comprehensive set of domains as well as different markers and determinants during the life course of hypertensive patients.
Conclusion
Our findings suggested that a high global PSQI score is associated with poor hypertension compliance. According to our results, we found that improving the compliance to hypertensive care may be an effective intervention to improve patients’ sleep quality. Subsequent research should focus more on modifiable variables (eg, compliance) as a means to improve sleep quality among hypertensive patients. Furthermore, a larger sample population that is sufficiently representative and a larger number of variables can better enrich other factors affecting sleep quality in different residence and ethnic samples with hypertension.
Abbreviations
BP, blood pressure; PSQI, Pittsburgh Sleep Quality Index; CHPS, Compliance of Hypertensive Patients Scale.
Acknowledgment
We gratefully acknowledge all participants in this study.
Author contributions
All authors contributed to investigation, data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
This research was supported by a grant from the 2018 College Students’ Summer Social Practice of “San Xia Xiang Program” of Wuhan University and identifier: 2018-1602000-03-02. The authors report no other conflicts of interest in this work.
References
1. Lim S, Vos T, Bruce N. The burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions 1990–2010: a systematic analysis for the global burden of disease study 2010[J]. LANCET. 2012;380:2224–2260. doi:10.1016/S0140-6736(12)61766-8
2. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. doi:10.1016/S0140-6736(05)17741-1
3. Abudesimu A, Liu F, Siti D, et al. An assessment of platelet parameters in different ethnic groups with hypertension subtypes and associated risk factors in Xinjiang, China. Clin Exp Hypertens. 2018;40:1–8. doi:10.1080/10641963.2017.1411494
4. Bansil P, Kuklina EV, Merritt RK, Yoon PW. Associations between sleep disorders, sleep duration, quality of sleep, and hypertension: results from the National Health And Nutrition Examination Survey, 2005 to 2008. J Clin Hypertens. 2011;13:739–743. doi:10.1111/j.1751-7176.2011.00500.x
5. Lo K, Woo BFY, Wong M, Tam WWS. Subjective sleep quality, blood pressure, and hypertension: a meta-analysis. J Clin Hypertens. 2018. doi:10.1111/jch.13220
6. Maria C, Jatinder B, Aysha B, et al. Increased prevalence of insomnia and changes in hypnotics use in England over 15 years: analysis of the 1993, 2000, and 2007 National Psychiatric Morbidity Surveys. Sleep. 2012;35:377. doi:10.5665/sleep.1700
7. CDC P. Perceived insufficient rest or sleep among adults - United States, 2008. Morbidity Mortality Weekly Rep. 2009;58:1175–1179.
8. Lu K, Chen J, Wang L, et al. Association of sleep duration, sleep quality and shift-work schedule in relation to hypertension prevalence in chinese adult males: a cross-sectional survey. Int J Environ Res Public Health. 2017;14:210. doi:10.3390/ijerph14020210
9. Liu RQ, Qian Z, Trevathan E, et al. Poor sleep quality associated with high risk of hypertension and elevated blood pressure in China: results from a large population-based study. Hypertens Res Off J Jan Soc Hypertens. 2016;39:54. doi:10.1038/hr.2015.98
10. Okubo N, Matsuzaka M, Takahashi I, et al. Relationship between self-reported sleep quality and metabolic syndrome in general population. BMC Public Health. 2014;14:1–7. doi:10.1186/1471-2458-14-1
11. Pepin JL. Hypertension and sleep: overview of a tight relationship. Sleep Med Rev. 2014;18:509–519. doi:10.1016/j.smrv.2014.03.003
12. Livingstone KM, Mcnaughton SA. A health behavior score is associated with hypertension and obesity among Australian adults. Obesity. 2017. doi:10.1002/oby.21911
13. Kayima J, Wanyenze RK, Katamba A, Leontsini E, Nuwaha F. Hypertension awareness, treatment and control in Africa: a systematic review. BMC Cardiovasc Disord. 2013;13(1):1–11. doi:10.1186/1471-2261-13-1
14. Musinguzi G, Anthierens S, Nuwaha F, Geertruyden JPV, Wanyenze RK, Bastiaens H. Factors influencing compliance and health seeking behaviour for hypertension in Mukono and Buikwe in Uganda: a qualitative study. Int J Hypertens. 2018;2:1–13. doi:10.1155/2018/8307591
15. Lubaki JPF, Mabuza L, Malete N, Maduna P, Ndimande JV. Reasons for non-compliance among patients with hypertension at Vanga Hospital, Bandundu Province, Democratic Republic of Congo: a qualitative study. Afr J Primary Health Care Family Med. 2009;1(1):068. doi:10.4102/phcfm.v1i1.68
16. Bourne PA. Impact of poverty, not seeking medical care, unemployment, inflation, self-reported illness, and health insurance on mortality in Jamaica. N Am J Med Sci. 2009;1:99–109.
17. Bourne PA, Morris C, Charles CA, Eldemire-Shearer D, Kerr-Campbell MD, Crawford TV. Health literacy and health seeking behavior among older men in a middle-income nation. Patient Relat Outcome Meas. 2010;1:39. doi:10.2147/PROM.S11141
18. Burkhart PV, Sabaté E. Adherence to long-term therapies: evidence for action. J Nurs Scholarship Off Publ Sigma Theta Tau Int Honor Soc Nurs. 2003;35:207.
19. Jenkinsjones S, Parviainen L, Porter J, et al. Poor compliance and increased mortality, depression and healthcare costs in patients with congenital adrenal hyperplasia. Eur J Endocrinol. 2018;178:
20. Townsend RR, Mahfoud F, Kandzari DE, et al. Catheter-based renal denervation in patients with uncontrolled hypertension in the absence of antihypertensive medications (SPYRAL HTN-OFF MED): a randomised, sham-controlled, proof-of-concept trial. Lancet. 2017;390:2160–2170. doi:10.1016/S0140-6736(17)32281-X
21. Kuria N, Reid A, Owiti P, et al. Compliance to follow up and adherence to medication in hypertensive patients in an urban informal settlement in Kenya: comparison of three models of care. Trop Med Int Health. 2018. doi:10.1111/tmi.13078
22. Helvi Kyngäs RN, Rn TLM. Compliance of patients with hypertension and associated factors. J Adv Nurs. 1999;29:832–839.
23. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiat Res. 1989;28:193–213. doi:10.1016/0165-1781(89)90047-4
24. Tsai PS, Wang SY, Wang MY, et al. Psychometric evaluation of the Chinese Version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual Life Res. 2005;14:1943–1952. doi:10.1007/s11136-005-4346-x
25. Zhang J, Wang C, Gong W, et al. Poor sleep quality is responsible for the non-dipper pattern in hypertensive but not in normotensive chronic kidney disease patients. Nephrology. 2017;22(9):690–698. doi:10.1111/nep.12839
26. Lo K, Woo B, Wong M, et al. Subjective sleep quality, blood pressure, and hypertension: a meta-analysis [J]. The Journal of Clinical Hypertension. 2018;20(3):592–605. doi:10.1111/jch.13220
27. Ko D, Bratzke LC, Roberts T. Self-management assessment in multiple chronic conditions: a narrative review of literature. International Journal of Nursing Studies. 2018;83:83–90. doi:10.1016/j.ijnurstu.2018.04.009
28. Schmieder RE, Grassi G, Kjeldsen SE. Patients with treatment-resistant hypertension report increased stress and anxiety: a worldwide study. J Hypertens. 2016;31:610. doi:10.1097/HJH.0b013e32835d6e53
29. Banach M, Rysz J, Malyszko J, et al. Patients with prehypertension-do we have enough evidence to treat them?. Current Vascular Pharmacology. 2014;12(4):586–97. doi:10.2174/15701611113119990126
30. Osamor PE. Social support and management of hypertension in south-west Nigeria. Cardiovasc J Afr. 2015;26:29–33. doi:10.5830/CVJA-2014-066.
31. Petrella RJ, Merikle EP, Jones J. Prevalence, treatment, and control of hypertension in primary care: gaps, trends, and opportunities. J Clin Hypertens. 2007;9:28–35. doi:10.1111/j.1524-6175.2007.05944.x
32. Akpa MR, Agomuoh DI, Odia OJ. Drug compliance among hypertensive patients in Port Harcourt, Nigeria. Niger J Med J National Assoc Resident Doctors Niger. 2005;14:55.
33. Shengji L, Manxue C, Kangyin L. Policy effort analysis on China’s new rural cooperative medical system. Nat Commun. 2014;5:4094. doi:10.1038/ncomms5972
34. Lallukka T, Sivertsen B, Kronholm E, Yu SB, Øverland S, Glozier N. Association of sleep duration and sleep quality with the physical, social, and emotional functioning among Australian adults. Sleep Health. 2018;4(2):S1137904322. doi:10.1016/j.sleh.2017.11.006
35. Stafford M, Bendayan R, Tymoszuk U, Kuh D. Social support from the closest person and sleep quality in later life: evidence from a British birth cohort study. J Psychosom Res. 2017;98:1–9. doi:10.1016/j.jpsychores.2017.04.014
36. Barazzetta M, Ghislandi S. Family income and material deprivation: do they matter for sleep quality and quantity in early life? Evidence from a longitudinal study. SLEEP. 2017;40(3). doi:10.1093/sleep/zsw066
37. .Baker E, Richdale A, Hazi A. Employment status is related to sleep problems in adults with autism spectrum disorder and no comorbid intellectual impairment. Autism. 2019;23(2):531–536. doi:10.1177/1362361317745857
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
