Back to Journals » Patient Preference and Adherence » Volume 8
Completion of therapeutic and safety monitoring tests in Lebanese outpatients on chronic medications: a cross-sectional study
Received 11 June 2014
Accepted for publication 11 July 2014
Published 8 September 2014 Volume 2014:8 Pages 1195—1204
DOI https://doi.org/10.2147/PPA.S69250
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Elsy Ramia, Rony Zeenny
Department of Pharmacy Practice, School of Pharmacy, Lebanese American University, Byblos, Lebanon
Purpose: To evaluate the appropriateness of laboratory-test monitoring recommended for patients on chronic medication therapies in the Lebanese community setting.
Patients and methods: In October 2011, all outpatients visiting selected community pharmacies in Lebanon were screened by pharmacists to evaluate their use of one or more chronic medications requiring safety and/or therapeutic laboratory tests. The list of medications was elaborated after an extensive review of laboratory-test monitoring recommendations from pertinent up-to-date clinical guidelines, medications that have been issued black box warnings for monitoring, and the most current information from the US Food and Drug Administration website. Patients receiving these medications were subjected to a questionnaire assessing the appropriateness of their laboratory-test monitoring. The study was approved by the Lebanese American University’s Institutional Review Board.
Results: A total of 284 outpatients, with almost equal distribution by sex, were identified during the aforementioned period to be on one or more of the specified medications. The majority of the sample (68%) was younger than 65 years of age. Overall, most of the study group (65%) were found to be partially monitored with laboratory tests, while only 27% were fully monitored and 8% were not monitored at all. The study group reported clinic-visit intervals as follows: more than a year (35%), on yearly basis (18%), every 6 months (25%), every 3 months (16%), less than 3 months (6%).
Conclusion: Seventy-three percent (73%) of the study group were receiving incomplete therapeutic/safety laboratory-test monitoring recommended for patients on chronic medication in the Lebanese community. It is concluded from the results that patients need to better understand the importance of recommended test monitoring for the safe and effective use of their medications. Education by physicians may be required to achieve better understanding.
Keywords: laboratory tests, hypertension, statins, diabetes, chronic diseases, drugs, disease management, primary care
Introduction
Therapeutic and safety drug monitoring is an essential element for the effective use of medications and for high-quality medical care. It allows clinicians to use better correlations between drug concentrations and both efficacy and toxicity, and contributes to an ethos of safety. These factors raise standards of medical practice.
In fact, a common cause of therapeutic failures and adverse drug reactions in ambulatory care is related to suboptimal patient monitoring, including inadequate follow-up and insufficient use of laboratory tests to monitor organ function and drug levels.1
Studies done on ambulatory patients showed that almost 60% of the reported preventable adverse events occurred at the stage of monitoring.2,3 A report from two large academic long-term care facilities also confirms that inappropriate monitoring, in addition to inappropriate prescribing, are the most common errors in preventable adverse drug events, whereas errors in dispensing and administration are less commonly identified.4 Additionally, studies have shown a gap between guideline recommendations and actual frequency of baseline medication laboratory-test monitoring.5
Furthermore, the Institute of Medicine report, To Err is Human: Building a Safer Health System, has categorized medical error based on diagnostic, treatment, prevention, and other types of errors.6 Specifically, failure to employ indicated tests, to act on their results, or to follow-up were considered to be medical errors.
Total annual costs of medical errors resulting in injury are estimated to be between $17 billion and $29 billion per year.6 Over one-half of these expenditures are for direct health care costs, such as longer stay or treatment. Thus, the health and economic burden of medication errors, adverse drug reactions, and therapy failures occurring throughout the health care continuum remain significant.7
In summary, the indications for carrying out therapeutic/safety drug monitoring are limited not only to avoiding toxicity of chronic medications, but also to monitoring patient compliance, adjusting drug dose to the patients’ individual need, assessing the control of the disease, and monitoring and detecting drug interactions.
Aim of the study
There is a dearth of literature that assessed the completion of therapeutic/safety monitoring tests of chronic medications in the Middle East and North Africa region, and particularly in the Lebanese community. Thus, the primary objective of this study was to evaluate the completion of therapeutic/safety monitoring tests recommended for patients on chronic medication therapies in the Lebanese community setting.
Ethical approval
The study was approved by the Lebanese American University’s Institutional Review Board. A written informed consent was not needed for this type of protocol approval; however, every participant gave his/her oral informed consent when approached prior to collection of information. The purpose of the study was elucidated to all patients for their approval before participation.
Methods
Study setting
The study was conducted in two community pharmacies affiliated with the School of Pharmacy at the Lebanese American University, located in the Beirut area. Pharmacies were selected on the basis of their ability to attract sufficient numbers and variety of patients, a good record of professionalism and care toward patients, and their ability to protect patient privacy and confidentiality.
Medication selection
The study group developed a list of chronic medications requiring therapeutic/safety monitoring parameters (Table 1). This list of medications was expanded after an extensive review of monitoring recommendations from respective up-to-date clinical guidelines, lists of medications that have been issued black box warnings for monitoring, and the most current information, at the time, from the US Food and Drug Administration (FDA) website.8–26
The medications that required therapeutic/safety monitoring tests included: acenocoumarol, amiodarone, antiepileptics (carbamazepine, phenytoin, and valproic acid), oral antidiabetics, oral antifungals, antihypertensives, bisphosphonates, digoxin, immunosuppressants, isotretinoin, lithium, statins, and thyroid replacement therapy.
In a few cases where the frequency of therapeutic/safety monitoring recommendations was not consistent for a specific medication/class among different authorities, we adopted the longer time interval to assess completion of monitoring tests. For example, the American Society of Hypertension recommends self-monitoring of blood pressure (SMBP) on several days per week for patients in whom antihypertensive medication has been recently started or changed, and less frequently for more-stable patients.14 The New York City Department of Health and Mental Hygiene recommends adjusting monitoring-test frequency to complement patient self-management goals, varying from once a day to once a week.15 Hence, patients were considered completely monitored if they tested their blood pressure (BP) at least once weekly. It is of interest to highlight that warfarin is not available on the Lebanese market. Its use is substituted with acenocoumarol. The monitoring requirement for both is the same.8,9
Our study design included only the most commonly prescribed anticonvulsant agents in our community setting and did not expand to all antiepileptics. Along the same lines, the study design did not include antipsychotic medications except for lithium, considering that the majority of patients on such therapy benefit from the Lebanese Ministry of Public Health – National programs and therefore complete all therapeutic/safety monitoring tests recommended. Lithium is not covered under the provision of this program.
For reporting purposes, we defined 1) a patient with “Complete Monitoring Tests” (CoMT) as a patient who completed all recommended therapeutic/safety monitoring tests specific to their drug therapy, 2) a patient with “Partial Monitoring Tests” (PaMT) as a patient who completed some, but not all, of the recommended therapeutic/safety monitoring tests, and 3) a patient with “No Monitoring Tests” (NoMT) as a patient who did not complete any of the recommended therapeutic/safety monitoring tests. Those three terminologies have been used throughout to identify the completion rate of tests within a single disease condition, and per patient overall. Classification of the patients was completed and verified by two researchers to ensure its accuracy and transparency. These data were double checked and validated by an external reviewer.
Selection of participants
Participants were selected from all patients aged 18 years or older who visited the study site(s) from October 1–31, 2012. Participants were chosen if they received one or more of the chronic medications mentioned previously and agreed to participate in the study.
Questionnaire administration
Eligible patients were voluntarily subjected to a questionnaire designed to evaluate the completion rates of the therapeutic/safety monitoring tests indicated. The questionnaire collected information related to patient demographics, physician specialty, frequency of patient clinic visits, dates and frequency of monitoring tests, and time of treatment initiation. Licensed pharmacists were trained to interview the patients and collect the data.
Statistics
Data were collected and then entered into Microsoft Office Excel spreadsheet, and descriptive statistics were used to calculate and report the frequency distribution of patients maintained on each medication/medication class, frequency of patients’ clinic visits, and percentage of CoMT, PaMT, and NoMT.
Results
Study medications
The detailed list of the study medications, as well as their recommended therapeutic/safety monitoring parameters and respective frequencies, are listed in Table 1.
Patient demographics
Of 468 patients approached, 72 patients rejected participation due to time constraints and 112 patients did not meet the inclusion criteria (younger than 18 years of age; not receiving one or more of the chronic medications mentioned previously), giving a total response rate of 61%. Accordingly, a total of 284 outpatients were included in the analysis, and the majority (n=193; 68%) were of age below 65 years. Such age distribution is aligned with the US Central Intelligence Agency’s world factbook data.27
Patients surveyed were using antihypertensives (n=179; 63%), statins (n=106; 37%), oral antidiabetics (n=72; 25%), thyroid replacement therapy and bisphosphonates (n=24; 9% each), insulin (n=19; 7%), antiepileptics, oral antifungals, and acenocoumarol (n=12; 4% each), and other medications (n=9; 3%). Among those, 139 patients (49%) were recorded to be on two or more medication classes, while no patient was reported to be on digoxin, fibrates, and phenytoin therapy. Detailed results are shown in Table 2.
  | Table 2 Patient characteristics |
The majority of drug prescribers were cardiologists (n=144; 51%), followed by endocrinologists (n=94; 33%) and general practitioners (n=29; 10%). It is interesting to note that 14% (n=41) of patients had multiple prescribers, with 11% (n=31) having had two specialist prescribers and 4% (n=10) having had both a specialist and general practitioner. Around 3% (n=9) of patients reported to have had their drug dispensed by pharmacists without physician consultation.
Thirty-two percent of the patients (n=90) did not visit their physician for more than a year, whereas 16% (n=45) visited their physician every 3 months. The clinic visit interval was reported as “not applicable” for patients whose medications were dispensed by pharmacists without physician consultation (n=9; 3%).
Chronic medications monitoring results
The majority of patients (65%; n=185) were found to be PaMT for all the medications they were taking, while 27% (n=76) were CoMT and 8% (n=23) did not complete any of the recommended monitoring tests (NoMT) (Tables 3 and 4).
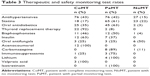  | Table 3 Therapeutic and safety monitoring test rates |
Among patients with incomplete therapeutic/safety monitoring (PaMT and NoMT combined; n=208), 57% (n=119) had two or more medical conditions, 47% (n=97) visited their physicians on a yearly basis or less frequently, and 31% (n=64) received prescriptions and follow-ups from nonspecialist prescribers. Indeed, incomplete monitoring was reported by 80% (n=64) of the patients who had received their prescriptions and follow-ups from nonspecialist prescribers. Around 42.5% of patients (n=76) taking antihypertensive medications were classified as CoMT, as their BP was monitored at a once-weekly interval or more frequently (Table 2). Another 42.5% (n=76) were found to be PaMT since they monitored their BP less frequently than every week and the remaining 15% (n=27) did not complete any SMBP (NoMT).
In contrast, 17% (n=18) of patients on statin therapy were reported to be CoMT, while 61% (n=65) and 22% (n=23) were PaMT and NoMT, respectively.
Thirty-five percent of patients (n=25) taking oral antidiabetics were classified as CoMT as they reported completing a baseline and periodic glycosylated hemoglobin (HbA1c) test every 6 months or more frequently. Around 63% (n=45) were considered PaMT because they missed the baseline HbA1c test or performed it less frequently than recommended, while only two patients were NoMT.
Interestingly, insulin therapy patients had higher rates of monitoring-test completion overall, as 63% (n=12) were CoMT. These patients reported completing a baseline and periodic HbA1c test at least every 6 months, and self-monitoring of blood glucose (SMBG) at least three times daily. A proportion of insulin therapy patients (37%; n=7) were PaMT because they either missed the periodic HbA1c test or completed the SMBG less frequently than recommended.
On the contrary, the majority of patients taking thyroid supplement (92%; n=22) were CoMT, as they reported completing a thyroid stimulating hormone/thyroxine test at baseline and yearly thereafter, while only 8% (n=2) were PaMT because they performed the test less frequently.
Forty-six percent (n=11) of patients on bisphosphonate therapy were classified as CoMT as they reported completing a dual-energy X-ray absorptiometry test at baseline and at least every 2 years thereafter. Fifty percent (n=12) were reported as PaMT because they missed the periodic dual-energy X-ray absorptiometry test or performed it less frequently, while only one patient did not undergo any monitoring tests at all (NoMT). It is noteworthy to mention that, among those who had incomplete monitoring tests (PaMT and NoMT), 62% (8 out of 13 patients) were visiting their physicians less frequently than once a year.
Among patients taking oral antifungal therapy, 25% (n=3) were reported to be CoMT, 25% (n=3) were PaMT, and 50% (n=6) did not complete any monitoring tests at all (NoMT). Fifty percent (n=6) of patients who took antifungal therapy were dispensed the medication from the pharmacist without a physician’s prescription.
Interestingly, all patients taking acenocoumarol (n=12) were CoMT, as they completed the international normalized ratio test 48 hours after the initial dose, every 2–4 days until stabilization, and monthly thereafter.
Discussion
In our study, 185 patients partially completed their monitoring tests, whereas only 76 patients were fully monitored. The present results were compared to those from other studies28–32 that assessed completion of recommended monitoring tests.
In fact, 85% (n=152) of the hypertensive patients in our study group reported SMBP, 42% (n=76) did it at least once weekly, and 49% (n=88) did self-monitoring at least once monthly. These results are similar to those obtained in a telephone survey among patients with hypertension, where 70% of patients were found to practice self-measurement.28 Furthermore, in a multicenter survey from six outpatient hypertension clinics in Italy, 75% of the participants performed home SMBP measurements at least once monthly.29 However, this is in contrast to another cross-sectional survey, where only 31% of patients with hypertension registered with primary care practices in the United Kingdom reported SMBP; of these, 60% self-monitored at least monthly and 13% at least weekly.30
Numerous recent guidelines and reviews highlight the importance of SMBP as a means to evaluate therapy, and as a key prognostic factor for cardiovascular risk.33–38 However, none of these references, and none of the recent guidelines for the management of hypertension,39–43 have recommended a determined frequency for the SMBP. Twice-daily SMBP has been strongly recommended for patients with resistant hypertension.35,44 Duplicate twice-daily SMBP has also been recommended only for 7 consecutive days for confirmation of hypertension diagnosis, as complementary to ambulatory BP monitoring. Both of the aforementioned conditions are beyond the scope of this study.36,37,43
In our study groups, 35% (n=25) of the diabetic patients on oral medications adhered to the American Diabetes Association guidelines on frequency of HbA1c monitoring tests. These findings are lower than those reported in a study of 193 Type II diabetic patients in a rural family, where 51% of the study population adhered to these guidelines.31 This could be primarily due to the fact that 62% (n=29) of the diabetic patients who had incomplete monitoring tests (PaMT and NoMT combined) in our study visited their physician once yearly or less frequently.
Similarly, 64% (n=68) and 25% (n=27) of our patient population receiving statins completed their baseline liver function tests and creatine phosphokinase tests, respectively. From a different perspective, 65% (n=69) of patients who received statin therapy had periodic liver function tests measured at least once during the follow-up. These results closely align with those reported by Tragni et al32 where the prevalence of safety laboratory-monitoring tests necessary for statin therapy, prescribed by Italian general practitioners, was 8.5% and 37.8% for the creatine phosphokinase test, 50.9% and 60.3% for the aspartate aminotransferase test, and 53.9% and 64.4% for the alanine aminotransferase test at baseline and during follow-up, respectively.
It is noteworthy to mention that in our study, completed in 2011, a patient on statin therapy must monitor baseline and yearly liver function tests and baseline creatine phosphokinase to be considered CoMT as per the American College of Cardiology/American Heart Association/National Heart, Lung and Blood Institute 2002 clinical advisory on use and safety of statins.25 However, the US FDA issued revised labels and new safety warnings for statins in February 2012.45 The new labels only recommend baseline liver function testing, and to only repeat such testing for clinical indications, rather than periodically thereafter. Hence, routine/periodic monitoring of liver enzymes for statin users is no longer needed.45 Accordingly, the percentages of CoMT, PaMT, and NoMT participants in our study were recalculated under these new guidelines as follows: 25%, 52% and 22%, respectively.
Our data collected for patients on antiepileptics, immunosuppressants, lithium, and isotretinoin did not have enough power to generate any relevant conclusion or recommendation. Moreover, our results indicate that 3% of patients have had their antifungal drugs dispensed by pharmacists without physician consultation, and for these patients, the clinic-visit interval was reported to be not applicable. Unfortunately, patients in the Lebanese community can acquire most prescription medications, excluding psychotropic drugs, narcotics, cocaine, and other highly addictive substances, without a physician’s prescription. This is mainly due to the absence of law application and reinforcement. Although the number of individuals surveyed in this category was small, lack of monitoring of these patients could potentially lead to rare but serious liver toxicity.
Interventions to increase awareness and improve adherence of physicians and patients to the recommended therapeutic/safety monitoring tests are also needed. In fact, adherence to the required monitoring tests is a multifaceted issue that requires cooperation between the patient and health care providers involved. Patients need the knowledge, attitudes, and means to appropriately complete all recommended therapeutic/safety monitoring tests and to sequentially have the behavior to intentionally or nonintentionally adhere to pharmacotherapy.46 In a study aiming to explore the barriers and facilitators to SMBG in type 2 diabetes patients using insulin, barriers identified included the perception that SMBG was only for insulin titration, fear of needles and pain, cost of test strips and needles, as well as lack of knowledge and self-efficacy.47
Similarly, physicians, particularly nonspecialists, need to follow updated and current guidelines in recommending therapeutic/safety monitoring tests, particularly its indicated frequency. They also need to ensure that patients understand the reason and importance for therapeutic/safety drug monitoring.48 In fact, a study assessing the perception of laboratory monitoring by physicians in practice suggested varying opinions among practitioners for its necessity, especially for medications perceived to be low-risk for adverse effects. They also expressed their inability to track the progress of laboratory tests that they had ordered and recommended for patients.49
Several approaches can be adopted to increase patient completion rates for monitoring tests, such as attending patient education programs. In a cross-sectional study carried out in 15,000 patients with diabetes, diabetes education center attendance was associated with improved SMBG (adjusted odds ratio =6.45 [95% confidence interval =5.61–7.42], P<0.0001).50
Technology developments, such as the use of point-of-care testing medical devices, present increasing opportunities for monitoring to occur outside hospitals or clinics.51 The use of widely available communications technologies, such as electronic medical record reminders to the prescribing health care professional and automated voice messages to the patient, were also effective in increasing laboratory monitoring when initiating new medications in primary care.52,53
Study limitations
This study has the following potential limitations that should be considered.
Firstly, we could not identify whether tests have not been ordered by physicians or whether they were ordered but not performed. Hence, it was not possible to separate physicians’ inadequate follow-up from patient nonadherence with recommended tests, nor to identify possible reasons behind the incomplete monitoring tests, such as patients’ socioeconomic status.
Many of the patients who were admitted in our study presented with their laboratory tests’ results or prescriptions for the next scheduled follow-up visit; however, data collection may still be subject to recall bias, as the study relied on patient recall to determine the completion of some of the therapeutic/safety monitoring tests.
Moreover, it was beyond the scope of our study to assess clinical conditions such as recent initiation of medications, dose adjustments, or achievement of therapeutic goals as judged by clinician’s discretion; hence, these situations were not addressed in our questionnaire. This might have implications in the results of some drug classes, particularly antihypertensives and antidiabetics. Consequently, this study assessed monitoring of all antihypertensives, as a class, by the completion of SMBP alone, in an attempt to maintain the objectivity of the data and minimize complexity of the parameters’ condition.
To the best knowledge of the authors, the present study is the first to address such a topic in the Lebanese community and in the (Middle East) region. In the absence of national consensus clinical guidelines, the evaluation of the therapeutic/safety monitoring tests in our study participants was benchmarked to international evidence-based guidelines that are recognized in Lebanese practice. This may help to strengthen the external validity of this study.
The authors also believe that this study identified potential risk factors behind incomplete monitoring, which included patients with two or more medical conditions, patients visiting their physicians on a yearly basis or less frequently, and patients receiving their prescriptions from nonspecialist prescribers. Future studies may be needed to identify characteristics associated with patient monitoring rates, and to further examine these risk factors in terms of achieving guideline-recommended monitoring. Furthermore, future studies can also assess the economic and health burden of incomplete therapeutic/safety test monitoring results and its potential impact on health care costs.
Conclusion
Seventy-three percent of the study group were receiving incomplete therapeutic and safety monitoring tests recommended for patients on chronic medications in the Lebanese community. Patients were categorized into completely monitored (27%), partially monitored (65%) or not monitored at all (8%).
While the completion rates of monitoring tests in our study were similar to those obtained from other reports, the present results identified the various types of medications that require therapeutic/safety monitoring tests and their completion rates for each class or type of medication. Patients need to better understand the importance of recommended test monitoring for the safe and effective use of their medications.
Further research is needed to determine the consequent clinical implications. Measures should also be taken to further educate prescribers about medication-safety updates and the importance of completion of the recommended therapeutic and safety monitoring tests.
Acknowledgment
We would like to acknowledge Maria Salman for her contribution in the data collection.
Author contributions
Elsy Ramia and Rony Zeenny have equal contribution in this work, and this is based on:
- Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data;
- Drafting the article or revising it critically for important intellectual content;
- Final approval of the version to be published; and
- Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure
The authors report no conflicts of interest in this work. The ideas expressed in this manuscript are those of the authors and in no way represent the position of the Lebanese American University or the School of Pharmacy, Byblos, Lebanon. No sources of funding were used to assist in the preparation of this study.
References
Hurley JS, Roberts M, Solberg LI, et al. Laboratory safety monitoring of chronic medications in ambulatory care settings. J Gen Intern Med. 2005;20(4):331–333. | ||
Gandhi TK, Weingart SN, Borus J, et al. Adverse drug events in ambulatory care. N Engl J Med. 2003;348(16):1556–1564. | ||
Gurwitz JH, Field TS, Harrold LR, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA. 2003;289(9):1107–1116. | ||
Gurwitz JH, Field TS, Judge J, et al. The incidence of adverse drug events in two large academic long-term care facilities. Am J Med. 2005; 118(3):251–258. | ||
Raebel MA, Lyons EE, Andrade SE, et al. Laboratory monitoring of drugs at initiation of therapy in ambulatory care. J Gen Intern Med. 2005;20(12):1120–1126. | ||
Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000. | ||
World Health Organization. The Importance of Pharmacovigilance: Safety Monitoring of Medicinal Products. Geneva, Switzerland: World Health Organization; 2002. Available from: http://apps.who.int/medicinedocs/en/d/Js4893e.html. Accessed June 24, 2014. | ||
Agence Nationale de Sécurité du Médicament et des Produits de Santé (ANSM). Anti-Vitamine K (AVK). Saint-Denis, France: ANSM; 2014. Available from: http://ansm.sante.fr/Dossiers/Anti-vitamine-K-AVK/Information-pour-les-professionnels-de-sante/(offset)/2. Accessed June 24, 2014. | ||
Hirsh J, Fuster V, Ansell J, Halperin JL; American Heart Association; American College of Cardiology Foundation. American Heart Association/American College of Cardiology Foundation guide to warfarin therapy. Circulation. 2003;107(12):1692–1711. | ||
Siddoway LA. Amiodarone: guidelines for use and monitoring. Am Fam Physician. 2003;68(11):2189–2196. | ||
Goldschlager N, Epstein AE, Naccarelli G, Olshansky B, Singh B. Practical guidelines for clinicians who treat patients with amiodarone. Practice Guidelines Subcommittee, North American Society of Pacing and Electrophysiology. Arch Intern Med. 2000;160(12):1741–1748. | ||
American Diabetes Association. Executive summary: standards of medical care in diabetes – 2011. Diabetes Care. 2011;34 Suppl 1:S4–S10. | ||
Glucophage®, Glucophage® XR (extended-release oral tablets, oral tablets) [package insert]. Princeton NJ: Bristol-Myers Squibb; 2009. | ||
Pickering T. Recommendations for the use of home (self) and ambulatory blood pressure monitoring. American Society of Hypertension Ad Hoc Panel. Am J Hypertens. 1996;9(1):1–11. | ||
Bloomberg MR, Frieden TR. Patient Self-Monitoring of Blood Pressure: A Provider’s Guide. New York, NY: The New York City Department of Health and Mental Hygiene; 2014. Available from: http://www.nyc.gov/html/doh/downloads/pdf/csi/hyperkit-hcp-bpselfmon-guide.pdf. Accessed June 24, 2014. | ||
Watts NB, Bilezikian JP, Camacho PM, et al; AACE Osteoporosis Task Force. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the diagnosis and treatment of postmenopausal osteoporosis. Endocr Pract. 2010;16 Suppl 3:1–37. | ||
National Institute for Health and Clinical Excellence. Bipolar Disorder: the Management of Bipolar Disorder in Adults, Children and Adolescents, in Primary and Secondary Care. Manchester, UK: National Institute for Health and Clinical Excellence; 2006. Available from: http://www.nice.org.uk/guidance/cg38/resources/guidance-bipolar-disorder-pdf. Accessed June 24, 2014. | ||
Tegretol® (oral chewable tablets, tablets, suspension) [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2007. | ||
Epocrates. Cyclosporine modified: black box warnings [webpage on the Internet]. San Mateo, CA: Epocrates; 2014. Available from: https://online.epocrates.com/u/10b4183/cyclosporine+modified/Black+Box+Warnings. Accessed June 24, 2014. | ||
Sandimmune® (oral capsules, oral solution, intravenous injection) [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2010. | ||
National Institute for Health and Clinical Excellence. Chronic Heart Failure: Management of Chronic Heart Failure in Adults in Primary and Secondary Care. Manchester, UK: National Institute for Health and Clinical Excellence; 2010. Available from: http://www.nice.org.uk/guidance/cg108/resources/guidance-chronic-heart-failure-pdf. Accessed June 24, 2014. | ||
Goldsmith LA, Bolognia JL, Callen JP, et al; American Academy of Dermatology. American Academy of Dermatology Consensus Conference on the safe and optimal use of isotretinoin: summary and recommendations. J Am Acad Dermatol. 2004;50(6):900–906. | ||
Rodgers P, Bassler M. Treating onychomycosis. Am Fam Physician. 2001;63(4):663–672, 677–678. | ||
Dilantin® (extended phenytoin sodium capsules, USP) [package insert]. New York, NY: Pfizer Inc; 2009. | ||
Pasternak RC, Smith SC, Bairey-Merz CN, Grundy SM, Cleeman JI, Lenfant C; American College of Cardiology; American Heart Association; National Heart, Lung and Blood Institute. ACC/AHA/NHLBI clinical advisory on the use and safety of statins. J Am Coll Cardiol. 2002;40(3):567–572. | ||
Demers LM, Spencer CA. The National Academy of Clinical Biochemistry Laboratory Medicine Practice Guidelines. Laboratory Support for the Diagnosis and Monitoring of Thyroid Disease. Washington, DC: National Academy of Clinical Biochemistry; 2002. Available from: http://www.aacc.org/SiteCollectionDocuments/Archived%20and%20Historical/ThyroidArchived2010.pdf#page=1. Accessed June 24, 2014. | ||
Central Intelligence Agency. The world factbook (webpage on the Internet]. Washington, DC: US Central Intelligence Agency; 2014 [updated June 20, 2014]. Available from: https://www.cia.gov/library/publications/the-world-factbook/geos/le.html. Accessed June 24, 2014. | ||
Krecke HJ, Lütkes P, Maiwald M. Patient assessment of self-measurement of blood pressure: results of a telephone survey in Germany. J Hypertens. 1996;14(3):323–326. | ||
Cuspidi C, Meani S, Lonati L, et al; Lombardy Regional Section of the Italian Hypertension Society. Prevalence of home blood pressure measurement among selected hypertensive patients: results of a multicenter survey from six hospital outpatient hypertension clinics in Italy. Blood Press. 2005;14(4):251–256. | ||
Baral-Grant S, Haque MS, Nouwen A, Greenfield SM, McManus RJ. Self-monitoring of blood pressure in hypertension: a UK primary care survey. Int J Hypertens. 2012;2012:582068. | ||
Parcero AF, Yaeger T, Bienkowski RS. Frequency of monitoring hemoglobin A1C and achieving diabetes control. J Prim Care Community Health. 2011;2(3):205–208. | ||
Tragni E, Filippi A, Mazzaglia G, Sessa E, Cricelli C, Catapano AL. Monitoring statin safety in primary care. Pharmacoepidemiol Drug Saf. 2007;16(6):652–657. | ||
Kjeldsen SE, Aksnes TA, Ruilope LM. Clinical implications of the 2013 ESH/ESC hypertension guidelines: targets, choice of therapy, and blood pressure monitoring. Drugs R D. 2014;14(2):31–43. | ||
Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111(5):697–716. | ||
Calhoun DA, Jones D, Textor S, et al; American Heart Association Professional Education Committee. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation. 2008;117(25):e510–e526. | ||
Parati G, Stergiou GS, Asmar R, et al; ESH Working Group on Blood Pressure Monitoring. European Society of Hypertension guidelines for blood pressure monitoring at home: a summary report of the Second International Consensus Conference on Home Blood Pressure Monitoring. J Hypertens. 2008;26(8):1505–1526. | ||
Parati G, Stergiou G, O’Brien E, et al; European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014;32(7): 1359–1366. | ||
O’Brien E, Parati G, Stergiou G. Ambulatory blood pressure measurement: what is the international consensus? Hypertension. 2013;62(6): 988–994. | ||
James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–520. | ||
Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Practice Guidelines for the Management of Arterial Hypertension. Blood Press. 2014;23(1):3–16. | ||
Doyle-Campbell C. European Society of Hypertension and European Society of Cardiology guidelines and the muted enthusiasm for home blood pressure monitoring. Hypertension. 2014;63(2):e5. | ||
Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens. 2014;32(1):3–15. | ||
Jaques H; National Institute for Health and Clinical Excellence (NICE). NICE guideline on hypertension. Eur Heart J. 2013;34(6):406–408. | ||
Vongpatanasin W. Resistant hypertension: a review of diagnosis and management. JAMA. 2014;311(21):2216–2224. | ||
US Food and Drug Administration. FDA drug safety communication: important safety label changes to cholesterol-lowering statin drugs [webpage on the Internet]. Silver Spring, MD: US Food and Drug Administration; 2012. Available from: http://www.fda.gov/Drugs/DrugSafety/ucm293101.htm. Accessed June 24, 2014. | ||
Kjeldsen LJ, Bjerrum L, Herborg H, Knudsen P, Rossing C, Søndergaard B. Development of new concepts of non-adherence measurements among users of antihypertensives medicines. Int J Clin Pharm. 2011;33(3):565–572. | ||
Ong WM, Chua SS, Ng CJ. Barriers and facilitators to self-monitoring of blood glucose in people with type 2 diabetes using insulin: a qualitative study. Patient Prefer Adherence. 2014;8:237–246. | ||
Haynes RB, Montague P, Oliver T, McKibbon KA, Brouwers MC, Kanani R. Interventions for helping patients to follow prescriptions for medications. Cochrane Database Syst Rev. 2000;(2):CD000011. | ||
Goldman RE, Soran CS, Hayward GL, Simon SR. Doctors’ perceptions of laboratory monitoring in office practice. J Eval Clin Pract. 2010; 16(6):1136–1141. | ||
Millar A, Cauch-Dudek K, Shah BR. The impact of diabetes education on blood glucose self-monitoring among older adults. J Eval Clin Pract. 2010;16(4):790–793. | ||
Shah SG, Barnett J, Kuljis J, Hone K, Kaczmarski R. Factors determining patients’ intentions to use point-of-care testing medical devices for self-monitoring: the case of international normalized ratio self-testing. Patient Prefer Adherence. 2013;7:1–14. | ||
Feldstein AC, Smith DH, Perrin N, et al. Improved therapeutic monitoring with several interventions: a randomized trial. Arch Intern Med. 2006;166(17):1848–1854. | ||
Hoch I, Heymann AD, Kurman I, Valinsky LJ, Chodick G, Shalev V. Countrywide computer alerts to community physicians improve potassium testing in patients receiving diuretics. J Am Med Inform Assoc. 2003;10(6):541–546. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


