Back to Journals » Clinical Ophthalmology » Volume 13
Comparison of tolerance to induced astigmatism in pseudophakic eyes implanted with small aperture, trifocal, or monofocal intraocular lenses
Authors Ang RE
Received 13 March 2019
Accepted for publication 6 May 2019
Published 30 May 2019 Volume 2019:13 Pages 905—911
DOI https://doi.org/10.2147/OPTH.S208651
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Robert Edward Ang
Department of Cornea and Refractive Surgery, Asian Eye Institute, Makati City, Philippines
Purpose: To compare the effect of induced astigmatic defocus on visual performance in pseudophakic eyes implanted with a small aperture, trifocal, or monofocal intraocular lens (IOL).
Patients and methods: The study included 44 eyes with one of four types of IOL (IC-8 IOL (AcuFocus Inc., USA); FineVision (PhysIOL SA, Belgium); AT Lisa (Carl Zeiss AG, Germany); and enVista monofocal (Bausch & Lomb, USA). For astigmatic tolerance assessment, monocular distance visual acuity was measured with cylindrical lenses (power range=0.00–2.50 diopters (D) in 0.50 D increments) added to the subjects best-corrected distance manifest refraction. The assessment was repeated on three pre-determined axes (90°, 180°, and either 45° or 135°). The magnitude of astigmatic tolerance at each defocus step was assessed by taking the difference between logMAR visual acuity at the defocus step relative to that at 0.0 D (ie, no defocus condition).
Results: Across all three axes, the reduction of mean monocular visual acuity at all defocus levels relative to no defocus was significantly smaller in IC-8 group compared to the other IOL groups. When the data was combined across all axes, the astigmatic tolerance of the IC-8 group was better than AT Lisa group from 0.50 D to 2.50 D and FineVision group from 0.50 D to 1.50 D (all P<0.05, ANOVA). The IC-8 group was better than the enVista group, but not significantly (P>0.05, ANOVA). Among individual orientations, statistically significant differences were seen between IC-8 IOLs and the other IOLs, with the largest difference being in the oblique axis. Astigmatic tolerance at all axes combined was 1.40 D for IC-8 IOL, 0.70 D for AT Lisa and FineVision, and 1.00 D for enVista IOLs.
Conclusion: The small aperture IC-8 IOL showed greater tolerance to induced astigmatic defocus compared to trifocal and monofocal IOLs.
Keywords: cataract, refractive error, small aperture IOL, residual astigmatism
Introduction
Spectacle independence is a key expectation in patients undergoing premium intraocular lens (IOL) implantation.1 Refractive misses with presbyopia-correcting IOLs can cause residual ametropia, resulting in reduced vision and patient satisfaction.2 Forty percent of the cataract population presents with corneal toricity of 0.75 D or more and, for eyes with greater than 0.50 D of corneal astigmatism, a toric IOL may be needed.3,4 When spectacle independence is desired after cataract surgery, the options for management of preoperative corneal or postoperative residual astigmatism include limbal relaxing incisions, toric IOLs for higher degrees of astigmatism, laser in situ keratomileusis (LASIK), photorefractive keratectomy (PRK), arcuate keratotomy, and piggy-back IOLs.5–9
Knowledge of the astigmatic tolerance of IOLs is, therefore, an essential component of surgical planning, as visual performance and patient satisfaction are affected when the magnitude of astigmatism is beyond the lenses limit of tolerance, requiring secondary management. The astigmatic tolerance limit of multifocal IOLs, in general, is estimated to be 0.75 D.10 A recent study compared the astigmatic tolerance of an extended depth of focus (EDOF) IOL with different multifocal IOLs. The EDOF IOL demonstrated a slightly better astigmatic tolerance of 1.00 D compared to that of bifocal IOLs at 0.75 D and trifocal IOL at 0.50 D.11
The IC-8 IOL is a small aperture IOL that provides an extended depth of focus which improves vision from far through near.12 Monocular implantation of the IC-8 IOL with a monofocal IOL in the fellow eye achieved uncorrected binocular visual acuities better than 20/20, 20/25, and 20/30 at distance, intermediate, and near, respectively.13 The extended depth of focus and the tolerance to residual refractive error is accomplished by the small aperture design, which effectively decreases the size of the blur circle, similar to that in the KAMRA inlay (CorneaGen, Seattle, WA, USA) that is approved by the US Food and Drug Administration for correction of presbyopia.14 The tolerance to residual astigmatism was evidenced in publications on clinical performance of the IC-8 IOL, which showed no significant difference in uncorrected visual acuities at far, intermediate, and near, between the eyes with ≤0.75 D of cylinder and the eyes with 0.76–1.50 D cylinder, with the mean difference in visual acuity being less than half a line.13 Additionally, in a recent publication we have shown that the eyes implanted with the IC-8 IOL were able to maintain 20/25 or better distance acuity with up to 1.50 D of induced astigmatic defocus.15 The objective of this prospective, comparative study was to investigate how increasing levels of induced astigmatic defocus influences visual performance in pseudophakic eyes implanted with small aperture vs trifocal and standard monofocal IOLs.
Methods
This was a prospective, single-center, comparative study of pseudophakic subjects from the Asian Eye Institute (Manila, Philippines). The study was performed in accordance with the Declaration of Helsinki and was approved by the Ethics Committee. All eligible subjects provided written informed consent for participation in the study.
Patients over the age of 40 years who were implanted with IC-8 IOL (AcuFocus Inc., Irvine, CA, USA), FineVision IOL (PhysIOL SA, Liège, Belgium), AT Lisa IOL (Carl Zeiss AG, Jena, Germany), or enVista IOL (Bausch & Lomb, Rochester, NY, USA) in at least one eye with best-corrected distance visual acuity (BCDVA) of 20/20 or better in that eye were included in the study. In addition, all subjects had manifest refraction sphere between −1.00 and +1.00 D, cylinder not exceeding 1.00 D, and clear ocular media in the study eye. Patients with any pathology that was predicted to cause a loss in BCDVA or diagnosis of dry-eye or dependency on ocular lubricating drops to maintain eye comfort or adequate vision were excluded.
Tolerance to induced astigmatism
One eye of each subject was used for the measurement of astigmatic tolerance; the right eye was used when both eyes qualified for the study. Baseline distance manifest refraction and BCDVA were recorded for the study eye, as the 0 D or no defocus condition. Astigmatic defocus was induced over the manifest distance refraction with plus cylinder from +0.50 D to +2.50 D in 0.50 D steps at three orientations (90°, 180°, and oblique at either 45° or 135°). For the oblique axis, defocus was induced at 135° when manifest refraction cylinder was between 0 and 90° and at 45° when manifest refraction cylinder was between 91° and 179°. A Landolt C Snellen chart was used to measure the visual acuity at each defocus step. All visual acuities were converted to logMAR acuity for data analysis. The magnitude of astigmatic tolerance at each defocus step was assessed by calculating the difference between logMAR visual acuity at the defocus step to that at 0 D or no defocus baseline.
Statistical analysis
Statistical analysis was performed using JMP® software (Version 13.0, SAS Institute Inc., North Carolina, USA). Snellen visual acuity was converted to logMAR, and then the magnitude of astigmatic tolerance was calculated at each defocus step for statistical analysis (mean and 95% confidence intervals) and comparisons between groups at defocus steps from 0.00 to 2.50 D for each astigmatic orientation using pairwise non-parametric Wilcoxon test and for all axes combined using ANOVA. Categorical variables between the IOL groups were compared using Fisher’s Exact Test. The non-parametric tests were chosen for being appropriate and efficient tests in comparing small sample sizes without a normal distribution assumption. The ANOVA test was chosen for the comparison between groups when all axes were combined for the sample sizes in this test and were close to or above 30 for each group. These tests are confirmed for their appropriateness from the data before being conducted. Differences were considered significant at P<0.05. Monocular astigmatic defocus curves were plotted as change in logMAR visual acuity vs defocus in diopters for each IOL group.
Results
Demographics and baseline characteristics
The study included 44 eyes of 44 subjects in the age range of 53–79 years, implanted with one of the four types of IOL in at least one eye. The IC-8 IOL group had 12 subjects; the FineVision IOL group had nine subjects; the AT Lisa IOL group had 10 subjects; and the enVista IOL group had 13 subjects. Table 1 shows summary statistics for subject demographics, photopic pupil size, baseline uncorrected distance visual acuity (UCDVA), best-corrected distance visual acuity (BCDVA), sphere, cylinder, manifest refractive spherical equivalent (MRSE), and postoperative time for each IOL group. There were no significant differences between the IOL groups on age, race, gender, UCDVA, BCDVA, cylinder, and photopic pupil size (all P>0.05, Fisher’s exact test or Wilcoxon test). Statistically significant differences were noted between groups on MRSE, sphere, and postoperative time (all P<0.05, Wilcoxon test).
 | Table 1 Subject demographics and baseline characteristics by IOL group |
Astigmatic tolerance
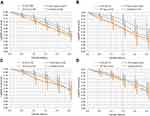
Figures 1A–D shows change in visual acuity from baseline (0 D or no defocus) at induced astigmatic defocus steps from 0.50 to 2.50 D for all four IOL groups, with all axes combined (Figure 1A) and at oblique (Figure 1B), 90° (Figure 1C), and 180° (Figure 1D) axes. With all axes combined, the IC-8 group showed a smaller decline in visual acuity with induced astigmatic defocus when compared to other IOL groups; the astigmatic tolerance in the IC-8 group was significantly better than the AT Lisa group for 0.50 D to 2.50 D of defocus and the FineVision group for 0.50 D–1.50 D of defocus (all P<0.05, ANOVA), and was not significantly better than the enVista group (P>0.05, ANOVA).
As shown in Figures 1A–D, the magnitude of change in visual acuity from baseline with induced astigmatic defocus was significantly less for IC-8 IOL eyes than FineVision IOL eyes; significant P-values are presented as follows: at 0.50 D, P=0.0005 and 0.0047 for all axes combined and oblique, respectively; at 1.00 D, P=0.0002, 0.0156, and 0.0188 for all axes combined, oblique, and 90°, respectively; at 1.50 D, P=0.0010 and 0.0189 for all axes combined and oblique, respectively; at 2.00 D, P=0.0236 for all axes combined; and at 2.5 D, P=0.0235 for all axes combined. Similarly, when compared to AT Lisa IOL eyes, the change in visual acuity from baseline in IC-8 IOL eyes was significantly less with induced astigmatic defocus of 0.50 D, P=0.0006 and 0.0012 for all axes combined and oblique, respectively, 1.00 D, P=0.0002 and 0.0010 for all axes combined and oblique, respectively, 1.50 D, P=0.0018 and 0.0014 for all axes combined and oblique, respectively, 2.00 D, P=0.0054 and 0.0110 for all axes combined and oblique, respectively, and 2.50 D, P=0.0004 and 0.0134 for all axes combined and oblique, respectively. The comparison of astigmatic tolerance between IC-8 IOL eyes and enVista monofocal IOL eyes was only significant at 1.50 D defocus in the oblique axis (P=0.0334).
On average, with 1.50 D of induced astigmatic defocus when all axes are combined, visual acuity decreased from baseline by 1.2 lines in the IC-8 group, 2.2 lines in the FineVision group, 2 lines in the AT Lisa group, and 1.7 lines in the enVista group. For 90° and oblique axes, at 2.50 D of defocus the IC-8 group was 1–1.5 lines better than the other three IOL groups. At 180° axis, the IC-8 group was about the same as the enVista group and was 0.5–1 line better than the trifocal IOL groups.
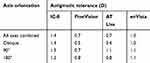
The mean astigmatic defocus range to maintain acuity with no more than one line of reduction from the 0 D or no defocus condition is presented in Table 2 for each IOL group. With all axes combined, the aforementioned astigmatic defocus range is 1.40 D for IC-8, 0.70 D for AT Lisa and FineVision, and 1.00 D for the enVista group. The largest difference in that astigmatic defocus range between IC-8 and trifocal eyes were noted for the oblique axis, with 1.4 D for the IC-8 group, and 0.50 D for the FineVision group and 0.40 D for the AT Lisa group. The smallest difference in that astigmatic defocus range between IC-8 and trifocal eyes were noted at 180°, with 1.2 D for the IC-8 group and 0.80 D for the FineVision and AT Lisa groups.
 | Table 2 Mean astigmatic defocus that resulted in one line of loss in visual acuity from the 0 D or no defocus condition for all IOL groups |
Discussion
In this study, the small aperture IOL showed larger tolerance to induced astigmatism when compared to the trifocal IOLs. On average, visual acuity was maintained with no more than one line of loss from baseline with induced astigmatic defocus up to 1.40 D in the IC-8 group, up to 1.00 D in the EnVista monofocal group, and up to 0.70 D in the trifocal (FineVision and AT Lisa) groups when all axes were combined. In a recently published pilot evaluation,15 similar tolerance to astigmatic defocus was shown for the IC-8 IOL eyes, in spite of methodological differences between the two studies. In the published pilot evaluation, astigmatic defocus was induced in the same axis as the manifest sphere-cylinder refraction of the IC-8 IOL eye and a tumbling E was used to assess visual acuities. Similarly, Dick et al13 compared visual acuity results by magnitude of postoperative residual astigmatism in a large European post-market study on the IC-8 IOL. IC-8 IOL eyes with up to 1.50 D of uncorrected residual astigmatism achieved mean uncorrected visual acuity of 20/22.13 Irrespective of the differences in testing and study population, the eyes implanted with the IC-8 IOL have shown a robust and consistent tolerance for up to 1.50 D of astigmatic defocus (induced or residual).
Among other presbyopia-correcting IOLs, the EDOF IOL (Tecnis Symfony ZRX00, Abbott Medical Optics, Santa Ana, CA, USA) has shown greater astigmatic tolerance than what is obtained with multifocal and trifocal IOLs. In a comparative prospective study, the astigmatic tolerance was determined to be 1.00 D with Symfony, 0.75 D with AcrySof ReSTOR IOL (Alcon Laboratories Inc., Fort Worth, TX, USA), and 0.50 D with Panoptix IOL (Alcon Laboratories Inc., Fort Worth, TX, USA).11 For 1.50 D of astigmatic defocus, the average loss in the number of lines from baseline visual acuity were three for multifocal, four lines for trifocal, and two lines for Symfony IOLs. In comparison, for up to 1.50 D of astigmatic defocus, IC-8 IOL eyes lost one line of visual acuity. Similarly, additional studies have shown up to 0.75 D of astigmatism tolerance with refractive (AMO Array, Allergan Medical Optics, CA, USA) and diffractive (AcrySof ReSTOR IOL SN6AD1 and SN6AD3, Alcon Laboratories Inc., Fort Worth, TX, USA) multifocal IOLs.16,17 The astigmatic tolerance of IC-8 IOL is higher than that of other EDOF, multifocal, and trifocal IOLs because of its small aperture design, which effectively decreases the size of the blur circle by blocking aberrated peripheral light rays. Computational eye modeling of astigmatic tolerance with a small aperture corneal inlay showed doubling of astigmatic tolerance from 1.00 D with a 3.00 mm aperture to 1.90 D with a 1.60 mm aperture in a series of 20 eyes.18
Among patients presenting for cataract surgery, nearly 80% have corneal astigmatism of 1.50 D or less, and 32% between 0.75 and 1.50 D, which represents the range outside the tolerance of multifocal IOLs and within that of the small aperture IOL.3,19 Even though toric EDOF and multifocal IOLs are an option for astigmatism management in patients seeking presbyopia correction, in the event of toric IOL misalignment, every degree of off-axis rotation results in a loss of up to 3.3% of IOL cylindrical power. This means, with a 10° off-axis rotation, one-third of the cylindrical effect would be lost.20 Additionally, the presence of residual astigmatism in patients implanted with presbyopia-correcting IOLs is a major factor for dissatisfaction. Sixty-four percent of patients with eyes with 1.0 D–1.50 D of residual astigmatism after multifocal implantation reported dissatisfaction due to complaints of blurry vision.2 The functional advantage of simultaneous focal points in multifocal IOLs is impeded by the interference of astigmatic focal lines between different foci.21 Gundersen et al22 showed a retreatment rate of 10.8% in eyes implanted with multifocal IOLs, and the eyes that required retreatment had significantly higher residual refractive astigmatism compared with those which did not require retreatment (1.21±0.51 D vs 0.51±0.39 D). Compensation of residual astigmatism and improved patient satisfaction, for correction of astigmatism as low as 0.50–0.75 D, has been shown to improve contrast and quality of vision.23,24
The broader tolerance to astigmatic defocus with the IC-8 IOL may provide a simpler approach to the management of astigmatism up to 1.50 D, obviating the need to determine precise axis placement, number of relaxing incisions, or additional surgical procedures.13,15 The increased astigmatic tolerance of IC-8 IOL also has the potential to be more robust to refractive surprises in postoperative astigmatism and to changes in corneal topography over time.25
The astigmatic tolerance data show that the change from baseline acuity for all the tested IOLs was greatest for astigmatism induced at the oblique axis and smallest at the 180° axis (with-the-rule). However, these small differences among orientations were not statistically significant at all defocus steps for the IC-8, FineVision and EnVista groups (all P>0.05, Wilcoxon test). Significant differences among orientations was observed at defocus steps 0.50 D (P=0.0352), 1.0 D (P=0.0419), and 1.50 D (P=0.0131) in the AT Lisa group. Orientation of astigmatism has a small effect on visual acuity, favoring with-the-rule astigmatism.26,27 Atchison et al27 reported higher levels of sensitivity to the detection of blur with against-the-rule than with-the-rule crossed cylinder astigmatism. In this study, visual acuity was measured using a Landolt C Snellen chart to minimize orientation bias. However, a larger sample size of subjects is required to confirm the true nature of the relationship between astigmatic tolerance and axis orientation.
One limitation of this study is the small group sizes (between nine and 13 subjects per group), which is why continuous parameters were compared between groups using the Wilcoxon Test for each orientation axis. The Wilcoxon test is a non-parametric test that does not have a normal distribution assumption. This attribute makes it more appropriate for small sample size comparisons, while still being an efficient test. On the other hand, under the premise that the Wilcoxon test is to compare if the distributions of two populations are different, only when big differences between the values of the two samples occur, then a small sample size might cause loss of information. In this study, the individual logMAR visual acuity values at different induced cylinder astigmatism levels were highly concentrated, which supports the use of the Wilcoxon test to examine the mean differences in the magnitude of astigmatic tolerance. And, when all axes were combined, the sample points were around or above 30 for each IOL group, warranting the use of the ANOVA test.
In summary, the subjects implanted with the small aperture extended depth of focus IC-8 IOL demonstrated better tolerance to induced astigmatism vs the other tested lenses, with the differences being significant vs the FineVision and AT Lisa IOLs. The IC-8 IOL group maintained good visual acuity with no more than one line of loss from baseline with up to 1.40 D of induced astigmatism when all axes were combined. The results of this study further demonstrate the ability of a small aperture IOL to manage preoperative or postoperative astigmatism and to provide an alternative to monofocal and presbyopia-correcting IOLs for correction of low-to-moderate magnitudes of astigmatism, especially in patients with oblique astigmatism.
Disclosure
Dr Robert Edward Ang is the clinical investigator of this study and a member of the AcuFocus’ medical advisory board. Dr Robert Edward Ang reports travel grants and speaking fees from AcuFocus, during the conduct of the study; and grants from Physiol, outside the submitted work.
References
1. de Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2016;12:CD003169. doi:10.1002/14651858.CD003091.pub4
2. de Vries NE, Webers CA, Touwslager WR, et al. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2011;37(5):859–865. doi:10.1016/j.jcrs.2010.11.032
3. Ferrer-Blasco T, Montés-Micó R, Peixoto-de-Matos SC, González-Méijome JM, Cerviño A. Prevalence of corneal astigmatism before cataract surgery. J Cataract Refract Surg. 2009;35(1):70–75. doi:10.1016/j.jcrs.2008.09.027
4. Villegas EA, Alcón E, Artal P. Minimum amount of astigmatism that should be corrected. J Cataract Refract Surg. 2014;40(1):13–19. doi:10.1016/j.jcrs.2013.09.010
5. Rubenstein JB, Raciti M. Approaches to corneal astigmatism in cataract surgery. Curr Opin Ophthalmol. 2013;24(1):30–34. doi:10.1097/ICU.0b013e32835ac853
6. Poll JT, Wang L, Koch DD, Weikert MP. Correction of astigmatism during cataract surgery: toric intraocular lens compared to peripheral corneal relaxing incisions. J Refract Surg. 2011;27(3):165–171. doi:10.3928/1081597X-20100526-01
7. Alio JL, Abdelghany AA, Fernández-Buenaga R. Management of residual refractive error after cataract surgery. Curr Opin Ophthalmol. 2014;25(4):291–297. doi:10.1097/ICU.0000000000000067
8. Macsai MS, Fontes BM. Refractive enhancement following presbyopia-correcting intraocular lens implantation. Curr Opin Ophthalmol. 2008;19(1):18–21. doi:10.1097/ICU.0b013e3282f14d9f
9. Sáles CS, Manche EE. Managing residual refractive error after cataract surgery. J Cataract Refract Surg. 2015;41(6):1289–1299. doi:10.1016/j.jcrs.2015.05.001
10. Braga-Mele R, Chang D, Dewey S, et al.,
11. Carones F. Residual astigmatism threshold and patient satisfaction with bifocal, trifocal and extended range of vision intraocular lenses (IOLs). Open J Ophthalmol. 2017;7(01):1. doi:10.4236/ojoph.2017.71001
12. Grabner G, Ang RE, Vilupuru S. The small aperture IC-8 intraocular lens: a new concept for added depth of focus in cataract patients. Am J Ophthalmol. 2015;160(6):1176–1184. doi:10.1016/j.ajo.2015.08.017
13. Dick HB, Piovella M, Vukich J, Vilupuru S, Lin L,
14. Vilupuru S, Lin L, Pepose JS. Comparison of contrast sensitivity and through focus in small aperture inlay, accommodating intraocular lens, or multifocal intraocular lens subjects. Am J Ophthalmol. 2015;160(1):150–162. doi:10.1016/j.ajo.2015.04.023
15. Ang RE. small aperture intraocular lens tolerance to induced astigmatism. Clin Ophthalmol. 2018;12:1659. doi:10.2147/OPTH.S172557
16. Hayashi K, Manabe S, Yoshida M, Hayashi H. Effect of astigmatism on visual acuity in eyes with a diffractive multifocal intraocular lens. J Cataract Refract Surg. 2010;36(8):1323–1329. doi:10.1016/j.jcrs.2010.02.016
17. Hayashi K, Hayashi H, Nakao F, Hayashi F. Influence of astigmatism on multifocal and monofocal intraocular lenses. Am J Ophthalmol. 2000;130(4):477–482.
18. Vilupuru A, Tabernero J, Artal P. Tolerance to astigmatism with a small aperture corneal inlay. Invest Ophthalmol Vis Sci. 2013;54(15):4280.
19. Khan MI, Muhtaseb M. Prevalence of corneal astigmatism in patients having routine cataract surgery at a teaching hospital in the United Kingdom. J Cataract Refract Surg. 2011;37(10):1751–1755. doi:10.1016/j.jcrs.2011.04.026
20. Novis C. Astigmatism and toric intraocular lenses. Curr Opin Ophthalmol. 2000;11(1):47–50. doi:10.1097/00055735-200002000-00007
21. Ravalico G, Parentin F, Baccara F. Effect of astigmatism on multifocal intraocular lenses. J Cataract Refract Surg. 1999;25(6):804–807.
22. Gundersen KG, Makari S, Ostenstad S, Potvin R. Retreatments after multifocal intraocular lens implantation: an analysis. Clin Ophthalmol. 2016;10:365–371. doi:10.2147/OPTH.S100840
23. Richdale K, Berntsen DA, Mack CJ, Merchea MM, Barr JT. Visual acuity with spherical and toric soft contact lenses in low- to moderate-astigmatic eyes. Optom Vis Sci. 2007;84(10):969–975. doi:10.1097/OPX.0b013e318157c6dc
24. Lehmann RP, Houtman DM. Visual performance in cataract patients with low levels of postoperative astigmatism: full correction versus spherical equivalent correction. Clin Ophthalmol. 2012;6:333–338. doi:10.2147/OPTH.S28241
25. Hashemi H, Asgari S, Emamian MH, Mehravaran S, Fotouhi A. Age-related changes in corneal curvature and shape: the Shahroud eye cohort study. Cornea. 2015;34(11):1456–1458. doi:10.1097/ICO.0000000000000595
26. Charman WN, Voisin L. Optical aspects of tolerances to uncorrected ocular astigmatism. Optom Vis Sci. 1993;70(2):111–117.
27. Atchison DA, Guo H, Charman WN, Fisher SW. Blur limits for defocus, astigmatism and trefoil. Vision Res. 2009;49(19):2393–2403. doi:10.1016/j.visres.2009.07.009
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.