Back to Journals » Journal of Hepatocellular Carcinoma » Volume 9
Comparison of the Efficacy and Safety of Transarterial Chemoembolization Plus Microwave Ablation versus Surgical Resection in Patients with Solitary Large Hepatocellular Carcinoma: A Propensity Score-Matched Analysis
Authors Zhang Y, Chen H, Chen S, Duan Y, Cheng L , Gao J, Li W
Received 15 August 2022
Accepted for publication 27 November 2022
Published 19 December 2022 Volume 2022:9 Pages 1309—1321
DOI https://doi.org/10.2147/JHC.S386264
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr David Gerber
Yongchao Zhang,1 Hualei Chen,1 Shanshan Chen,1 Youjia Duan,1 Long Cheng,1 Jie Gao,2,* Wei Li1,3,*
1Cancer Center, Beijing Ditan Hospital, Capital Medical University, Beijing, People’s Republic of China; 2Department of Hepatobiliary Surgery, Peking University People’s Hospital, Beijing, People’s Republic of China; 3Cancer Center, Beijing Tongren Hospital, Capital Medical University, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jie Gao, Department of Hepatobiliary Surgery, Peking University People’s Hospital, No. 11 Xizhimen South Street, Xicheng District, Beijing, 100044, People’s Republic of China, Email [email protected] Wei Li, Cancer Center, Beijing Ditan Hospital, Capital Medical University, 8 Jingshun East Street, Chaoyang District, Beijing, 100015, People’s Republic of China, Email [email protected]
Background: The liver resection for solitary large hepatocellular carcinoma (SLHCC) remains controversial due to the high risk of complications and recurrence after resection. This study aimed to compare the efficacy and safety of transcatheter arterial chemoembolization (TACE) plus microwave ablation (MWA) with resection for SLHCC.
Methods: We retrospectively analyzed a total of 148 patients who were treated with either TACE-MWA (n = 94) or resection (n = 54) for SLHCC (≥ 5 cm). A matched cohort composed of 86 patients was included after propensity score matching (PSM). The primary endpoint was overall survival (OS), and the secondary endpoints were progression-free survival (PFS) and safety.
Results: The TACE-MWA group was older with higher ALT and AST (all P < 0.05). After PSM, the 1-, 3-, and 5-year OS were 100%, 80.3%, and 51.0% in the TACE-MWA group, and 88.3%, 66.7%, and 39.4% in the liver resection group, respectively. The 1-, 3-, and 5-year PFS were 76.7%, 48.8%, and 19.6% in the TACE-MWA group, and 72%, 40.2%, and 22.6% in the liver resection group, respectively. There was no significant difference in OS and PFS between the two groups (all P > 0.05). For SLHCC patients with tumor size ≥ 7cm, TACE-MWA showed favorable OS than liver resection. The TACE-MWA group exhibited a lower rate of major complications and shorter hospital stay than the resection group.
Conclusion: TACE-MWA showed comparable efficacy to liver resection in patients with SLHCC, but better safety and shorter hospital stay. TACE-MWA might provide a longer OS than liver resection for SLHCC patients with tumor size ≥ 7cm.
Keywords: transarterial embolization, microwave ablation, hepatocellular carcinoma, liver resection
Introduction
Worldwide, hepatocellular carcinoma (HCC) is the sixth most common malignancies, with nearly 906,000 new cases and 830,000 deaths in 2020.1 China is responsible for nearly half of the global morbidity and mortality, where solitary large HCC (SLHCC) (maximal diameter >5 cm) has a higher incidence compared with other countries.2 This is potentially explained by the different aetiology of HCC, no obvious symptoms in the early stage, limited awareness of early screening, and poor economic conditions.3 As per the Barcelona Clinic Liver Cancer (BCLC) staging system, although SLHCC without macrovascular invasion and/or extrahepatic spread is classified in the early stage where patients can benefit from curative therapies such as liver resection, liver transplantation or thermal ablation, the optimal therapies for SLHCC remain controversial.4–7
Liver resection is the preferred option for patients with early-stage HCC, but SLHCC occupying more space may compromise liver function seriously and often invade the surrounding tissues, which amplifies the risk of surgery.3,8 Furthermore, postoperative complications and long-term risk of recurrence are still the main challenges in patients with SLHCC.9 Liver transplantation has worse outcomes in SLHCC patients compared with those with small HCC due to tumor size beyond Milan criteria (single tumor ≤5 cm or ≤3 tumors each ≤3 cm).10 Ablation, mainly radiofrequency ablation (RFA) and microwave ablation (MWA), is recommended in patients who are not candidates for resection, with a higher local recurrence than the resection, especially in patients with large tumor.11,12 Transcatheter arterial chemoembolization (TACE) has been widely used in large HCC. However, due to TACE as a palliative treatment, complete tumor necrosis is rarely achieved in one session and residual tumors often exist in large HCC.13
Currently, the combination of TACE with ablation has shown better efficacy as compared to either alone.14–16 TACE can decrease the heat-sink effect, which may compromise the efficacy of ablation by reducing the arterial blood flow to the tumor, and combined therapy provides a larger ablation area than ablation alone.17 Therefore, TACE combined with ablation has been widely used in the management of HCC. Recently, a meta-analysis showed no significant differences in terms of overall survival (OS) and progression between the TACE plus RFA groups and liver resection group when only the propensity-matched data were evaluated.18
MWA, theoretically, can achieve larger ablation zones with higher temperatures than RFA.19 Furthermore, a meta-analysis comparing TACE combined with RFA or MWA demonstrated that the superiority of TACE plus MWA was mainly reflected in patients with larger tumors (≥3 cm).20 Given TACE plus MWA seems to be a more effective therapy than TACE plus RFA for large HCC, with better survival outcomes and similar safety, we thus performed this study to compare the survival and safety outcomes between TACE-MWA and liver resection for the treatment of SLHCC.
Materials and Methods
Patients
This study was conducted in line with the Declaration of Helsinki, and written informed consent was obtained from all the eligible patients before treatment. Clinical research protocol and clinical data were approved by the Ethics Committee of Beijing Ditan Hospital (KY2020-030).
The medical records of HCC patients treated with TACE with MWA and liver resection between September 2008 and December 2019 were retrospectively examined. The following eligibility criteria were included (i) patients with HCC confirmed by pathological or radiological examination, (ii) age ranges >18 years, (iii) solitary HCC tumor >5 cm in diameter, (iv) liver function indicated by Child-Pugh grade A or B, with <25% retention of indocyanine green 15 min after injection (v) treatment by surgical resection or TACE-MWA, and suitability for the other therapies in a re-evaluation by our multidisciplinary teams; (vi) no history of other malignancies, (vii) Eastern Cooperative Oncology Group performance status 0. The criteria of exclusion included (i) macrovascular invasion or extrahepatic metastasis, (ii) severe chronic condition (eg, heart failure), (iii) insufficient residual liver volume, (iv) esophageal or gastric variceal bleeding, (v) hepatic encephalopathy, (vi) severe coagulation disorders, (vii) prior history of any treatment except TACE.
Clinical information including age, sex, date of diagnosis, tumor size, date of death, etiology of HCC, cirrhosis, antiviral treatment, pre-TACE, alpha-fetoprotein (AFP), albumin (ALB), alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin (TBIL), Child-Pugh grade, neutrophil counts, lymphocyte counts platelet (PLT) counts, international normalized ratio (INR) and follow-up results were collected.
Neutrophil to lymphocyte (NLR) was calculated by dividing the neutrophil count by the lymphocyte count. Its cutoff value was determined by the maximally selected rank statistics in all patients.21 ALBI score = (log10 bilirubin [µmol/L] × 0.66) + (albumin [g/L] × −0.0852). ALBI grades were stratified as follows: ALBI score ≤ −2.60 (ALBI grade 1), > −2.60 to ≤ −1.39 (ALBI grade 2), and > −1.39 (ALBI grade 3).22
Treatment Strategies
The decision to whether perform surgical resection or TACE+MWA for individual patients was determined by multidisciplinary team (MDT) meetings and each patient’s preference.
TACE Plus MWA Procedure
TACE was performed by two radiologists in our cancer center, with more than 10 years of experience in interventional radiology. Patients were under local anesthesia with 1% lidocaine. A 5-F catheter was introduced through the femoral artery, and the survey of tumor feeding arteries was performed. Distal superselective 5-F catheterization of tumor-feeding hepatic arteries with Embosphere microspheres (300–500 mm; Biosphere Medical Inc., Rockland, MA), lipiodol (5–20 mL) (Lipiodol Ultra-Fluide; André Guerbet Laboratories, AulnaySous-Bois, France), and epirubicin (50 mg) (Pharmorubicin; Pfizer, Wuxi, China). Repeated TACE was performed if the viable tumor or intrahepatic recurrences were detected by CT/MRI. MWA was performed 3–14 days after TACE. Two cooled-shaft microwave systems (KY-2000, Kangyou Medical, Nanjing, China) with frequencies of 2450 MHz and 915 MHz were used with two generators, both capable of producing 1–100 W of power. The antennae were percutaneously inserted into the tumor and placed at a designated location under CT guidance. A power output of 50–60 W was routinely used during MWA. Completed ablation was considered as the heat-generated hyperechoic water vapor completely encompassing the entire tumor with no enhancement in the CT image. The tumor response was assessed one month later using CT and/or MRI.
Liver Resection Procedure
All included patients in the liver resection group were performed by experienced surgeons under general anesthesia. Preoperative CT/MRI was routinely used to evaluate the tumor extent, the liver remnant, and the resection margin. The detailed surgical protocol was according to tumor location, hepatic functional reserve, and residual liver content. All procedures of liver resection are according to the standard procedures recommended by the guidelines.5
Follow-Up and Outcomes
Routine radiological examinations and laboratory tests were performed at 1 month, 3 months, and then every 6 months after treatment. The primary endpoint of this study was overall survival (OS), which was calculated from the date of HCC treatment to death from any cause or the time of the last follow-up by December 31, 2021. The secondary endpoint was progression-free survival (PFS), which was defined from the date of treatment until tumor progression, death from any cause, or the last visit by December 31, 2021. Other outcomes included the major complications (major complications were defined as an event that resulted in disability or morbidity and caused a hospital admission or prolonged the length of hospital stay). If tumor recurrence is identified, subsequent treatments will include resection, MWA, TACE, targeted therapies, and immunotherapies after discussion by MDT.
Statistical Analysis
Categorical variables were presented as a frequency (%) and analyzed by Chi-square or Fisher exact tests. Continuous variables were represented as mean ± standard deviation (SD) or median (interquartile range [IQR]) and analyzed by Student’s t-test or Mann–Whitney U-test. Moreover, we perform propensity score-matching analyses (PSM) using logistic regression to reduce the potential selection bias and the influence of confounding factors, with covariates including sex, age, etiology, cirrhosis, ALT, AST, TBIL, tumor size, pre-TACE, and platelet counts. TACE-MWA group and surgical resection group were matched 1:1 using the nearest neighbor matching method (caliper = 0.1). Kaplan–Meier analysis was used to compare the OS and PFS between groups and the difference was compared by Log rank test. Univariate and multivariate Cox regression analyses were used to identify independent prognostic factors of OS and PFS. P < 0.05 was considered statistically significant. All statistical analyses were performed using R Software version 4.1.1 (R Package for Statistical Computing; www.r-project.org).
Results
Patient Characteristics
Finally, 148 patients with SLHCC treated by TACE-MWA or liver resection were included in this study (Figure 1). Patients in the TACE-MWA group were older and had higher ALT and AST than those in the liver resection group. There were no significant differences in baseline characteristics between the TACE-MWA group and the liver resection group except for age, ALT, and AST. In the TACE-MWA group, a total of TACE treatment was used 329 times (average: 3.5 times/case) and a total of ablations were conducted 196 times (average: 2.08 times/case).
 |
Figure 1 Flow chart of patient selection criteria. |
After PSM, a total of 86 patients were matched, including 43 patients in the TACE-MWA group and 43 patients in the liver resection group, respectively. The differences in the baseline characteristics between the two groups were balanced after PSM. The detailed characteristics of the patients before and after PSM are summarized in Table 1.
 |
Table 1 The Detailed Characteristics of the Patients Before and After PSM |
Overall Survival
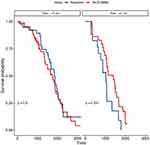
The median follow-up period was 80.7 months (95% CI, 69.7–104.6 months) in all patients. During the follow-up period, 76 patients (80.8%) in the TACE-MWA group and 42 patients (87.5%) in the liver resection group died. The median OS was 50.2 months in the TACE-MWA group and 54.1 months in the liver resection group. The cumulative survival rates at 1, 3, and 5 years were 92.5%, 69.1%, and 37.5% in the TACE-MWA group and 90.7%, 71.4%, and 40.5% in the liver resection group, respectively. The survival benefits were comparable between the two groups (P = 0.93, Figure 2A).
After employing PSM, the median OS was 61.2 months in the TACE-MWA group and 54.3 months in the liver resection group. The cumulative survival rates at 1, 3, and 5 years were 100%, 80.3%, and 51.0% in the TACE-MWA group and 88.3%, 66.7%, and 39.4% in the liver resection group, respectively. The TACE-MWA group still showed comparable OS to the resection group even after PSM (P = 0.3, Figure 2B). Subgroup analyses were then conducted according to potentially important factors, including age, gender, etiology, tumor size (<7cm vs ≥7cm), AFP (AFP <400ng/mL vs AFP ≥400ng/mL), and ALBI grade. No significant differences were observed in most of the subgroups apart from the patients with tumor size ≥7cm. Patients with tumor size ≥7cm in the TACE-MWA group had significantly prolonged OS compared to patients in the liver resection group (P < 0.001) (Figure 3).
Univariate and multivariate regression results are shown in Table 2. In the univariate analysis, the significant prognostic factors were antiviral treatment (HR = 0.25; 95% CI: 0.13–0.52; P = 0.002), tumor size ≥7cm (HR = 2.27; 95% CI: 1.30–3.95; P = 0.004) and NLR ≥2.81 (HR = 3.34; 95% CI: 1.97–5.68; P < 0.001). Similarly, antiviral treatment (HR = 0.57; 95% CI: 0.34–0.97; P = 0.037), tumor size ≥7cm (HR = 1.88; 95% CI: 1.07–3.31; P = 0.029) and NLR ≥2.81 (HR = 3.49; 95% CI: 1.79–6.83; P < 0.001) remained significantly associated with OS in the multivariate analysis.
 |
Table 2 Univariate and Multivariate Analyses of Prognostic Factors for Overall Survival in Patients with Solitary Large HCC and in the Propensity Score-Matched Cohort |
Progression Survival
During the follow-up period, 84 (89.3%) patients in the TACE-MWA group and 42 (77.7%) patients in the liver resection group had tumor progression. The median PFS, 1-, 3-, and 5-year PFS rates were 24.4 months, 74.2%, 37.5%, and 15.2% in the TACE-MWA group and 32.5 months, 75.9%, 45.1%, and 28.2% in the liver resection group, respectively. PFS did not significantly differ between the two groups (P = 0.12, Figure 4A).
In the PSM adjusted population, the median PFS was 35.3 months in the TACE-MWA group and 31.3 months in the liver resection group. The 1-, 3-, and 5-year PFS rates were 76.7%, 48.8%, and 19.6% in the TACE plus MWA group and 72%, 40.2%, and 22.6% in the liver resection group, respectively. Similarly, there was still no significant difference in PFS between the two groups after PSM (P=0.66; Figure 4B). Subgroup analyses showed that no significant difference was obtained.
Univariate and multivariate analyses are shown in Table 3. In the univariate analysis, the significant prognostic factors were antiviral treatment (HR = 0.55; 95% CI: 0.43–0.71; P = 0.001), tumor size ≥7cm (HR = 2.15; 95% CI: 1.31–3.54; P = 0.003) and NLR ≥2.81 (HR = 2.07; 95% CI: 1.28–3.35; P = 0.003). Similarly, antiviral treatment (HR = 0.47; 95% CI: 0.34–0.65; P = 0.002), tumor size ≥7cm (HR = 2.04; 95% CI: 1.24–3.37; P = 0.005) and NLR ≥2.81 (HR = 1.97; 95% CI: 1.22–3.20; P = 0.006) remained significantly associated with PFS in the multivariate analysis.
 |
Table 3 Univariate and Multivariate Analyses of Prognostic Factors for Progression Free Survival in Patients with Solitary Large HCC and in the Propensity Score-Matched Cohort |
Complications and Length of Hospital Stay
No treatment-related deaths were observed in the TACE-MWA group and the liver resection group. Minor complications in both groups included fever, nausea, vomiting, abdominal pain, transient abnormal liver function, and pleural effusion, which could be relieved by symptomatic treatments. Major complications in the TACE-MWA group included liver abscess, bile leakage, and bleeding, while these in the liver resection group were liver failure, biliary leakage, ascites, liver abscess, hemorrhage, pulmonary infection, and abdominal infection. Major complications were reported more frequently in the resection group than in the TACE-MWA group either before or after PSM (before: P = 0.001; after: P = 0.029) (Table 4). Also, the length of hospital stay was significantly shorter in the TACE-MWA group (before: 14.4 ± 7.62; after: 13.2 ± 6.78 days) than in the resection group (before: 26.2 ± 14.0; after: 23.1 ± 12.2 days) either before or after PSM (before: P < 0.001; after: P < 0.01).
 |
Table 4 Safety in Patients with Solitary Large HCC Before and After PSM |
Discussion
In our study, TACE-MWA showed comparable efficacy in terms of OS and PFS to liver resection in patients with SLHCC. Of note, TACE plus MWA showed longer OS than liver resection for HCC patients with tumor size ≥7cm. Moreover, the TACE-MWA group had a lower rate of major complications and shorter length of hospital stay. To our knowledge, this is the first study to compare TACE plus MWA with surgical resection in patients with SLHCC.
SLHCC is a special subgroup of HCC, for which the best treatment option remains to be addressed. According to the BCLC staging system, solitary tumor irrespective of their size, along with good clinical conditions and preserved liver function without macrovascular invasion and extrahepatic spread, is defined as early stage. Liver resection is the first-line option for patients at the early stage.4,5 Nevertheless, some authors considered that SLHCC should be classified as BCLC B stage or BCLC AB stage, due primarily to its significantly worse prognosis when resected as compared to a small tumor, creating an urgent need to optimize treatments for these patients.3,23,24 Ablation therapies are considered comparable to resection in patients with HCC ≤ 3 cm, but their efficacy decreases with the tumor burden increasing. Livraghi et al reported that the complete ablation rate was 75% after RFA in patients with a medium tumor (3–5 cm), while the rate was only 23–25% in patients with a large tumor (≥5 cm).11 Although MWA achieves more tumor necrosis rate than RFA, its survival benefits remain limited in large tumor.19 TACE has been regarded as the first-line treatment for unresectable HCC, which is difficult to achieve complete necrosis in one session, especially in large HCC. TACE is usually used repeatedly. The repeated TACE not only increases the cumulative dose of chemotherapeutic drugs, thereby worsening liver function, but also may result in “TACE refractory” and reduce the efficacy.25 Several studies have shown that TACE alone in the treatment of SLHCC is inferior to surgical resection. Jin et al reported the 1-, 3-, and 5-year survival rates of SLHCC were 83.2%, 75.7%, and 65.0% in the resection group, and 68.5%, 45.0%, and 17.5% in the TACE group (P < 0.01).26 Liu et al also reported that 1-, 3- and 5-year survival rates of SLHCC were 87%, 76%, and 61% in the resection group, and 79%, 46%, and 36% in TACE alone group, respectively (p < 0.001). These results showed that ablation or TACE was insufficient to improve the prognosis of SLHCC.
TACE plus ablation is a promising therapy for large HCC in clinical scenario.27,28 The rationale of the combination includes (1) a large tumor has richer blood supply than a small one. The thermal energy generated by the ablation is more easily carried away by the blood flow (heat-sink effect), which reduces the efficacy of ablation. This phenomenon can be improved by TACE via a reduction in blood supply. (2) Post-TACE lipiodol deposition provides help for tumor localization and guidance for subsequent ablation and the achievement of precise ablation. (3) For large tumor burden, the tumor volume can be significantly reduced by TACE, thereby decreasing the ablation zone and time. (4) The chemotherapy drugs used in TACE have immunosuppressive side effects, while some studies have demonstrated that ablation can enhance immune response.29,30
Previous studies compared TACE combined with RFA versus surgical resection in HCC. Kagawa et al31 in 2010 reported that the 1-, 3-, and 5-year OS in the TACE+RFA group were 100%, 94.8%, and 64.6%, while those in the surgical resection group were 92.5%, 82.7%, and 76.9% within the Milan Criteria, respectively (P > 0.05). Kim et al32 published a study in 2013 comparing TACE plus RFA versus surgical resection for single 2–5 cm HCC. The 1-, 2-, 3-, and 4-year OS in the TACE+RFA group were 97.3%, 86.5%, 78.4% and 78.4%, and 95.7%, 89.4%, 84.3% and 80.3% in the surgical resection group (P = 0.6321). Since the patients included in our study had larger tumor size compared with the above studies, the OS and PFS were lower. Pan et al33 compared TACE-RFA and liver resection in patients with HCC who met the up-to-seven criteria (the sum of the size of the largest tumor (cm) and the number of tumors equals seven). After PSM, the median OS was 56.0 months and 58.0 months in the TACE plus RFA group and surgical resection, respectively. The 1-, 3-, and 5-year survival rates were 96.1%, 76.7%, and 41.3% and 96.1%, 86.4% and 46.2%, respectively. No significant difference was obtained in the two groups (P = 0. 261). Tumor size >5 cm was not an independent prognostic factor (P=0.0163). This conclusion was consistent with our study. Subsequently, Yuan et al34 published a study in 2018 comparing the efficacy of TACE plus RFA and liver resection in patients with liver cancer beyond Milan criteria. The 1-, 2-, 3-, and 5-year OS rates and median survival time in the TACE combined with the RFA group were 98.5%, 83.1%, 66.2%, and 37.1% and 46 months, and 89.6%, 69.4%, 53.7%, 30.3%, and 38 months in the surgical resection group, respectively (P = 0.017). The better OS in our study may be due to the larger tumor diameter, and 100 patients (37.1%) were multiple tumors in Yuan et al’s study.
In our study, tumor diameter ≥7 cm was an independent risk factor for OS and PFS. The larger the liver tissue ablated or resected, the worse liver function compromised. Besides, the invasiveness of the tumor enhances with the tumor size increasing.35 A great number of studies suggested that tumor diameter was associated with microvascular invasion in HCC, which significantly affected postoperative recurrence and survival.36 The study by Zhuang et al37 showed that tumor diameter >7.1 cm was an independent risk factor for surgical resection of large solitary HCC (HR: 2.21, 95% CI: 1.3–3.75, P = 0.003). Yuan et al’s study comparing surgical resection and TACE combined with RFA in patients beyond Milan criteria also showed that tumor diameter >7 cm was an independent risk factor for OS and PFS.34
In addition, this study found that higher NLR was an independent risk factor for OS and PFS. In HCC patients, previous studies demonstrated the prognostic value of NLR in multiple treatment modalities, including TACE, ablation, targeted, and immunotherapy.38,39 Numerous studies have shown that systemic inflammatory response plays a crucial role in the development and progression in various cancers. Neutrophils promote cancer progression by suppressing the cytolytic activity of immune cells and the secretion of various inflammatory cytokines and therefore probably lead to a stimulating tumor microenvironment.40,41 Moreover, lymphocytes have long been considered one of the primary effector cells in anti-tumor response, and previous researches showed that increasing infiltration of tumors with lymphocytes was associated with better response to cytotoxic treatment and prognosis in cancer patients.42,43
Antiviral treatment plays a critical role in the management of HCC. The predominant etiology of HCC in China is HBV, which is higher than other etiology.44 HBV reactivation may be influenced by operations such as resection or TACE, which activates HBV-DNA replication, thereby influencing prognosis.45,46
This study has several limitations. First, the main concern of our study is its retrospective nature, which makes selection and confounding biases inevitable, thus limiting the power of conclusions. Although PSM and multivariate regression may adjust for some of the imbalanced covariates, unknown confounders that cannot be adjusted for may be exist. Second, this study is a single-center study, and the results of this study may be affected by the experience of doctors and the patients who come to our hospital. Third, the sample size is small especially after PSM, with only 43 patients in each group. Fourth, most patients in this study were viral hepatitis, especially hepatitis B. Therefore, the results need to be further verified in large-scale cohorts or randomized clinical trials.
Conclusions
In conclusion, TACE plus MWA provides comparable efficacy, better safety, and shorter hospital stay. For HCC patients with tumor diameters greater than 7 cm, TACE plus MWA may be superior to surgical resection. Large-scale randomized clinical trials are warranted to validate these results in the future.
Ethics Approval and Informed Consent
This study was conducted in line with the Declaration of Helsinki, and written informed consent was obtained from all the eligible patients before treatment. Clinical research protocol and clinical data were approved by the Ethics Committee of Beijing Ditan Hospital (KY2020-030).
Acknowledgment
This work was supported by the Capital’s Funds for Health Improvement and Research [grant number 2020-2475 2175], Beijing Talents Project, and Beijing Municipal Science & Technology [Commission No. Z221100007422026].
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no known competing interests or personal relationships that could have appeared to influence the work reported in this paper.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249.
2. Park JW, Chen M, Colombo M, et al. Global patterns of hepatocellular carcinoma management from diagnosis to death: the BRIDGE Study. Liver Int. 2015;35(9):2155–2166.
3. Liu PH, Su CW, Hsu CY, et al. Solitary large hepatocellular carcinoma: staging and treatment strategy. PLoS One. 2016;11(5):e0155588.
4. Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67(1):358–380.
5. European Association for the Study of the Liver. Electronic address eee, European Association for the Study of the L. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69(1):182–236.
6. Kim J, Kim JY, Lee JH, et al. Long-term outcomes of transarterial radioembolization for large single hepatocellular carcinoma: a comparison to resection. J Nucl Med. 2021;63:1215.
7. Ding X, Sun W, Chen J, et al. Percutaneous radiofrequency ablation combined with transarterial chemoembolization plus sorafenib for large hepatocellular carcinoma invading the portal venous system: a prospective randomized study. Front Oncol. 2020;10:578633.
8. Yang LY, Fang F, Ou DP, Wu W, Zeng ZJ, Wu F. Solitary large hepatocellular carcinoma: a specific subtype of hepatocellular carcinoma with good outcome after hepatic resection. Ann Surg. 2009;249(1):118–123.
9. Zhao HC, Wu RL, Liu FB, et al. A retrospective analysis of long term outcomes in patients undergoing hepatic resection for large (>5 cm) hepatocellular carcinoma. HPB. 2016;18(11):943–949.
10. Mazzaferro V, Sposito C, Zhou J, et al. Metroticket 2.0 model for analysis of competing risks of death after liver transplantation for hepatocellular carcinoma. Gastroenterology. 2018;154(1):128–139.
11. Livraghi T, Goldberg SN, Lazzaroni S, et al. Hepatocellular carcinoma: radio-frequency ablation of medium and large lesions. Radiology. 2000;214(3):761–768.
12. Abdelaziz AO, Nabeel MM, Elbaz TM, et al. Microwave ablation versus transarterial chemoembolization in large hepatocellular carcinoma: prospective analysis. Scand J Gastroenterol. 2015;50(4):479–484.
13. Xue T, Le F, Chen R, et al. Transarterial chemoembolization for huge hepatocellular carcinoma with diameter over ten centimeters: a large cohort study. Med Oncol. 2015;32(3):64.
14. Yang Y, Yu H, Qi L, et al. Combined radiofrequency ablation or microwave ablation with transarterial chemoembolization can increase efficiency in intermediate-stage hepatocellular carcinoma without more complication: a systematic review and meta-analysis. Int J Hyperthermia. 2022;39(1):455–465.
15. Chen QW, Ying HF, Gao S, et al. Radiofrequency ablation plus chemoembolization versus radiofrequency ablation alone for hepatocellular carcinoma: a systematic review and meta-analysis. Clin Res Hepatol Gastroenterol. 2016;40(3):309–314.
16. Wang Y, Ma L, Yuan Z, Zheng J, Li W. Percutaneous thermal ablation combined with TACE versus TACE monotherapy in the treatment for liver cancer with hepatic vein tumor thrombus: a retrospective study. PLoS One. 2018;13(7):e0201525.
17. Makary MS, Khandpur U, Cloyd JM, Mumtaz K, Dowell JD. Locoregional therapy approaches for hepatocellular carcinoma: recent advances and management strategies. Cancers. 2020;12:7.
18. Gui CH, Baey S. Trans-arterial chemoembolization + radiofrequency ablation versus surgical resection in hepatocellular carcinoma – a meta-analysis. Euro J Surg Oncol. 2020;46(5):763–771.
19. Nault JC, Sutter O, Nahon P, Ganne-Carrie N, Seror O. Percutaneous treatment of hepatocellular carcinoma: state of the art and innovations. J Hepatol. 2018;68(4):783–797.
20. Zhao J, Wu J, He M, et al. Comparison of transcatheter arterial chemoembolization combined with radiofrequency ablation or microwave ablation for the treatment of unresectable hepatocellular carcinoma: a systemic review and meta-analysis. Int J Hyperthermia. 2020;37(1):624–633.
21. Laska E, Meisner M, Wanderling J. A maximally selected test of symmetry about zero. Stat Med. 2012;31(26):3178–3191.
22. Deng M, Ng SWY, Cheung ST, Chong CCN. Clinical application of Albumin-Bilirubin (ALBI) score: the current status. Surgeon. 2020;18(3):178–186.
23. Jung YK, Jung CH, Seo YS, et al. BCLC stage B is a better designation for single large hepatocellular carcinoma than BCLC stage A. J Gastroenterol Hepatol. 2016;31(2):467–474.
24. Zhong JH, Pan LH, Wang YY, et al. Optimizing stage of single large hepatocellular carcinoma: a study with subgroup analysis by tumor diameter. Medicine. 2017;96(15):e6608.
25. Raoul JL, Forner A, Bolondi L, Cheung TT, Kloeckner R, de Baere T. Updated use of TACE for hepatocellular carcinoma treatment: how and when to use it based on clinical evidence. Cancer Treat Rev. 2019;72:28–36.
26. Jin YJ, Lee JW, Choi YJ, et al. Surgery versus transarterial chemoembolization for solitary large hepatocellular carcinoma of BCLC stage A. J Gastrointest Surg. 2014;18(3):555–561.
27. Wang Y, Ma L, Sheng S, Yuan Z, Zheng J, Li W. Combination therapy of TACE and CT-guided partial hepatic segment ablation for liver cancer. Minim Invasive Ther Allied Technol. 2018;27(6):355–364.
28. Liu B, Li W, Zheng J. Safety and efficacy of the combination therapy of transcatheter arterial chemoembolization and ablation for hepatocellular carcinoma with inferior vena cava tumor thrombus: a consecutive case series. J Cancer Res Ther. 2020;16(5):1186–1190.
29. Liu B, Zhang Y, Chen H, Li W, Tsochatzis E. The combination of transcatheter arterial chemoembolisation (TACE) and thermal ablation versus TACE alone for hepatocellular carcinoma. Cochrane Database Syst Rev. 2022;1:CD013345.
30. Zuo TY, Liu FY, Wang MQ, Chen XX. Transcatheter arterial chemoembolization combined with simultaneous computed tomography-guided radiofrequency ablation for large hepatocellular carcinomas. Chin Med J. 2017;130(22):2666–2673.
31. Kagawa T, Koizumi J, Kojima S-I, et al. Transcatheter arterial chemoembolization plus radiofrequency ablation therapy for early stage hepatocellular carcinoma: comparison with surgical resection. Cancer. 2010;116(15):3638–3644.
32. Kim JW, Shin SS, Kim JK, et al. Radiofrequency ablation combined with transcatheter arterial chemoembolization for the treatment of single hepatocellular carcinoma of 2 to 5 cm in diameter: comparison with surgical resection. Korean J Radiol. 2013;14(4):626–635.
33. Pan T, Mu L-W, Wu C, et al. Comparison of combined transcatheter arterial chemoembolization and CT-guided radiofrequency ablation with surgical resection in patients with hepatocellular carcinoma within the up-to-seven criteria: a multicenter case-matched study. J Cancer. 2017;8(17):3506–3513.
34. Yuan H, Cao P, Li H-L, et al. Transarterial chemoembolization with radiofrequency ablation versus hepatectomy in hepatocellular carcinoma beyond the Milan criteria: a retrospective study. Cancer Manag Res. 2018;10:5545–5552.
35. Pawlik TM, Delman KA, Vauthey JN, et al. Tumor size predicts vascular invasion and histologic grade: implications for selection of surgical treatment for hepatocellular carcinoma. Liver Transpl. 2005;11(9):1086–1092.
36. Hu H, Qi S, Zeng S, et al. Importance of microvascular invasion risk and tumor size on recurrence and survival of hepatocellular carcinoma after anatomical resection and non-anatomical resection. Front Oncol. 2021;11:621622.
37. Zhuang H, Zhou Z, Ma Z, et al. Prognostic stratification based on a novel nomogram for solitary large hepatocellular carcinoma after curative resection. Front Oncol. 2020;10:556489.
38. Mouchli M, Reddy S, Gerrard M, Boardman L, Rubio M. Usefulness of neutrophil-to-lymphocyte ratio (NLR) as a prognostic predictor after treatment of hepatocellular carcinoma”. Review article. Ann Hepatol. 2021;22:100249.
39. Lin S, Hu S, Ran Y, Wu F. Neutrophil-to-lymphocyte ratio predicts prognosis of patients with hepatocellular carcinoma: a systematic review and meta-analysis. Transl Cancer Res. 2021;10(4):1667–1678.
40. Giese MA, Hind LE, Huttenlocher A. Neutrophil plasticity in the tumor microenvironment. Blood. 2019;133(20):2159–2167.
41. Mollinedo F. Neutrophil degranulation, plasticity, and cancer metastasis. Trends Immunol. 2019;40(3):228–242.
42. Farhood B, Najafi M, Mortezaee K. CD8(+) cytotoxic T lymphocytes in cancer immunotherapy: a review. J Cell Physiol. 2019;234(6):8509–8521.
43. Bian J, Lin J, Long J, et al. T lymphocytes in hepatocellular carcinoma immune microenvironment: insights into human immunology and immunotherapy. Am J Cancer Res. 2020;10(12):4585–4606.
44. Stella L, Santopaolo F, Gasbarrini A, Pompili M, Ponziani FR. Viral hepatitis and hepatocellular carcinoma: from molecular pathways to the role of clinical surveillance and antiviral treatment. World J Gastroenterol. 2022;28(21):2251–2281.
45. Lin XJ, Lao XM, Shi M, Li SP. Changes of HBV DNA after chemoembolization for hepatocellular carcinoma and the efficacy of antiviral treatment. Dig Dis Sci. 2016;61(9):2465–2476.
46. Yu LH, Li N, Shi J, Guo WX, Wu MC, Cheng SQ. Does anti-HBV therapy benefit the prognosis of HBV-related hepatocellular carcinoma following hepatectomy? Ann Surg Oncol. 2014;21(3):1010–1015.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.