Back to Journals » OncoTargets and Therapy » Volume 9
Comparison of single agent versus combined chemotherapy in previously treated patients with advanced urothelial carcinoma: a meta-analysis
Authors Wu X, Zhi Y, He P, Zhou X, Zheng J, Chen Z, Zhou Z
Received 24 September 2015
Accepted for publication 6 November 2015
Published 15 March 2016 Volume 2016:9 Pages 1535—1543
DOI https://doi.org/10.2147/OTT.S97062
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Daniele Santini
Xiao-Jun Wu, Yi Zhi, Peng He, Xiao-Zhou Zhou, Ji Zheng, Zhi-Wen Chen, Zhan-Song Zhou
Institute of Urinary Surgery, Southwest Hospital, Third Military Medical University, Chongqing, People’s Republic of China
Background: Platinum-based chemotherapy is the standard treatment for advanced urothelial cancer (UC) and is generally used in the first-line setting. However, the optimal salvage treatment for previously treated UC patients is unclear. We conducted a systematic review of published clinical trials of single agent versus combined chemotherapy as salvage treatment in previously treated UC patients.
Methods: Trials published between 1994 and 2015 were identified by an electronic search of public databases (MEDLINE, EMBASE, Cochrane library). All relevant studies were independently identified by two authors for inclusion. Demographic data, treatment regimens, objective response rate (ORR), disease control rate (DCR), median progression-free and overall survival (PFS, OS), and grade 3/4 toxicities were extracted and analyzed using Comprehensive Meta Analysis software (Version 2.0).
Results: Fifty cohorts with 1,685 patients were included for analysis: 814 patients were treated with single agent chemotherapy and 871 with combined chemotherapy. Pooled OS was significantly higher at 1 year for combined chemotherapy than for single agent (relative risk [RR] 1.52; 95% CI: 1.01–2.37; P=0.03) but not for 2-year OS (RR 1.31; 95% CI: 0.92–1.85; P=0.064). Additionally, combined chemotherapy significantly improved ORR (RR 2.25; 95% CI: 1.60–3.18; P<0.001) and DCR (RR 1.12; 95% CI: 1.01–1.25, P=0.033) compared to single agent for advanced UC patients. As for grade 3 and 4 toxicities, more frequencies of leukopenia and thrombocytopenia were observed in the combined chemotherapy than in single agent group, while equivalent frequencies of anemia, nausea, vomiting, and diarrhea were found between the two groups.
Conclusion: In comparison with single agent alone, combined chemotherapy as salvage treatment for advanced UC patients significantly improved ORR, DCR, and 1-year OS, but not 2-year OS. Our findings support the need to compare combined chemotherapy with single agent alone in the salvage setting in large prospective trials due to its potential survival benefit in advanced UC patients.
Keywords: advanced urothelial cancer, salvage chemotherapy, cytotoxic agents, meta-analysis, efficacy
Introduction
Urothelial cancer (UC), also called transitional cell carcinoma, accounts for more than 90% of bladder cancers, with more than 350,000 newly diagnosed cases, and causes approximately 150,000 deaths per year worldwide.1 Approximately 75%–80% of cases of urothelial tumors present with non-muscle invasive disease; however, the remaining cases of advanced (muscle invasive) disease can progress to metastatic disease, and the prognosis of these patients is very poor.2 Currently, platinum-based chemotherapy is the standard of care for advanced UC patients. These chemotherapy regimens include combinations such as cisplatin and gemcitabine and methotrexate, vinblastine, doxorubicin, and cisplatin.3 However, platinum resistance occurs rapidly and nearly 80% of cases relapse. For these patients, there remains no consensus regarding optimal treatment. In the first and largest randomized Phase-III trial conducted by Bellmunt et al in 2009,4 vinflunine chemotherapy demonstrated a 8.6% response rate with a 2.3-month survival benefit; this led to the approval of vinflunine as second-line therapy for UC by the European Medicines Agency (EMA) in 2009 but not in the USA. Recently, many cytotoxic agents,5–11 as single agent or in combination, have been extensively investigated as candidate second-line chemotherapies for advanced UC. However, to our best knowledge, there are no head-to-head comparison data available for single agent versus combined chemotherapy in the treatment of previously treated patients with UC. Therefore, we performed a systematic review and meta-analysis of published data to compare treatment outcomes with single agent versus combined chemotherapy for the management of previously treated patients with UC.
Methods
Study design
We developed a protocol that defined inclusion criteria, search strategy, outcomes of interest, and analysis plan. The reporting of this systematic review adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statements.12
Identification and selection of studies
To identify studies for inclusion in our systematic review and meta-analysis, we did a broad search of four databases, including EMBASE, MEDLINE, the Cochrane Central Register of Controlled Trials, and the Cochrane Database of Systematic Reviews, from the date of inception of every database to July 2015. The search included the following terms: “urothelial neoplasms”, “urothelial carcinoma”, “urothelial cancer”, “chemotherapy”, “previously treated”, “refractory”, “salvage therapy”, and “clinical trials”. Additional references were searched through manual searches of the reference lists and specialist journals. No language restrictions were applied.
Study populations (referred to hereafter as cohorts) with the following criteria were eligible for the study: 1) patients with UC who were refractory to previous chemotherapy; 2) patients who were under treatment with combined chemotherapy or single agent chemotherapy (patients who received molecular agent alone or chemotherapy plus molecular targeted agents were excluded for analysis in our study); 3) patients with reported outcomes of interest (ie, objective response rate [ORR], disease control rate [DCR], and 1- and 2-year overall survival [OS]; and 4) patients from an original study (ie, randomized controlled trial, non-randomized clinical trial, observational studies, or case series).
Data extraction
Two investigators screened the titles and abstracts of potentially relevant studies. We retrieved the full text of relevant studies for further review by the same two reviewers. A third senior investigator resolved any discrepancies between reviewers. If reviewers suspected an overlap of cohorts in a report, they contacted the corresponding author for clarification; we excluded studies with a clear overlap.
The same pair of reviewers extracted study details independently, using a standardized pilot-tested form. A third investigator reviewed all data entries. We extracted the following data: author, study design, study period, median age, interventions (chemotherapy regimens and dose), sample size, and outcomes of interest. We defined outcomes of interest as ORR, DCR, and 1- and 2-year OS. To assess quality, since we included non-comparative (uncontrolled) studies in our systematic review and meta-analysis, we used the Newcastle-Ottawa quality assessment scale.13 We selected items that focused on representativeness of study patients, demonstration that the outcome of interest was not present at the start of the study, adequate assessment of outcome, sufficient length of follow-up to allow outcomes to arise, and adequacy of follow-up.
Statistical analysis
We prespecified the analysis plan in the protocol. We analyzed all patients who started single agent or combined chemotherapy, regardless of their adherence to treatment. We calculated event rates of outcome (the proportion of patients who developed outcomes of interest) from the included cohorts for both single agent and combined chemotherapy. We pooled log-transformed event rates with DerSimonian and Laird random-effect models and assessed heterogeneity using chi-square-based Q statistic test.14 We used the test of interaction proposed by Altman and Bland15 to compare log-transformed rates of outcomes between single agent and combined chemotherapy. A statistical test with a P-value less than 0.05 was considered significant. To measure overall heterogeneity across the included cohorts, we calculated the I2 statistic, with I2 greater than 50% indicating high heterogeneity. We did all statistical analyses with comprehensive meta-analysis software version 2.0 (Biostat, Englewood, NJ, USA).
Results
Search results
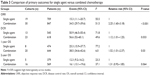
A total of 569 studies were identified from the database search, of which 70 reports were retrieved for full-text evaluation. Fifty cohorts from 49 trials met the inclusion criteria and were included in this systematic review4–11,16–56 (Figure 1). We did not find randomized controlled trials or controlled studies that compared single agent with combined chemotherapy in previously treated patients with UC directly. Table 1 shows the characteristics of the included studies. Overall, 1,685 patients previously treated with advanced UC were included, with a median age of 64 years for the single agent group and 65 years for the combined chemotherapy group. The median progression-free survival (PFS) and OS were higher in combined chemotherapy cohorts than single agent cohorts, while the median age did not significantly differ between groups (Table 2).
  | Figure 1 Selection process for clinical trials included in the meta-analysis. |
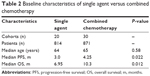  | Table 2 Baseline characteristics of single agent versus combined chemotherapy |
Methodological quality of the included studies was fair; most studies provided adequate outcome ascertainment, enrolled a representative sample of patients, and had an acceptable length of follow-up (Figure 2). However, comparative evidence was at high risk of bias because we compared data across studies not within them, and selection bias was likely to be present. Assessment of publication bias was not done because data would be unreliable in view of the few studies included for each treatment group and high heterogeneity (I2>50%) in most analyses.
  | Figure 2 Selected methodological quality indicator. |
Pooled incidence of primary outcomes
A total of 1,556 patients were included for ORR analysis. The pooled event rate of ORR for combination chemotherapy was higher than that of single agent alone (34.5% vs 15.3%, Table 3). A higher incidence of DCR and 1-year OS was observed in combination chemotherapy (56.6% and 38.5%, respectively), while comparable incidence of 2-year OS was found between combination chemotherapy and single agent alone (16.1% vs 12.3%, Table 3).
Efficacy comparison between combination chemotherapy and single agent
The pooled event rate of OS for combined chemotherapy was significantly higher than that for single agent chemotherapy at 1 year (relative risk [RR] 1.52; 95% confidence interval [CI]: 1.01–2.37; P=0.03) but not for 2-year OS (RR 1.31; 95% CI: 0.92–1.85; P=0.064, Table 3). Additionally, ORR and DCR were significantly different between combined chemotherapy and single agent (P<0.001 and P=0.033, respectively) (Table 3).
Toxicity
Table 4 shows the overall occurrence of high-grade (≥ grade 3) toxic effects with single agent versus combined chemotherapy. There were significantly more toxicities of leukopenia and thrombocytopenia in the combined chemotherapy than in single agent group (P<0.001 and P=0.024, respectively). While more incidence of fatigue was observed in single agent group when compared to combined chemotherapy (RR 0.17, 95% CI: 0.07–0.42, P<0.001). Additionally, equivalent frequencies of anemia, nausea, vomiting, and diarrhea were found between single agent and combined chemotherapy (Table 4).
  | Table 4 Comparison of higher than grade 3 toxic effect event rates for single agent versus combined chemotherapy |
Discussion
UC is the most common cancer of the urinary tract. Although platinum-based chemotherapy regimen is regarded as the gold standard for treating advanced UC patients,57 there is no established treatment for these patients with progressive disease other than the first-line platinum-based chemotherapy. Due to the aggressive and rapid fatal disease course of advanced UC, the development of systematic chemotherapy using combinations of agents is rational for the salvage treatment of this disease, especially in those patients with good performance status. However, to the best of our knowledge, there is lack of head-to-head comparison data available for combination chemotherapy versus single agent alone as salvage treatment for advanced UC patients. As a result, we conducted this systematic review and meta-analysis to evaluate the efficacy of combination chemotherapy versus single agent alone as salvage treatment for advanced UC patients.
A total of 1,685 advanced UC patients from 50 cohorts are included for analysis. Based on our pooled results, we found that combined chemotherapy resulted in a statistically increased ORR, DCR, and 1-year OS but not for 2-year OS. In addition, our study indicated that combination chemotherapy was associated with more frequencies of grade 3 and 4 myelosuppression toxicities, while equivalent frequencies of anemia, nausea, vomiting, and diarrhea were found between single agent and combined chemotherapy except for fatigue. However, clinicians should be cautious when interrupting these results due to the limitation of our studies, and more evidence is still required to identify patients who will most likely benefit by the appropriate combination chemotherapy.
After we completed our study, a similar analysis of taxanes-containing combination chemotherapy versus single agent taxane in previously treated UC patients was published.58 This latter study revealed that taxanes-containing chemotherapy significantly is associated with an improved OS (hazard ratio 0.60; 95% CI: 0.45–0.82; P<0.001) and PFS (hazard ratio 0.61; 95% CI: 0.49–0.77; P<0.001). Our study is different on several counts. First, our study included both taxanes and other chemotherapy drugs as salvage treatment for advanced UC patients, resulting in a larger sample size (1,685 versus 370 patients). Secondly, our study also assessed the ORR, DCR, and grade 3/4 toxicities with combination chemotherapy versus single agent. Importantly, despite literature review from two separate groups, using different methodology, and including some nonoverlapping trials, both studies demonstrated a significantly increased OS benefits, adding further validity to the findings.
Several limitations need to be mentioned in this analysis. First and most importantly, the application of formal meta-analytic methods to observational studies was controversial. One of the most important reasons for this is that the designs and populations of the studies were diverse and that these differences may influence the pooled estimates. However, as no head-to-head comparison data are available for combination chemotherapy versus single agent alone, a meta-analysis of observational studies is one of the few methods for assessing efficacy and toxicities.59 Moreover, it represents the uncertainty surrounding the pooled estimates and is a valuable method to decide on whether more evidence is needed, which was a timely discussion topic with regard to salvage chemotherapy for advanced UC patients. Second, the study was a pooled analysis of primarily single-arm prospective studies and retrospective series, with a small number of patients included that might have overreported the benefit of preoperative treatments. The inclusion criteria also likely favor young, fit, and responder patients and a highly selected group of subjects with good prognostic indicators; all of these might cause potential selection bias. Third, we included UC patients treated with different combination or single agent chemotherapy for analysis, which would increase the clinical heterogeneity among included trials, which also made the interpretation of a meta-analysis more problematic. Additionally, we could not answer that which combination regimens would be the best choice. Finally, this meta-analysis only considered published literature, and lack of individual patient data restricted us from adjusting the treatment effect according to previous treatment and patient variables.
Conclusion
Currently available clinical evidence for advanced UC patients indicates that combined chemotherapy may be a more efficient regimen for previously treated UC patients, but with more frequencies of grade 3 and 4 myelosuppression toxicities compared with single agent. However, since the overall quantity and quality of data regarding salvage chemotherapy is poor, there might be risk of bias in comparisons between observation studies. No definite conclusions were attained from the results. As a result, prospective randomized studies, definitively comparing the survival and treatment toxicity between combined chemotherapy and single agent, are strongly recommended to clearly determine the role of combined chemotherapy as salvage treatment for previously treated UC patients.
Acknowledgments
The authors are indebted to the authors of the primary studies, for without their contributions, this work would have been impossible. The study was supported by a grant from Natural Science Foundation of China (No 81270692).
Disclosure
The authors report no conflicts of interest in this work.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. | ||
Narayanan S, Harshman LC, Srinivas S. Second-line therapies in metastatic urothelial carcinoma. Hematol Oncol Clin North Am. 2015;29(2):341–359. | ||
Bellmunt J, von der Maase H, Mead GM, et al. Randomized phase III study comparing paclitaxel/cisplatin/gemcitabine and gemcitabine/cisplatin in patients with locally advanced or metastatic urothelial cancer without prior systemic therapy: EORTC Intergroup Study 30987. J Clin Oncol. 2012;30(10):1107–1113. | ||
Bellmunt J, Theodore C, Demkov T, et al. Phase III trial of vinflunine plus best supportive care compared with best supportive care alone after a platinum-containing regimen in patients with advanced transitional cell carcinoma of the urothelial tract. J Clin Oncol. 2009;27(27):4454–4461. | ||
Albers P, Siener R, Hartlein M, et al. Gemcitabine monotherapy as second-line treatment in cisplatin-refractory transitional cell carcinoma – prognostic factors for response and improvement of quality of life. Onkologie. 2002;25(1):47–52. | ||
Krege S, Rembrink V, Borgermann C, Otto T, Rubben H. Docetaxel and ifosfamide as second line treatment for patients with advanced or metastatic urothelial cancer after failure of platinum chemotherapy: a phase 2 study. J Urol. 2001;165(1):67–71. | ||
Lorusso V, Pollera CF, Antimi M, et al. A phase II study of gemcitabine in patients with transitional cell carcinoma of the urinary tract previously treated with platinum. Italian Co-operative Group on Bladder Cancer. Eur J Cancer. 1998;34(8):1208–1212. | ||
Papamichael D, Gallagher CJ, Oliver RT, Johnson PW, Waxman J. Phase II study of paclitaxel in pretreated patients with locally advanced/metastatic cancer of the bladder and ureter. Br J Cancer. 1997;75(4):606–607. | ||
Sweeney CJ, Roth BJ, Kabbinavar FF, et al. Phase II study of pemetrexed for second-line treatment of transitional cell cancer of the urothelium. J Clin Oncol. 2006;24(21):3451–3457. | ||
Winquist E, Vokes E, Moore MJ, Schumm LP, Hoving K, Stadler WM. A phase II study of oxaliplatin in urothelial cancer. Urol Oncol. 2005;23(3):150–154. | ||
McCaffrey JA, Hilton S, Mazumdar M, et al. Phase II trial of docetaxel in patients with advanced or metastatic transitional-cell carcinoma. J Clin Oncol. 1997;15(5):1853–1857. | ||
Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. | ||
Wells GA SB, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in metaanalyses; 2014. Available from: http://www.ohrica/programs/clinical_epidemiology/oxfordasp. Accessed August 22, 2014. | ||
Zintzaras E, Ioannidis JP. Heterogeneity testing in meta-analysis of genome searches. Genet Epidemiol. 2005;28(2):123–137. | ||
Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ. 2003;326(7382):219. | ||
Matsumoto K, Mochizuki K, Hirayama T, et al. Gemcitabine plus nedaplatin as salvage therapy is a favorable option for patients with progressive metastatic urothelial carcinoma after two lines of chemotherapy. Asian Pac J Cancer Prev. 2015;16(6):2483–2487. | ||
Maolake A, Izumi K, Takahashi R, et al. Efficacy of tegafur-uracil in advanced urothelial cancer patients after the treatment failure of platinum-based chemotherapy. Anticancer Res. 2015;35(3):1603–1606. | ||
Naiki T, Kawai N, Hashimoto Y, et al. Gemcitabine and docetaxel, an effective second-line chemotherapy for lung metastasis of urothelial carcinoma. Int J Clin Oncol. 2014;19(3):516–522. | ||
Morales-Barrera R, Suarez C, Valverde C, et al. Do patients with metastatic urothelial carcinoma benefit from docetaxel as second-line chemotherapy? Clin Transl Oncol. 2014;16(1):102–106. | ||
Lee JH, Kang SG, Kim ST, et al. Modified MVAC as a second-line treatment for patients with metastatic urothelial carcinoma after failure of gemcitabine and cisplatin treatment. Cancer Res Treat. 2014;46(2):172–177. | ||
Rozzi A, Santini D, Salerno M, et al. Pegylated liposomal doxorubicin as third-line chemotherapy in patients with metastatic transitional cell carcinoma of urothelial tract: results of a phase II study. Med Oncol. 2013;30(1):407. | ||
Ko YJ, Canil CM, Mukherjee SD, et al. Nanoparticle albumin-bound paclitaxel for second-line treatment of metastatic urothelial carcinoma: a single group, multicentre, phase 2 study. Lancet Oncol. 2013;14(8):769–776. | ||
Halim A, Abotouk N. Methotrexate-paclitaxel-epirubicin-carboplatin as second-line chemotherapy in patients with metastatic transitional cell carcinoma of the bladder pretreated with cisplatin-gemcitabine: a phase II study. Asia Pac J Clin Oncol. 2013;9(1):60–65. | ||
Bhattacharyya M, Powles T, Mutsvangwa K, Wilson P, Oliver T, Shamash J. A phase II study of mitomycin, fluorouracil, folinic acid, and irinotecan (MFI) for the treatment of transitional cell carcinoma of the bladder. Urol Oncol. 2013;31(6):878–882. | ||
Tsuruta H, Inoue T, Narita S, et al. Combination therapy consisting of gemcitabine, carboplatin, and docetaxel as an active treatment for advanced urothelial carcinoma. Int J Clin Oncol. 2011;16(5):533–538. | ||
Rozzi A, Salerno M, Bordin F, De Marco F, Di Nicola S, Lanzetta G. Weekly regimen of epirubicin and paclitaxel as second-line chemotherapy in patients with metastatic transitional cell carcinoma of urothelial tract: results of a phase II study. Med Oncol. 2011;28(Suppl 1):S426–S432. | ||
Kitamura H, Taguchi K, Kunishima Y, et al. Paclitaxel, ifosfamide, and nedaplatin as second-line treatment for patients with metastatic urothelial carcinoma: a phase II study of the SUOC group. Cancer Sci. 2011;102(6):1171–1175. | ||
Joung JY, Kwon WA, Cho IC, et al. Paclitaxel and cisplatin chemotherapy for metastatic urothelial carcinoma after failure of two courses of platinum-based regimens. Int J Urol. 2011;18(5):350–357. | ||
Ikeda M, Matsumoto K, Tabata K, et al. Combination of gemcitabine and paclitaxel is a favorable option for patients with advanced or metastatic urothelial carcinoma previously treated with cisplatin-based chemotherapy. Jpn J Clin Oncol. 2011;41(10):1214–1220. | ||
Albers P, Park SI, Niegisch G, et al. Randomized phase III trial of 2nd line gemcitabine and paclitaxel chemotherapy in patients with advanced bladder cancer: short-term versus prolonged treatment [German Association of Urological Oncology (AUO) trial AB 20/99]. Ann Oncol. 2011;22(2):288–294. | ||
Tanji N, Ozawa A, Miura N, et al. Long-term results of combined chemotherapy with gemcitabine and cisplatin for metastatic urothelial carcinomas. Int J Clin Oncol. 2010;15(4):369–375. | ||
Suyama T, Ueda T, Fukasawa S, et al. Combination of gemcitabine and paclitaxel as second-line chemotherapy for advanced urothelial carcinoma. Jpn J Clin Oncol. 2009;39(4):244–250. | ||
Srinivas S, Harshman LC. A phase II study of docetaxel and oxaliplatin for second-line treatment of urothelial carcinoma. Chemotherapy. 2009;55(5):321–326. | ||
Joly F, Houede N, Noal S, et al. Do patients with advanced urothelial carcinoma benefit from weekly paclitaxel chemotherapy? A GETUG phase II study. Clin Genitourin Cancer. 2009;7(2):E28–E33. | ||
Dumez H, Gallardo E, Culine S, et al. Phase II study of biweekly plitidepsin as second-line therapy for advanced or metastatic transitional cell carcinoma of the urothelium. Mar Drugs. 2009;7(3):451–463. | ||
Lassiter LK, Tummala MK, Hussain MH, Stadler WM, Petrylak DP, Carducci MA. Phase II open-label study of oral piritrexim in patients with advanced carcinoma of the urothelium who have experienced failure with standard chemotherapy. Clin Genitourin Cancer. 2008;6(1):31–35. | ||
Kanai K, Kikuchi E, Ohigashi T, et al. Gemcitabine and paclitaxel chemotherapy for advanced urothelial carcinoma in patients who have received prior cisplatin-based chemotherapy. Int J Clin Oncol. 2008;13(6):510–514. | ||
Han KS, Joung JY, Kim TS, et al. Methotrexate, vinblastine, doxorubicin and cisplatin combination regimen as salvage chemotherapy for patients with advanced or metastatic transitional cell carcinoma after failure of gemcitabine and cisplatin chemotherapy. Br J Cancer. 2008;98(1):86–90. | ||
Uhm JE, Lim HY, Kim WS, et al. Paclitaxel with cisplatin as salvage treatment for patients with previously treated advanced transitional cell carcinoma of the urothelial tract. Neoplasia. 2007;9(1):18–22. | ||
Matsumoto K, Irie A, Satoh T, Okazaki M, Iwamura M, Baba S. Gemcitabine and paclitaxel chemotherapy as a second-line treatment for advanced or metastatic urothelial carcinoma. Int J Urol. 2007;14(11):1000–1004; discussion 1004. | ||
Lin CC, Hsu CH, Huang CY, et al. Gemcitabine and ifosfamide as a second-line treatment for cisplatin-refractory metastatic urothelial carcinoma: a phase II study. Anticancer Drugs. 2007;18(4):487–491. | ||
Kouno T, Ando M, Yonemori K, et al. Weekly paclitaxel and carboplatin against advanced transitional cell cancer after failure of a platinum-based regimen. Eur Urol. 2007;52(4):1115–1122. | ||
Galsky MD, Mironov S, Iasonos A, Scattergood J, Boyle MG, Bajorin DF. Phase II trial of pemetrexed as second-line therapy in patients with metastatic urothelial carcinoma. Invest New Drugs. 2007;25(3):265–270. | ||
Fechner G, Siener R, Reimann M, Kobalz L, Albers P. Randomised phase II trial of gemcitabine and paclitaxel second-line chemotherapy in patients with transitional cell carcinoma (AUO Trial AB 20/99). Int J Clin Pract. 2006;60(1):27–31. | ||
Culine S, Theodore C, De Santis M, et al. A phase II study of vinflunine in bladder cancer patients progressing after first-line platinum-containing regimen. Br J Cancer. 2006;94(10):1395–1401. | ||
Vaishampayan UN, Faulkner JR, Small EJ, et al. Phase II trial of carboplatin and paclitaxel in cisplatin-pretreated advanced transitional cell carcinoma: a Southwest Oncology Group study. Cancer. 2005;104(8):1627–1632. | ||
Hoshi S, Ohyama C, Ono K, et al. Gemcitabine plus carboplatin; and gemcitabine, docetaxel, and carboplatin combined chemotherapy regimens in patients with metastatic urothelial carcinoma previously treated with a platinum-based regimen: preliminary report. Int J Clin Oncol. 2004;9(2):125–129. | ||
Vaughn DJ, Broome CM, Hussain M, Gutheil JC, Markowitz AB. Phase II trial of weekly paclitaxel in patients with previously treated advanced urothelial cancer. J Clin Oncol. 2002;20(4):937–940. | ||
Pagliaro LC, Millikan RE, Tu SM, et al. Cisplatin, gemcitabine, and ifosfamide as weekly therapy: a feasibility and phase II study of salvage treatment for advanced transitional-cell carcinoma. J Clin Oncol. 2002;20(13):2965–2970. | ||
Bellmunt J, Cos J, Cleries R, et al. Feasibility trial of methotrexate-paclitaxel as a second line therapy in advanced urothelial cancer. Cancer Invest. 2002;20(5–6):673–685. | ||
Sternberg CN, Calabro F, Pizzocaro G, Marini L, Schnetzer S, Sella A. Chemotherapy with an every-2-week regimen of gemcitabine and paclitaxel in patients with transitional cell carcinoma who have received prior cisplatin-based therapy. Cancer. 2001;92(12):2993–2998. | ||
De Mulder PH, Theodore C, Sella A, et al. Phase II EORTC trial with 5-fluorouracil, cisplatin and interferon-alpha as second-line treatment of advanced transitional cell cancer of the urothelial tract. Ann Oncol. 2000;11(11):1391–1394. | ||
Sweeney CJ, Williams SD, Finch DE, et al. A Phase II study of paclitaxel and ifosfamide for patients with advanced refractory carcinoma of the urothelium. Cancer. 1999;86(3):514–518. | ||
Witte RS, Elson P, Bono B, et al. Eastern Cooperative Oncology Group phase II trial of ifosfamide in the treatment of previously treated advanced urothelial carcinoma. J Clin Oncol. 1997;15(2):589–593. | ||
Pronzato P, Vigani A, Pensa F, Vanoli M, Tani F, Vaira F. Second line chemotherapy with ifosfamide as outpatient treatment for advanced bladder cancer. Am J Clin Oncol. 1997;20(5):519–521. | ||
Dreicer R, Gustin DM, See WA, Williams RD. Paclitaxel in advanced urothelial carcinoma: its role in patients with renal insufficiency and as salvage therapy. J Urol. 1996;156(5):1606–1608. | ||
von der Maase H, Hansen SW, Roberts JT, et al. Gemcitabine and cisplatin versus methotrexate, vinblastine, doxorubicin, and cisplatin in advanced or metastatic bladder cancer: results of a large, randomized, multinational, multicenter, phase III study. J Clin Oncol. 2000;18(17):3068–3077. | ||
Sonpavde G, Pond GR, Choueiri TK, et al. Single-agent taxane versus taxane-containing combination chemotherapy as salvage therapy for advanced urothelial carcinoma. Eur Urol. Epub 2015 Aug 8. | ||
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.