Back to Journals » Journal of Multidisciplinary Healthcare » Volume 15
Comparison of Pull and Introducer Techniques for Percutaneous Endoscopic Gastrostomy
Authors Li X, Wang JX, Wang YP, Shen JX, Zheng YX, Zhang PH, Wei JJ, Zhuang ZH
Received 20 January 2022
Accepted for publication 15 March 2022
Published 5 April 2022 Volume 2022:15 Pages 733—741
DOI https://doi.org/10.2147/JMDH.S356865
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Xia Li,1,2 Jun-Xi Wang,1 Yu-Ping Wang,1 Jia-Xin Shen,1 Yi-Xing Zheng,1 Pei-Hong Zhang,1 Jing-Jing Wei,1 Ze-Hao Zhuang1
1Endoscopy Center, First Affiliated Hospital of Fujian Medical University, Fuzhou, People’s Republic of China; 2Endoscope Room, Changle District Hospital, Fuzhou, People’s Republic of China
Correspondence: Ze-Hao Zhuang, Endoscopy Center, First Affiliated Hospital of Fujian Medical University, 20, Chazhong Road, Taijiang District, Fuzhou, 350005, Fujian Province, People’s Republic of China, Tel +860591-87981370, Fax +860591-87981371, Email [email protected]
Objective: To compare indications, success rates and complications of pull [P] and introducer [I] techniques for percutaneous endoscopic gastrostomy (PEG).
Methods: In this retrospective study, inpatients who underwent primary PEG tube insertion between January 2015 and February 2020 at the Endoscopy Center of the First Affiliated Hospital of Fujian Medical University were included.
Results: A total of 103 inpatients were included in this study (P group, n = 67; I group, n = 36). The rates of tube replacement within first six months in the P and I groups were 1.5% and 11.1%, respectively (P = 0.049). The most common primary indication of PEG was malignancy. The proportion of patients with esophageal cancer was significantly lower in the P group (24.4% vs 54.2%, P = 0.015). No significant difference was found in the overall, major, or minor complications between the two groups. In patients with esophageal stenosis, the pull method was a risk factor for complications (P = 0.03; odds ratio [OR] = 12, 95% confidence interval [CI]: 1.164– 123.684). Logistic regression analysis showed that the risk factors for major and minor complications were the admission-to-gastrostomy interval (OR = 1.078, 95% CI: 1.016– 1.145, P = 0.014) and lack of antibiotic use (OR = 4.735, 95% CI: 1.247– 17.979, P = 0.022), respectively.
Conclusion: Both PEG techniques have high clinical success rates. The introducer technique is more suitable for patients with esophageal stricture, which has lower minor complications, but higher rate of tube replacement compared to the pull technique. Use of antibiotics may reduce minor complications following PEG. Early PEG insertion may help to reduce post-PEG major complications.
Keywords: endoscopy, gastrostomy, enteral nutrition, indications, complications
Introduction
Compared to parenteral nutrition, enteral nutrition helps to maintain mucosal barrier protection,1 as well as improve the immunology and nutritional status of patients.2 Tube feeding can be considered for patients with poor oral intake due to various reasons such as neurological disorders, dysphagia, etc. A nasogastric tube is mainly used for temporary enteral feeding (< 4 weeks), while various gastrostomy and enterostomy techniques are used for long-term enteral feeding (> 4 weeks).3 Currently, percutaneous endoscopic gastrostomy (PEG) is the most widely used technique for the establishment of long-term tube feeding access. It requires endoscopic assistance but is preferred over surgery due to fewer contraindications, shorter operation time, and low incidence of serious complications.4,5
The three most commonly used methods of PEG insertion include the Ponsky-Gauderer (pull) method, the Sacks-Vine (push) method, and the Russell (introducer) method.6 With the pull method, the feeding tube is pulled from the mouth to the stomach over an endoscopically placed string in the reverse direction. With the push method, the feeding tube is pushed over a guide wire into the stomach and out of the puncture site. The steps and procedure-related complications of these two methods are similar, but the pull method is simpler in the clinical setting. Additionally, the overall complication rate of the push method has been reported to be significantly higher than that of the pull method (33% vs 21.4%, P = 0.047).7 With the introducer method, the tube is directly inserted into the stomach through the abdominal wall, which can reduce the risk of infection and tumor metastasis to a certain extent. It is useful in patients with severe oropharyngeal or esophageal stenosis where it is difficult to place the tube by the pull method. However, this method needs a special trocar, which increases the total operation time (12.6 vs 6.4 minutes, P = 0.0166)8 and cost.9 The maintenance of the balloon tube is also more complicated compared to bumper internal fixation of the pull method. For patients with advanced tumors or patients who can not receive sufficient oral intake for other reasons, if their nutritional status can be improved by gastrostomy, their quality of life will be greatly improved. This can also be regarded as the humanistic care of clinicians for terminally ill patients. This single-center study aimed to compare the indications and outcomes of the pull and introducer techniques for PEG placement and determine which of these techniques is more suitable for various patients to create access for enteral feeding.
Materials and Methods
Patient Selection
The clinical data of consecutive patients who underwent an endoscopic gastrostomy or enterostomy at the Endoscopy Center of The First Affiliated Hospital of Fujian Medical University from January 2015 to February 2020 were collected retrospectively. Patients with a jejunostomy, repeat PEG insertion, or those that were treated on an outpatient basis were excluded from this study. The enrollment process is shown in Figure 1. PEG was inserted by one of two techniques in this study: the pull method or the introducer method as described below. The patients were accordingly divided into either the pull (P) or introducer (I) group.
 |
Figure 1 Patient flow diagram with inclusion and exclusion data. |
Devices Used to Construct PEG
A flexible endoscope (GIF-XQ260/290, Olympus, Tokyo, Japan), a pull method gastrostomy kit (Flocare, Nutricia, Netherlands) and an introducer method gastrostomy kit (Cliny, Create Medic, Yokohama, Japan) were used in the current study.
Procedure of PEG Insertion
PEG insertion was performed by endoscopists with more than two years of experience in both pull and introducer techniques. The first and most important step of PEG insertion was identification of the puncture site using the abdominal wall transillumination test and finger pressure under endoscopic view. If the test failed, then a combination of X-ray images and ultrasound-assisted endoscopic water bladder positioning technology on the body surface and finger pressure were used to locate the puncture site.10
In the pull method, a small incision was made at the puncture site on the abdominal wall. Using a needle, a string was inserted through the abdominal wall and into the stomach, and then removed through the mouth using the endoscope. Subsequently, the string was fixed to the external end of the feeding tube and the tube was pulled from the mouth to the esophagus, and then out through the abdominal wall. Finally, the position of the bumper was confirmed under the endoscope, the tube was fixed, and the exposed scale was recorded.
With the introducer method, a gastropexy device was used to fix the stomach to the abdominal wall. First, the double needle of the gastropexy device was inserted into the gastric lumen. Next, a loop snare was formed from the tip of one needle, and a suture thread was inserted via the other. The suture thread was then caught by closing the loop snare and after the double needle was withdrawn from the stomach, the thread was tied outside the abdominal wall.12 After local anesthesia, a special trocar was inserted in the center of the two fixations, the needle core was withdrawn, a balloon feeding tube was inserted, and water was infused to complete the internal fixation. The complete procedure for the introducer method is shown in Figure 2.
Data Collection
Demographic data were collected for all patients, along with biochemical parameters such as liver and kidney function tests, antibiotic usage (use of antibiotics due to other infections before PEG insertion, prophylactic antibiotics to prevent infection, and no antibiotics), physical status according to the American Society of Anesthesiologists (ASA) classification (refer to as ASAPS),11 PEG indications, complications (major, systemic or life-threatening; minor, local or non-life-threatening; overall, both major and minor), and contributing factors related to procedure-related complications of the two groups. An esophageal stricture was defined as a narrowing that an endoscope with a diameter of 8.9 mm could not pass through.
Statistical Analysis
Statistical analyses were performed using IBM SPSS software (version 23.0, IBM, USA). The t-test was used to compare measured data, categorical data were compared using the chi-square test or Fisher’s exact probability test, and non-parametric data were assessed with the rank sum test (Mann–Whitney U-test). The logistic regression model was used to analyze the possible factors affecting the occurrence of PEG complications. The level of significance was set at P-value < 0.05.
Results
Baseline Characteristics
A total of 171 patients who underwent gastroenterostomy insertion were selected during the study period. One hundred and twenty-five patients undergoing primary PEG tube insertion were enrolled, and the percentages of outpatients and inpatients were 17.6% (22/125) and 82.4% (103/125), respectively. The percentages of inpatients that underwent the pull or introducer techniques were 82.7% (67/81) and 81.8% (36/44), respectively (P = 0.900). Due to incomplete clinical data, 22 outpatients were excluded, and finally 103 inpatients were included for analysis (P group, n = 67; I group, n = 36).
No significant difference was found between the two groups regarding baseline characteristics (P > 0.05; Table 1). Antibiotics were used for other infections before PEG insertion in 17 patients and 3 patients in the P group and I group, respectively. While, antibiotics were used for PEG prophylaxis in 8 patients and 4 patients in the P group and the I group, respectively. The proportion of patients with a negative transillumination test in the P group and I group were 2.99% (2/67) and 2.78% (1/36), respectively (P > 0.05). The number of patients requiring tube replacement within six months in the I group was greater compared to the P group [11.1% (4/36) vs 1.5% (1/67), P = 0.049].
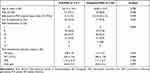 |
Table 1 Patient Characteristics |
Indications for PEG
The most common indication for PEG in both groups was malignant tumors, and the difference was not statistically significant (P > 0.05; Table 2). However, subgroup analysis based on the location of the cancer found that the proportion of patients with esophageal cancer in the P and I groups was 24.4% (10/41) and 54.2% (13/24), respectively (P = 0.015; Table 3).
 |
Table 2 Indications for Percutaneous Endoscopic Gastrostomy (PEG) [n (%)] |
 |
Table 3 Comparison of Complications Between the Two Groups [n (%)] |
Comparison of PEG-Related Complications
The complication rates and length of hospital stays in the two groups were similar (P > 0.05; Table 3). Pain was the most common minor complication. After stratifying patients with malignant tumors according to their tumor location, it was found that the complication rates of the two groups were similar in patients with head, neck and esophageal cancer (P = 0.648 and P = 0.052). After stratifying patients with malignant tumors according to the presence or absence of esophageal stenosis, it was found that in patients without esophageal stenosis, there was no significant difference in the incidence of complications between the two groups (P = 0.477), while in patients with esophageal stenosis, the P group was a risk factor for complications (P = 0.03; odds ratio [OR] = 12, 95% confidence interval [CI]: 1.164–123.684). All patients with esophageal stenosis received pre-PEG dilatation, and the complication rate in the P group was 50% (6/12), and in the I group was 7.69% (1/13).
Factors Affecting the Post-Procedure Complications
There was no significant correlation between PEG-related complications and ASA status of the patients. The risk factor for major complications was longer admission-to-gastrostomy interval while the lack of antibiotics was associated with higher rates of minor complications. (Table 4).
 |
Table 4 Multivariate Analysis of the Factors Affecting Complications |
Discussion
In this study, the most common indications for PEG in both study groups were malignancy followed by neurological disorders, which is different than that reported by Western-based studies.4,12 In addition to the factors associated with disease occurrence and survival time, it also reflects the differences in understanding the benefits of PEG between Chinese and Western doctors, and patients’ lower acceptance of PEG. Patient factors that influence PEG decision-making include appearance, fear of becoming a burden, worry of unknown technology and prognosis, and differences in values and beliefs.13 The life expectancy of patients with neurological diseases is often longer than that of patients with cancer, so the influence of the above-mentioned factors is greater.
In patients with head and neck cancers that have esophageal strictures due to radiotherapy or the tumor itself, the success rate of the pull method is reduced to 80–90%.14,15 Moreover, the use of a small endoscope cannot guarantee the smooth passage of the tube, and up to 23% of cases require prior endoscopic dilation, which also increases the risk of bleeding and perforation (1–3%).16,17 The I group was dominated by patients with esophageal cancer (54.2%, 13/24; P = 0.015), and the proportion of esophageal stenosis was as high as 100% (13/13). Meanwhile, among patients with esophageal stenosis, the risk of complications in the P group was 12 times than that of I group (P = 0.030). These findings indicated that the introducer method is more suitable for cases of severe esophageal stenosis in which the pull method would be difficult to perform. However, the proportion of tube replacements within the first six months in the I group was higher than that in the P group [11.1% (4/36) vs 1.5% (1/67), P = 0.049], which is likely due to the short life of the balloon catheter,18 and is complicated by the process of balloon replacement18 and the smaller diameter of the feeding tube.19
In this study, the overall, major, and minor complications in the two groups were similar (P = 0.122, P = 1.000, and P = 0.187, respectively). The admission-to-gastrostomy interval was the single most important risk factor for major complications (OR = 1.078, 95% CI: 1.016–1.145; P = 0.014). The longer admission-to-gastrostomy interval indicated the poor clinical condition of the patient and advanced stage of cancer. Moreover, as PEG is an invasive procedure, it often used as a last resort, so the optimal time for PEG insertion is often missed.
A large retrospective cohort analysis of all adult inpatients undergoing PEG placement in the United States found that all-cause in-hospital mortality rates of PEG dropped from 10.8% to 6.6% over a 10-year time period (P < 0.001).20 However, the incidence of complications remained the same over the 10-year time period (4.4% vs 5.1%, P = 0.2). Moreover, the total number of cases decreased from 174,228 to 155,550. The authors believed that this mainly reflected changes to the indications and timing of PEG insertion. Among them, the head and neck cancer group had the lowest mortality rate (3.0%), which may be related to the early acceptance of PEG in this group. On the contrary, patients with advanced cancer and dementia often have more complications and higher rates of mortality following PEG.21 “Early” placement refers to undergoing PEG before the underlying disease causes severe malnutrition and weight loss,21 which is important for patients to truly benefit from PEG.
The incidence of minor complications and postoperative pain was higher in the P group but the difference was not statistically significant. Studies have reported that the incidence of postoperative pain after PEG with the introducer method using a conventional diameter trocar (5.5–6.0 mm) was only 3.6% (5/137),22 while in another study using a 10 mm trocar, 60% of patients still had slight pain on the 10th day after surgery, suggesting that larger skin incisions increase postoperative pain.23 However, in general, a 4 mm difference in the skin incision is unlikely to cause a significant difference in postoperative pain. However, since the larger diameter (10 mm) incision does not tightly fit the feeding tube (outer diameter is 6 mm), it is necessary to routinely rotate the tube to prevent buried bumper syndrome in the initial period, and the frequent involvement of the feeding tube by movements such as turning over may cause repeated tears in the wound, thereby prolonging the length of postoperative incisional pain.
The incidence of infection surrounding the PEG site following the pull method is 26% to 35%,24 which is related to the contamination of the tube with oral microbiota during tube insertion.25 In general, the prophylactic use of antibiotics can reduce the local infection rate after PEG to 7–14%.26 In the current study, the incidence of infection in the P group was 4.5% (3/67), which was significantly lower than that reported in the literature. This low infection rate may be related to better technology during insertion and nursing. It also may be due to underreporting of mild infections as local pain. Logistic regression analysis showed that the lack of antibiotics was a risk factor for minor complications (OR = 4.735, 95% CI: 1.247–17.979; P = 0.022).
Interestingly, the proportion of antibiotics used in the I group was lower than that in the P group, but no infection occurred in the I group. In the introducer method, the feeding tube was directly inserted into the stomach through the abdominal wall. So, the chance of infection was significantly lower compared to the pull method.24 Martins et al8 found that the introducer method without antibiotics has a lower infection rate compared to the pull method with prophylactic antibiotics. Hence, the European Society of Parenteral and Enteral Nutrition (ESPEN) guidelines do not recommend the routine use of prophylactic antibiotics for PEG placement by the introducer method.
Studies have reported that gastric metastasis occurs in approximately 0.5–1.0% of patients with throat and esophageal cancer following the pull method due to tumor seeding during the transoral passage.27–29 Some studies found that the mean interval between PEG placement and tumor seeding was 7.8 ± 5.2 months.26 However, in this study the outcomes were recorded up to the day of discharge and the mean duration of hospital stay was 19 days. Hence, the effect of the PEG insertion technique on tumor seeding could not be observed in this study.
There are some limitations to this study. Firstly, it was a single center retrospective study with small sample size. Many details such as the cost of procedure, timing and severity of postoperative pain, reasons for PEG tube replacement, etc. were not available. Secondly, the follow up period was short and lacked a unified evaluation of complications. Hence, future larger prospective studies with long-term follow up are required to study the impact of these methods on the incidence of tumor implantation, long-term complications, and prognosis.
Conclusion
In conclusion, this study found that both the pull and introducer methods for PEG placement have high clinical success. The introducer technique may be more suitable for patients with severe esophageal stenosis. It has a lower incidence of minor complications but a higher rate of tube replacements within the first six months. Early PEG placement after admission and use of prophylactic antibiotics may reduce the incidence of major and minor complications, respectively.
Ethics Approval and Informed Consent
The comments of Ethics Committee of First Affiliated of Fujian Medical University are as follows: On Apr. 3rd, 2019, According to the national ethical principles of Good Clinical Practice, Declaration of Helsinki and Measures for the Ethical Review of Biomedical Research Involving Humans: a meeting ethical review of the project was conducted, and the project is approved to be carried out in our hospital.
The Institutional Review Board (IRB) declares that: In accordance with the requirements of ICH-GCP, China GCP and relevant laws and regulations or guidelines in China, the review and other working processes are free from any influence of any organization or individuals other than this Ethics Committee.
The Ethics Committee of First Affiliated of Fujian Medical University waived the need for patient consent to review their medical records as the confidentiality of patient data was maintained.
Acknowledgments
The authors report no grants or financial support for this work.
Author Contributions
Xia Li designed the study, extracted and analyzed data, interpreted results and wrote and substantially revised the manuscript. Ze-Hao Zhuang designed the study, substantially revised and critically reviewed the article. Jun-Xi Wang and Jing-Jing Wei made a significant contribution to acquisition of data and analysis, and took part in drafting and reviewing the article. Yu-Ping Wang, Jia-Xin Shen, Yi-Xing Zheng and Pei-Hong Zhang made a contribution to acquisition of data and analysis, and took part in drafting the manuscript. And all authors gave final approval of the version to be published, have agreed on the journal to which the article has been submitted and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Nature Science Foundation of Fujian province (Grant Numbers: 2019J01447 and 2020J01974) and Fujian Provincial Health Technology Project (No.2020TG012).
Disclosure
Dr Ze-Hao Zhuang reports a patent “An internal fixed gastroenterostomy replacement device with memory” issued. The authors report no other conflicts of interest in this work.
References
1. Schorghuber M, Fruhwald S. Effects of enteral nutrition on gastrointestinal function in patients who are critically ill. Lancet Gastroenterol Hepatol. 2018;3(4):281–287. doi:10.1016/S2468-1253(18)30036-0
2. Gramlich L, Kichian K, Pinilla J, Rodych NJ, Dhaliwal R, Heyland DK. Does enteral nutrition compared to parenteral nutrition result in better outcomes in critically ill adult patients? A systematic review of the literature. Nutrition. 2004;20(10):843–848. doi:10.1016/j.nut.2004.06.003
3. Farrag K, Shastri YM, Beilenhoff U, Aksan A, Stein J. Percutaneous endoscopic gastrostomy (PEG): a practical approach for long term management. BMJ. 2019;364:k5311. doi:10.1136/bmj.k5311
4. Wollman B, D’Agostino HB, Walus-Wigle JR, Easter DW, Beale A. Radiologic, endoscopic, and surgical gastrostomy: an institutional evaluation and meta-analysis of the literature. Radiology. 1995;197(3):699–704. doi:10.1148/radiology.197.3.7480742
5. Rustom IK, Jebreel A, Tayyab M, England RJ, Stafford ND. Percutaneous endoscopic, radiological and surgical gastrostomy tubes: a comparison study in head and neck cancer patients. J Laryngol Otol. 2006;120(6):463–466. doi:10.1017/S0022215106000661
6. Hucl T, Spicak J. Complications of percutaneous endoscopic gastrostomy. Best Pract Res Clin Gastroenterol. 2016;30(5):769–781. doi:10.1016/j.bpg.2016.10.002
7. Köhler G, Kalcher V, Koch OO, Luketina RR, Emmanuel K, Spaun G. Comparison of 231 patients receiving either “pull-through” or “push” percutaneous endoscopic gastrostomy. Surg Endosc. 2015;29(1):170–175. doi:10.1007/s00464-014-3673-9
8. Martins FP, Sousa MC, Ferrari AP. New “introducer” PEG-gastropexy with T fasteners: a pilot study. Arq Gastroenterol. 2011;48(4):231–235. doi:10.1590/S0004-28032011000400003
9. Okumura N, Tsuji N, Ozaki N, et al. Percutaneous endoscopic gastrostomy with Funada-style gastropexy greatly reduces the risk of peristomal infection. Gastroenterol Rep. 2015;3(1):69–74. doi:10.1093/gastro/gou086
10. Yang ZY, Wei JJ, Zhuang ZH, Zhang J, Xu YT, Huang XH. Balloon-assisted ultrasonic localization: a novel technique for direct percutaneous endoscopic jejunostomy. Eur J Clin Nutr. 2018;72(4):618–622. doi:10.1038/s41430-018-0115-0
11. Doyle DJ, Goyal A, Bansal P, Garmon EH. American Society of Anesthesiologists Classification. Treasure Island (FL): StatPearls; 2021.
12. Toh Yoon EW, Yoneda K, Nakamura S, Nishihara K. Percutaneous endoscopic gastrostomy (PEG) using a novel large-caliber introducer technique kit: a retrospective analysis. Endosc Int Open. 2016;4(9):E990–6. doi:10.1055/s-0042-112587
13. Lin LC, Li MH, Watson R. A survey of the reasons patients do not chose percutaneous endoscopic gastrostomy/jejunostomy (PEG/PEJ) as a route for long-term feeding. J Clin Nurs. 2011;20(5–6):802–810. doi:10.1111/j.1365-2702.2010.03541.x
14. Riley DA, Strauss M. Airway and other complications of percutaneous endoscopic gastrostomy in head and neck cancer patients. Ann Otol Rhinol Laryngol. 1992;101(4):310–313. doi:10.1177/000348949210100404
15. Gibson SE, Wenig BL, Watkins JL. Complications of percutaneous endoscopic gastrostomy in head and neck cancer patients. Ann Otol Rhinol Laryngol. 1992;101(1):46–50. doi:10.1177/000348949210100113
16. Toyama Y, Usuba T, Son K, et al. Successful new method of extracorporeal percutaneous endoscopic gastrostomy (E-PEG). Surg Endosc. 2007;21(11):2034–2038. doi:10.1007/s00464-007-9270-4
17. Stockeld D, Fagerberg J, Granstrom L, Backman L. Percutaneous endoscopic gastrostomy for nutrition in patients with oesophageal cancer. Eur J Surg. 2001;167(11):839–844. doi:10.1080/11024150152717670
18. Dormann AJ, Huchzermeyer H. Endoscopic techniques for enteral nutrition: standards and innovations. Dig Dis. 2002;20(2):145–153. doi:10.1159/000067486
19. Dormann AJ, Wejda B, Kahl S, Huchzermeyer H, Ebert MP, Malfertheiner P. Long-term results with a new introducer method with gastropexy for percutaneous endoscopic gastrostomy. Am J Gastroenterol. 2006;101(6):1229–1234. doi:10.1111/j.1572-0241.2006.00541.x
20. Stein DJ, Moore MB, Hoffman G, Feuerstein JD. Improving all-cause inpatient mortality after percutaneous endoscopic gastrostomy. Dig Dis Sci. 2021;66(5):1593–1599. doi:10.1007/s10620-020-06396-y
21. Dietrich CG, Schoppmeyer K. Percutaneous gastrostomy – too often? Too late? Who are the right patients for gastrostomy? World J Gastroenterol. 2020;26(20):2464–2471. doi:10.3748/wjg.v26.i20.2464
22. Retes FA, Kawaguti FS, de Lima MS, et al. Comparison of the pull and introducer percutaneous endoscopic gastrostomy techniques in patients with head and neck cancer. United Eur Gastroenterol J. 2017;5(3):365–373. doi:10.1177/2050640616662160
23. Giordano-Nappi JH, Maluf-Filho F, Ishioka S, et al. A new large-caliber trocar for percutaneous endoscopic gastrostomy by the introducer technique in head and neck cancer patients. Endoscopy. 2011;43(9):752–758. doi:10.1055/s-0030-1256495
24. Veitch AM, Vanbiervliet G, Gershlick AH, et al. Endoscopy in patients on antiplatelet or anticoagulant therapy, including direct oral anticoagulants: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guidelines. Endoscopy. 2016;48(4):385–402. doi:10.1055/s-0042-102652
25. Santos PM, McDonald J. Percutaneous endoscopic gastrostomy: avoiding complications. Otolaryngol Head Neck Surg. 1999;120(2):195–199. doi:10.1016/S0194-5998(99)70406-7
26. Lipp A, Lusardi G. Systemic antimicrobial prophylaxis for percutaneous endoscopic gastrostomy. Cochrane Database Syst Rev. 2013;11:CD005571.
27. Cappell MS. Risk factors and risk reduction of malignant seeding of the percutaneous endoscopic gastrostomy track from pharyngoesophageal malignancy: a review of all 44 known reported cases. Am J Gastroenterol. 2007;102(6):1307–1311. doi:10.1111/j.1572-0241.2007.01227.x
28. Ellrichmann M, Sergeev P, Bethge J, et al. Prospective evaluation of malignant cell seeding after percutaneous endoscopic gastrostomy in patients with oropharyngeal/esophageal cancers. Endoscopy. 2013;45(7):526–531. doi:10.1055/s-0033-1344023
29. Teh JL, Wong RK, Gowans M, et al. Gastric metastases of oral carcinoma resulting from percutaneous endoscopic gastrostomy placement via the introducer technique. Gastroenterol Rep. 2013;1(3):211–213. doi:10.1093/gastro/got027
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

