Back to Journals » Clinical Interventions in Aging » Volume 14
Comparison of prognostic values of high-sensitivity cardiac troponin T and N-terminal prohormone brain natriuretic peptide to assess mortality in elderly inpatients
Authors Chen JR, Wang Q, Wu W, Zhang SJ
Received 16 September 2018
Accepted for publication 3 December 2018
Published 31 December 2018 Volume 2019:14 Pages 81—90
DOI https://doi.org/10.2147/CIA.S187757
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Zhi-Ying Wu
Jie-Ruo Chen,1 Qing Wang,1 Wei Wu,2 Shao-Jing Zhang1
1Department of Geriatrics, Fuxing Hospital, affiliated to Capital Medical University, Beijing, China; 2General Practice Ward, Fuxing Hospital, affiliated to Capital Medical University, Beijing, China
Background: Studies have shown that increases in low-level high-sensitivity cardiac troponin T (hs-cTnT) and N-terminal prohormone brain natriuretic peptide (NT-proBNP) in the elderly population lead to high risk of adverse clinical outcomes, such as mortality. In this study, associations between the two biomarkers and long-term mortality in elderly patients hospitalized for medical conditions other than acute cardiovascular events were investigated. A comparison of the predictive value of hs-cTnT and NT-proBNP for all-cause mortality was conducted.
Methods: A cohort of 715 elderly inpatients free of acute cardiovascular events was initially recruited. Based on tertiles of baseline hs-cTnT and NT-proBNP levels, the elderly were arranged into low, middle, and high groups. The mortality of each group was observed and the predictive values of hs-cTnT and NT-proBNP compared. Additionally, all-cause mortality was analyzed for hs-cTnT and NT-proBNP combined.
Results: There were 135 (18.9%) all-cause mortality cases identified during follow-up (median 47 months). The upper tertile of hs-cTnT was significantly associated with an increased risk of mortality (HR 3.29, 95% CI 1.85–5.85), even after adjustment for potential confounders. However, there were no significant differences observed in mortality rates among the three NT-proBNP groups after adjustment for potential confounders (HR 1.77, 95% CI 0.83–3.17). Compared to NT-proBNP, hs-cTnT was a better predictor of mortality, as area under curves for hs-cTnT and NT-proBNP at 60 months were 0.712 (95% CI 0.616–0.809) and 0.585 (95% CI 0.483–0.6871), respectively. Also, the combination of the two cardiac biomarkers did not render a better predictive value for mortality than hs-cTnT alone.
Conclusion: Unlike hs-cTnT, baseline NT-proBNP levels failed to show an independent association with all-cause mortality in hospitalized elderly without acute cardiovascular events. hs-cTnT provided significant prognostic value for mortality in the study cohort.
Keywords: high-sensitivity cardiac troponin T (hs-cTnT), N-terminal prohormone brain natriuretic peptide (NT-proBNP), nonacute cardiovascular events, elderly patients
Introduction
The cardiac biomarkers high-sensitivity cardiac troponin T (hs-cTnT) and N-terminal prohormone brain natriuretic peptide (NT-proBNP) have been demonstrated to provide prognostic information for cardiovascular disease and mortality in a variety of populations.1–4 These two cardiac biomarkers can also help in cardiovascular disease risk stratification and improvement in patient management.5 NT-proBNP release is stimulated by ventricular overload from pressure or volume, and its concentration increases with elevating left ventricular (LV) mass.6 However, hs-cTnT, a component of the heart muscle, may increase in response to myocardial injury or myocardial remodeling.2 Moreover, studies have confirmed that hs-cTnT and NT-proBNP can be detected not only in patients with coronary heart disease or heart failure but also in a general population, such as the elderly.7,8 In apparently healthy and community-dwelling older adults, elevated hs-cTnT and NT-proBNP have been shown to be associated with poor cardiovascular outcomes including acute cardiovascular events and mortality.2,4,9 This evidence raises two questions. Is the predictive power of these two cardiac biomarkers consistent in elderly patients? Further, is the prognostic performance of the combination of the two biomarkers better than that of each alone? The present study aimed to compare the predictive values of hs-cTnT and NT-proBNP for long-term mortality in elderly patients hospitalized for medical conditions other than acute cardiovascular events. We also investigated the association between a combination of the biomarkers and mortality.
Methods
Patients
A total of 715 patients who had been admitted to the Department of Geriatrics at our hospital in June 2010 were recruited for this prospective observational study. All patients were >65 years old and provided signed informed consent before admission. Patients with acute coronary syndrome (ACS), acute or chronic cardiac failure, malignancies, and a history of hemodialysis or dementia were excluded. Patients were routinely examined by electrocardiography, ultrasound cardiography, and for cardiac biomarkers at entry, and ACS was excluded according to the fourth universal definition of myocardial infarction (2018).10 Acute or chronic heart failure was excluded according to patient medical history, hospitalization symptoms, physical signs combined with ultrasound cardiography, and NT-proBNP. Malignancies were excluded according to patient medical history and biomarkers for cancer after entrance. If a new tumor was diagnosed after enrollment, the patient’s information would be removed from the data. Patients with dementia were excluded according to Mini-Mental State Examination scores. The study was approved by the ethics committee of Fuxing Hospital (affiliated with Capital Medical University), and was conducted in accordance with the Declaration of Helsinki.
Data collection
Baseline characteristics of patients were recorded at entrance: age, sex, body-mass index, heart rate, blood pressure, and smoking status (never, former/current). Comorbidities were also recorded: hypertension, diabetes mellitus (DM), atrial fibrillation (AF), stable coronary artery disease, cerebral infarction, chronic kidney disease (CKD), and COPD. Blood biochemistry was assessed from fasting blood samples drawn on the day after entrance, when patients had been on an absolute diet for >12 hours: hemoglobin (Hb), ALT, estimated glomerular filtration rate (eGFR), total cholesterol (TC), triglycerides (TG), high-density-lipoprotein cholesterol (HDL-C), and low-density lipoprotein-cholesterol (LDL-C). eGFR was calculated based on the formula eGFR 175 × (serum creatinine/88.4) − 1.234 × (age) − 0.179 (female × 0.79),5 and eGFR <60 mL/min·1.73 m2 was considered decreased renal function.
hs-cTnT concentration was measured using an Elecsys Troponin T Stat immunoassay, while NT-proBNP concentration was determined on an Elecsys proBNP II (Roche Diagnostics). Both analyses were performed at the laboratory of our hospital using automatic analyzers according to recommendations from the manufacturer.
Echocardiography
Ultrasound cardiography was performed with patients on their left sides and breathing regularly, and standardized two-dimensional echocardiography was conducted in accordance with the recommendations from the American Society of Echocardiography. The stability of the instrument was evaluated by the quality-control technician before examination. The LV ejection fraction (LVEF) was measured under apical four-chamber and two-chamber views using a modified single-plane Simpson method. The weight and height of each patient was recorded and body-surface area calculated. The LV mass was determined by the Devereux method, and LV mass index (LVMI) was calculated by LV mass and body-surface area.
End point
Follow-up was conducted each 3 months through phone or home visits by our follow-up group after discharge. Our outcome was all-cause mortality.
Statistical analysis
Statistical analysis was performed using SPSS version 22.0 and R version 3.4.4. Continuous variables were expressed as means ± SD or medians and IQR, and categorical variables as frequency with percentage of total. Patients were classified into three groups (low, middle, and high) based on tertiles of hs-cTnT and NT-proBNP concentrations. One-way ANOVA or Kruskal–Wallis tests were used for continuous variables and χ2 for categorical variables. Cumulative survival curves were constructed by the Kaplan–Meier method and compared with log-rank tests. Cox proportional hazard-regression models were created to analyze relationships between the two biomarkers or their combination with all-cause mortality. HRs and 95% CIs for the high and middle hs-cTnT and NT-proBNP groups were obtained using the low group as the reference category. Receiver-operating characteristic (ROC) curves and time-dependent ROC curves were constructed to evaluate discriminative capacity for mortality of different biomarkers and to analyze which biomarker had higher predictive value for mortality by comparing area under the curve (AUC). P-values were considered indicative of statistical significance when lower than 0.05.
Results
Patient characteristics
Baseline characteristics of patients are shown in Tables 1 and 2. Among the 715 patients, the mean age was 82.4±6.0 years, and 470 (65.7%) were male. The median (IQR) of NT-proBNP was 290.6 (130.40–631.06) pg/mL and ranged from 9.5 to 14,226 pg/mL, while the median (IQR) of hs-cTnT was 0.013 (0.009–0.020) ng/mL and ranged from 0.003 to 0.109 ng/mL. There were 319 (44.2%) patients with hs-cTnT values higher than the clinical cutoff point (99th percentile upper reference limit 14 ng/L). NT-proBNP values in 59 patients (8.0%) were greater than the clinical age-related cutoff points (900 pg/mL for 50–75 years, 1,800 pg/mL for >75 years).5 The most common comorbidity was hypertension (80.0%), followed by stroke (60.4%).
According to the tertiles of NT-proBNP and hs-cTnT levels (NT-proBNP 130.4 and 631.06 pg/mL, hs-cTnT 0.009 and 0.020 ng/mL), patients were stratified into high, middle, and low groups to compare baseline characteristics. As shown in Tables 1 and 2, patients were likely to be older and have significantly elevated LVMI levels across the three tertiles of hs-cTnT and NT-proBNP. The same tendency was observed in the proportion of patients with stable coronary artery disease and CKD. In contrast, TC, TG, and LDL-C concentrations, eGFR levels, Hb concentrations, and LVEF levels declined significantly across the three tertiles of both hs-cTnT and NT-proBNP. However, significant decreases in HDL-C concentrations were observed only across the three tertiles of hs-cTnT. Patients with a high proportion of hypertension, COPD, and DM were classified in a higher tertile of hs-cTnT, as well as males. Increases in heart rate and proportion of AF history were observed at higher levels in NT-proBNP groups. There were no significant differences in hs-cTnT and NT-proBNP groups for body-mass index, blood pressure, smoking status, ALT concentrations, or cerebral infarction.
Biomarkers as predictors of mortality
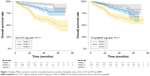
After 12–75 months of follow-up (median 47 months), 135 (18.9%) all-cause deaths were identified in the cohort, of which 108 (80%) were noncardiac. These mortalities were compared among each tertile group of the two cardiac biomarkers. As shown in Figure 1, the high group of NT-proBNP (Tertile 3) was related to a higher proportion of mortality compared with the middle group (tertile 2) and low group (tertile 1), and the log-rank test result was significant (54.1% vs 30.3% vs 15.6%, P<0.001). Furthermore, significant increases in mortality were also observed across the three tertiles of hs-cTnT (62.2% vs 26.0% vs 1.8%, P<0.001).
As shown in Table 3, NT-proBNP and hs-cTnT levels were both significantly associated with high mortality risks. HRs for death in the NT-proBNP tertiles were 4.13 (95% CI 2.52–6.79) in the high group and 1.98 (95% CI 1.16–3.38) in the middle group compared with the corresponding low group. In tertiles of hs-cTnT, HRs for death were 2.66 (95% CI 1.47–4.82) in the middle group and 7.22 (95% CI 4.23–12.34) in the high group. In multivariate Cox analyses, as shown in model 2 after adjusting for age and sex, the risk of death in the high NT-proBNP group was 2.76-fold (95% CI 1.66–4.60) higher than in the low group. Moreover, as shown in model 3, after adjustment for age, sex, heart rate, comorbidities, and blood-biochemistry parameters, the HR for death in the high group of NT-proBNP was 2.55 (95% CI 1.50–4.34) compared with the reference – tertile 1. However, after adjusting model 3 for LVEF and LVMI, there were no significant associations observed in death rates among the NT-proBNP groups, suggesting that NT-proBNP provides no reliable prognostic information independently of LV parameters. In addition, model 5 illustrated that the association between NT-proBNP and mortality remained poor after adjusting model 4 for hs-cTnT.
There were significant increases in mortality risk across the three tertiles of hs-cTnT (HR 1 vs 1.99 vs 4.69, P<0.05) in the age- and sex-adjusted analysis (model 2). These associations remained strong (HR 1 vs 1.86 vs 4.29, P<0.05), even after adjustment for age, sex, heart rate, comorbidities, and blood-biochemistry parameters, as shown in model 3. Moreover, after adjustment for potential confounders, including NT-proBNP, as shown in models 4 and 5, hs-cTnT still had robust prognostic value for mortality in this cohort. These results suggested that unlike NT-proBNP, hs-cTnT was an independent predictor for mortality in the study cohort.
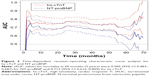
Mortality based on comparison and combination of biomarkers
To evaluate the discriminative capacity for mortality of NT-proBNP and hs-cTnT, ROC curves were constructed (Figure 2). For NT-proBNP, the incremental AUC (iAUC) was 0.700 (95% CI 0.651–0.748) and the predicted cutoff value was 386.15 pg/mL. At this time, predicted sensitivity was 68.9%, specificity 64.5%, and positive predictive value 31.1%. The Youden index was 0.334. For hs-cTnT, iAUC was 0.743 (95% CI 0.697–0.788) and predicted cutoff value was 0.016 ng/mL. At this time, predicted sensitivity was 65.9%, specificity 71.2%, positive predictive value 34.8%, and Youden index 0.371. Furthermore, we drew time-dependent ROC curves for each biomarker over follow-up, as shown in Figure 3. At each time point, the difference between estimated AUCs of the biomarkers was significant (P<0.001). For instance, iAUC values for NT-proBNP and hs-cTnT at 60 months (5 years) were 0.585 (95% CI 0.483–0.687) and 0.712 (95% CI 0.616–0.808), respectively. All of them were adjusted by potential confounders, including age, sex, heart rate, coronary artery disease, CKD, AF, TC, TG, LDL-C, HDL-C, Hb, eGFR, DM, AF, COPD, hypertension, LVEF, LVMI, NT-proBNP, or hs-cTnT. These results indicated that hs-cTnT was a better predictor of mortality than NT-proBNP.
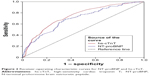  | Figure 2 Receiver-operating characteristic curves for NT-proBNP and hs-cTnT. |
Additionally, another Cox analysis model was conducted to analyze mortality using tertiles of a combination of hs-cTnT and NT-proBNP. Table 4 displays HRs for mortality with joint hs-cTnT and NT-proBNP after adjusting for age, sex, heart rate, comorbidities, blood-biochemistry parameters, and echocardiography. The increase in mortality in the higher tertiles of hs-cTnT levels was significant, while the correlation was not as significant in NT-proBNP. As shown in Table 4 and Figure 4, the combination of the high hs-cTnT group and middle NT-proBNP group was significantly associated with mortality (HR 3.62, 95% CI 1.28–10.20). The same correlation was observed between mortality and combination of the middle hs-cTnT group and high NT-proBNP group (HR 3.01, 95% CI 1.05–8.63). These associations indicated that the risk of mortality increased as the two biomarkers both increased. Furthermore, there was a significant association between mortality and combination of the upper tertiles of both hs-cTnT and NT-proBNP. However, the HR for death was 3.36 (95% CI 1.19–9.54), indicating that the combination of the two cardiac biomarkers did not render a better predictive value for mortality than hs-cTnT alone.
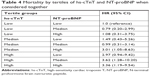  | Table 4 Mortality by tertiles of hs-cTnT and NT-proBNP when considered together |
  | Figure 4 Mortality based on the combination of hs-cTnT and NT-proBNP. |
Discussion
Our previous study demonstrated the slight elevation of hs-cTnT levels in elderly inpatients except for acute cardiovascular events, which was also associated with an increased risk of all-cause mortality after discharge.11 Other studies have shown that the cardiac biomarker NT-proBNP is also predictive of death, and thus we also measured NT-proBNP in this population. However, after adjustment for potential confounders, there were no associations with mortality rates among the NT-proBNP groups, and the predictive value of hs-cTnT for all-cause death was better than that of NT-proBNP. Compared with NT-proBNP, hs-cTnT was a better prognostic biomarker for mortality in the elderly population.
Previous studies have found that NT-proBNP still provides significant prognostic value for mortality in community-dwelling elderly people without heart failure, even after accounting for death-related risk factors, such as the ultrasonic indicators LVMI and LVEF.4,12,13 NT-proBNP release is stimulated by ventricular stretch, and is strongly related to LV dysfunction and structural abnormalities.14 Independently of heart-failure diagnosis, other factors, such as older age,15 anemia,16 AF,17 and renal function decline,18 have also been confirmed to lead to increased ventricular pressure, which in turn stimulates the elevated release of NT-proBNP and increases the risk of mortality. However, the present study did not find a relationship between mortality and NT-proBNP. In this study, the proportion of people who had elevated NT-proBNP concentrations above the age-related cutoffs was small (8%), which may suggest that few patients had LV pressure or volume overload. In line with most previous studies on apparently healthy community-dwelling people,2 noncardiac critically ill patients,19 and nursing home residents,20 the present study also found that hs-cTnT was an independent predictor for all-cause mortality in elderly inpatients without acute cardiovascular events. People with increased hs-cTnT levels are generally aged and have a relatively short life expectancy.7 Even without acute cardiovascular events, cardiac structural abnormalities and various comorbidities are often present, leading to potential myocardial ischemia and hypoxia risk and further explaining the increased risk of death.21–24
Several studies have compared the predictive power of hs-cTnT and NT-proBNP for adverse outcomes, and majority of patients included in were end-stage renal disease (ESRD).25–28 Apple et al28 conducted a follow-up study in ESRD patients and found that cTnT and cTnI were independently predictive of all-cause mortality, while elevated NT-proBNP levels based on normal cutoffs (age <75 years, 125 ng/L; ≥75 years, 450 ng/L) were not predictive of death. Normally, baseline levels of NT-proBNP in ESRD patients are higher than those of the general population, due to the decline in renal clearance mechanisms, which may explain in this study why NT-proBNP provided a poor prognostic value for death, since 99% of patient levels were above the normal cutoffs. Oh et al29 analyzed mortality in incident hemodialysis patients, and found that compared to cTnT, NT-proBNP was a better prognostic biomarker of mortality and independently predictive of mortality. Compared with other studies on the correlation between mortality and TnT in ESRD patients, median cTnT (0.05 ng/mL) in this study was only half the reference levels,30,31 while that of NT-proBNP was comparable to studies analyzing the association between NT-proBNP and mortality in patients with incident hemodialysis.27,32 Kim et al25 investigated the associations of hs-cTnT and NT-proBNP with risk of ESRD in a general community-based population, and found that both hs-cTnT and NT-proBNP were independent predictors of ESRD risk, although the results for hs-cTnT showed greater significance. These findings suggested the important involvement of cardiac damage, rather than ventricular overload, in the decline in kidney function. In addition, hs-cTnT levels may reflect end-stage organ damage or systemic pathophysiological processes, such as microvascular disease.33,34
In the present study, hs-cTnT and NT-proBNP were compared in elderly inpatients without acute cardiovascular events to assess their predictive values for mortality after discharge. The results showed an elevation in low-level hs-cTnT and a high proportion (44.2%) of patients whose hs-cTnT levels increased above the clinical cutoffs. However, the proportion of patients with elevated NT-proBNP levels above the age-related cutoffs was only 8.0%. Furthermore, the results demonstrated that hs-cTnT levels, but not NT-proBNP levels, are significantly predictive of all-cause mortality. These findings suggested that in this study cohort, the number of patients with potential myocardial ischemia was large, while the number of patients with cardiac overload or dysfunction was small.
Independently of acute cardiovascular events, the increased low-level hs-cTnT in this study was due to a number of factors. First, the study focused on an elderly cohort. With increasing age, individuals may experience cardiac aging, increased cell metabolism and apoptosis, and damage to the myocardial vascular endothelium, all of which lead to increased release of cTn from cardiomyocytes.7 Second, the median (IQR) of the eGFR in this study was 71.82 (58.1–87.1) mL/min/1.73 m2. Decreased eGFR results in a decline in cTn metabolism.35 Third, various comorbidities, such as DM, may cause cardiac structural and functional abnormalities, which lead to increased cTn release.22,36
Another distinctive feature in our study was that we conducted an additional Cox analysis to evaluate the predictive performance of hs-cTnT and NT-proBNP when combined for all-cause mortality. The mortality risk increased when the two cardiac biomarkers were both elevated, but the combination of them did not improve the close association with mortality compared to hs-cTnT alone.
There are several limitations in our study. First, we measured levels of biomarkers and performed echocardiography only once patients were in hospital. Unfortunately, we did not examine follow-up changes in these influential factors after discharge. Therefore, it is difficult to examine whether long-term fluctuation in the two biomarkers had any influence on clinical outcomes in this elderly population. Second, symptoms of myocardial ischemia are not typical in the elderly. Therefore, acute cardiovascular events, such as ACS, may not have been completely excluded in this study cohort. Third, information about medication taking was not collected adequately in this study, eg, angiotensin-converting enzyme inhibitors, angiotensin-receptor blockers, diuretics, and aspirin. These medications have an impact on the regulation of neurohormonal response. Therefore, interaction between them and biomarkers and mortality may have been ignored.
In conclusion, elevated low hs-cTnT levels were more common in elderly inpatients without acute cardiovascular events and showed better predictive performance for all-cause mortality after discharge than levels of NT-proBNP. The combination of the two cardiac biomarkers did not render a better predictive value for all-cause mortality than hs-cTnT alone. Screening strategies based on hs-cTnT levels may help to improve risk stratification, allowing the identification of patients with a higher risk of mortality.
Disclosure
The authors report no conflicts of interest in this work.
References
Lindholm D, Lindbäck J, Armstrong PW, et al. Biomarker-based risk model to predict cardiovascular mortality in patients with stable coronary disease. J Am Coll Cardiol. 2017;70(7):813–826. | ||
de Lemos JA, Drazner MH, Omland T, et al. Association of troponin T detected with a highly sensitive assay and cardiac structure and mortality risk in the general population. JAMA. 2010;304(22):2503–2512. | ||
Saunders JT, Nambi V, de Lemos JA, et al. Cardiac troponin T measured by a highly sensitive assay predicts coronary heart disease, heart failure, and mortality in the Atherosclerosis Risk in Communities Study. Circulation. 2011;123(13):1367–1376. | ||
Defilippi CR, Christenson RH, Gottdiener JS, Kop WJ, Seliger SL. Dynamic cardiovascular risk assessment in elderly people. The role of repeated N-terminal pro-B-type natriuretic peptide testing. J Am Coll Cardiol. 2010;55(5):441–450. | ||
Chow SL, Maisel AS, Anand I, et al. Role of biomarkers for the prevention, assessment, and management of heart failure: a scientific statement from the American Heart Association. Circulation. 2017;135(22):e1054–e10912017-05-30. | ||
Sarzani R, Spannella F, Giulietti F, et al. NT-proBNP and its correlation with in-hospital mortality in the very elderly without an admission diagnosis of heart failure. PLoS One. 2016;11(4):e0153759. | ||
Gore MO, Seliger SL, Defilippi CR, et al. Age- and sex-dependent upper reference limits for the high-sensitivity cardiac troponin T assay. J Am Coll Cardiol. 2014;63(14):1441–1448. | ||
Chew DP, Briffa TG, Alhammad NJ, et al. High sensitivity-troponin elevation secondary to non-coronary diagnoses and death and recurrent myocardial infarction: an examination against criteria of causality. Eur Heart J Acute Cardiovasc Care. 2015;4(5):419–428. | ||
Daniels LB, Clopton P, Defilippi CR, et al. Serial measurement of N-terminal pro-B-type natriuretic peptide and cardiac troponin T for cardiovascular disease risk assessment in the Multi-Ethnic Study of Atherosclerosis (MESA). Am Heart J. 2015;170(6):1170–1183. | ||
Thygesen K, Alpert JS, Jaffe AS. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2018;00:1–33. | ||
Wu W, Li DX, Wang Q, Xu Y, Cui YJ. Relationship between high-sensitivity cardiac troponin T and the prognosis of elderly inpatients with non-acute coronary syndromes. Clin Interv Aging. 2018;13:1091–1098. | ||
Mckie PM, Cataliotti A, Sangaralingham SJ, et al. Predictive utility of atrial, N-terminal pro-atrial, and N-terminal pro-B-type natriuretic peptides for mortality and cardiovascular events in the general community: a 9-year follow-up study. Mayo Clin Proc. 2011;86(12):1154–1160. | ||
Oudejans I, Mosterd A, Bloemen JA, et al. Clinical evaluation of geriatric outpatients with suspected heart failure: value of symptoms, signs, and additional tests. Eur J Heart Fail. 2011;13(5):518–527. | ||
Morrow DA. Cardiovascular risk prediction in patients with stable and unstable coronary heart disease. Circulation. 2010;121(24):2681–2691. | ||
Vaes B, Delgado V, Bax J, Degryse J, Westendorp RG, Gussekloo J. Diagnostic accuracy of plasma NT-proBNP levels for excluding cardiac abnormalities in the very elderly. BMC Geriatr. 2010;10(10):85. | ||
Nybo M, Benn M, Mogelvang R, et al. Impact of hemoglobin on plasma pro-B-type natriuretic peptide concentrations in the general population. Clin Chem. 2007;53(11):1921–1927. | ||
Vaes B, de Ruijter W, Degryse J, Westendorp RG, Gussekloo J. Clinical relevance of a raised plasma N-terminal pro-brain natriuretic peptide level in a population-based cohort of nonagenarians. J Am Geriatr Soc. 2009;57(5):823–829. | ||
Bansal N, Katz R, Dalrymple L, et al. NT-proBNP and troponin T and risk of rapid kidney function decline and incident CKD in elderly adults. Clin J Am Soc Nephrol. 2015;10(2):205–2142015-02-06. | ||
Baron JM, Lewandrowski EL, Januzzi JL, Bajwa EK, Thompson BT, Lewandrowski KB. Measurement of high-sensitivity troponin T in noncardiac medical intensive care unit patients. Correlation to mortality and length of stay. Am J Clin Pathol. 2014;141(4):488–493. | ||
Iversen K, Køber L, Gøtze JP, et al. Troponin T is a strong marker of mortality in hospitalized patients. Int J Cardiol. 2013;168(2):818–824. | ||
Nakamura Y, Yoshihisa A, Takiguchi M, et al. High-sensitivity cardiac troponin T predicts non-cardiac mortality in heart failure. Circ J. 2014;78(4):890–895. | ||
Hitsumoto T. Factors associated with high-sensitivity cardiac Troponin T in patients with type 2 diabetes mellitus. J Nippon Med Sch. 2015;82(6):274–280. | ||
Neukamm AM, Høiseth AD, Hagve TA, Søyseth V, Omland T. High-sensitivity cardiac troponin T levels are increased in stable COPD. Heart. 2013;99(6):382–387. | ||
Wassef AW, Hiebert B, Saeed MF, Tam JW. Novel high-sensitivity troponin assay requires higher cut-off value to separate acute myocardial infarction from non-acute myocardial infarction in a high-risk population. Can J Physiol Pharmacol. 2015;93(10):873–877. | ||
Kim Y, Matsushita K, Sang Y, et al. Association of high-sensitivity cardiac troponin T and natriuretic peptide with incident ESRD: the Atherosclerosis Risk in Communities (ARIC) study. Am J Kidney Dis. 2015;65(4):550–558. | ||
Oh HJ, Lee MJ, Kwon YE, et al. Which biomarker is the best for predicting mortality in incident peritoneal dialysis patients: NT-ProBNP, cardiac TnT, or hsCRP?: a prospective observational study. Medicine. 2015;94(44):e1636. | ||
Satyan S, Light RP, Agarwal R. Relationships of N-terminal pro-B-natriuretic peptide and cardiac troponin T to left ventricular mass and function and mortality in asymptomatic hemodialysis patients. Am J Kidney Dis. 2007;50(6):1009–1019. | ||
Apple FS, Murakami MM, Pearce LA, Herzog CA. Multi-biomarker risk stratification of N-terminal pro-B-type natriuretic peptide, high-sensitivity C-reactive protein, and cardiac troponin T and I in end-stage renal disease for all-cause death. Clin Chem. 2004;50(12):2279–2285. | ||
Oh HJ, Lee MJ, Lee HS, et al. NT-proBNP: is it a more significant risk factor for mortality than troponin T in incident hemodialysis patients? Medicine. 2014;93(27):e241. | ||
Khan NA, Hemmelgarn BR, Tonelli M, Thompson CR, Levin A. Prognostic value of troponin T and I among asymptomatic patients with end-stage renal disease: a meta-analysis. Circulation. 2005;112(20):3088–3096. | ||
Iliou MC, Fumeron C, Benoit MO, et al. Prognostic value of cardiac markers in ESRD: Chronic Hemodialysis and New Cardiac Markers Evaluation (CHANCE) study. Am J Kidney Dis. 2003;42(3):513–523. | ||
Madsen LH, Ladefoged S, Corell P, Schou M, Hildebrandt PR, Atar D. N-terminal pro brain natriuretic peptide predicts mortality in patients with end-stage renal disease in hemodialysis. Kidney Int. 2007;71(6):548–554. | ||
Rubin J, Matsushita K, Ballantyne CM, Hoogeveen R, Coresh J, Selvin E. Chronic hyperglycemia and subclinical myocardial injury. J Am Coll Cardiol. 2012;59(5):484–489. | ||
Dadu RT, Fornage M, Virani SS, et al. Cardiovascular biomarkers and subclinical brain disease in the atherosclerosis risk in communities study. Stroke. 2013;44(7):1803–1808. | ||
Defilippi C, Seliger SL, Kelley W, et al. Interpreting cardiac troponin results from high-sensitivity assays in chronic kidney disease without acute coronary syndrome. Clin Chem. 2012;58(9):1342–1351. | ||
Otsuka T, Kawada T, Ibuki C, Seino Y. Association between high-sensitivity cardiac troponin T levels and the predicted cardiovascular risk in middle-aged men without overt cardiovascular disease. Am Heart J. 2010;159(6):972–978. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.