Back to Journals » Drug Design, Development and Therapy » Volume 14
Comparison of Pharmacokinetics of Aprepitant in Healthy Chinese and Caucasian Subjects
Authors Yang MJ, Xu HR, Li H, Chen WL, Yuan F, Li XN
Received 30 December 2019
Accepted for publication 7 March 2020
Published 24 March 2020 Volume 2020:14 Pages 1219—1226
DOI https://doi.org/10.2147/DDDT.S243924
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Anastasios Lymperopoulos
Meng-Jie Yang, Hong-Rong Xu, Hui Li, Wei-Li Chen, Fei Yuan, Xue-Ning Li
Department of Clinical Pharmacology, Zhongshan Hospital, Fudan University, Shanghai, People’s Republic of China
Correspondence: Xue-Ning Li
Department of Clinical Pharmacology, Zhongshan Hospital, Fudan University, 180 Fenglin Road, Shanghai 200032, People’s Republic of China
Tel +86 21 31587861
Fax +86 21 64437963
Email [email protected]
Purpose: Aprepitant is used to prevent nausea and vomiting associated with moderately and highly emetogenic chemotherapy. In this open-label, 2-period study, the safety, tolerability, and pharmacokinetics (PK) of aprepitant (EMEND®) were evaluated in healthy Chinese and Caucasian subjects.
Patients and Methods: Twelve Chinese and 12 Caucasian subjects were to receive a 125 mg single-dose of aprepitant during period 1; subsequently, after 15 days washout, only Chinese subjects were to receive the 3-day regimen in period 2. In each period, serial blood samples were collected and analyzed by a validated liquid chromatographic and mass spectrometric method to characterize aprepitant PK across both groups.
Results: In both Chinese and Caucasian subjects, there were no serious adverse events. AUC0-∞, Cmax, Tmax, and t1/2 were largely comparable between the two ethnicities. Comparing the result of period 1 in Chinese and Caucasian subjects, the geometric least-squares mean maximum plasma concentrations (Cmax) were 1482 ng/mL and 1435 ng/mL, and the area under the concentration–time curve (AUC0-∞) 34,035 hr·ng/mL and 34,188 hr·ng/mL. In period 2, the geometric mean AUC0– 24 on Day 1 and Day 3 were 19,446 hr·ng/mL and 27,843 hr·ng/mL, and the geometric mean Cmax on Day 1 and Day 3 were 1423 ng/mL and 1757 ng/mL, respectively.
Conclusion: Aprepitant is generally safe and well tolerated in healthy Chinese and Caucasian subjects. Aprepitant PK is comparable between Chinese and Caucasian subjects following single-dose administration. The PK following a clinical 3-day regimen on healthy Chinese subjects has been characterized.
Keywords: pharmacokinetics, aprepitant, chemotherapy-induced nausea and vomiting, ethnicity, healthy subjects
Introduction
Chemotherapy-induced nausea and vomiting (CINV) is one of the most distressing concerns that reduce cancer patients’ quality of life and prevent them from receiving chemotherapy.1–4 The pathophysiology of CINV is a complex multifactorial process that involves communication between several neurotransmitters and receptors in the central nervous system and gastrointestinal tract.3 Increased risk of CINV may be attributable to the type of chemotherapy administered, and specific patient characteristics such as young patients, female patients, those with comorbid depression and anxiety, cancer-related fatigue, or previous history of nausea and vomiting are more likely to experience CINV.5–8 There have been several important advances in the management of CINV in recent years, particularly with the use of various antiemetic agents, including 5-HT3 serotonin receptor antagonist and tachykinin Neurokinin-1 receptor antagonists (NK-1 RAs).6,9,10 NK-1 RAs have high affinity and selectivity in the prophylaxis of emesis.11–13
Aprepitant is a potent and selective substance P (NK1-receptor) antagonist that is recommended in combination with other antiemetic agents for the prevention of acute and delayed nausea and vomiting associated with highly emetogenic and moderately emetogenic cancer chemotherapy (HEC and MEC, respectively).12,14-16
The pharmacokinetics (PK) of aprepitant have been well characterized in the non-Chinese population, and several multi-center studies have shown the efficacy and tolerability of aprepitant in Chinese subjects.17–23 The objective of this study was to investigate the PK and safety of aprepitant in Chinese subjects and compare the single-dose PK between Chinese and Caucasian subjects.
Materials and Methods
Ethical Considerations
The protocol (PN802) and the informed consent form were approved by the Ethics Committee of Zhongshan Hospital Fudan University, Shanghai, China, and registered on http://www.chinadrugtrials.org.cn (CTR20140116). Written informed consent was obtained from all subjects before any study-specific procedure. The study was conducted in accordance with the Good Clinical Practice and the Declaration of Helsinki.
Subjects
Subjects were male or female of Chinese or Caucasian descent residing in China and between 18 and 45 (inclusive) years of age with a Body Mass Index (BMI) range of ≥19 and ≤28 kg/m2 (inclusive) at the screening visit. Twelve Chinese subjects and 12 Caucasian subjects were in good general health, as confirmed by medical history, physical examination, vital signs, electrocardiogram (ECG), and clinical laboratory test. Chinese or Caucasian descent was defined as follows: Chinese descent: both biological parents and all four biological grandparents born in China and of Chinese descent. Caucasian subjects: both biological parents and all four biological grandparents born in Europe, Australia, or North America and of Caucasian descent.
Subjects were excluded from the study if they met any of the following criteria: pregnant or currently breastfeeding; mentally or legally incapacitated, significant emotional problems at the time of study, a history of major psychiatric disorders, clinically significant disease history, cardiac or vascular disorder, asthma or other pulmonary disease, major gastrointestinal abnormalities/peptic ulceration, hepatic or hepatobiliary, neurologic, endocrine, hematologic, renal disease, major genitourinary disease, estimated creatinine clearance of ≤80 mL/min based on the Cockcroft-Gault equation, history of any illness or any condition that, in the opinion of the investigator, may interfere with optimal participation in the study, confound the results of the study, or pose additional risk in administering aprepitant.
Study Design
This was an open-label, 2-period study in 24 healthy subjects (12 Chinese and 12 Caucasian). All subjects were to receive a 125 mg single-dose of aprepitant during period 1. During period 2, the same 12 Chinese subjects were to receive a 3-day regimen (125 mg dose of aprepitant on Day 1, 80 mg dose on Day 2 and Day 3). Two treatment periods were separated by 15 days washout period.
All doses of the study drug were administered in the fasted (following an at least 8 hr overnight fast) state. Each oral dose was administered with approximately 240 mL of room-temperature water.
Sample Collection and Plasma Drug Assays
In treatment period 1 (all subjects), 5 mL blood was collected per time points, as follows: pre-dose (0 hr), 0.5, 1, 2, 3, 4, 6, 8, 12, 24, 48, 72, and 96 hrs.
In treatment period 2 (only Chinese subjects), 5 mL blood was collected per time points, as follows: pre-dose (0 hr) and the following time points after the Day 1 dose: 0.5, 1, 2, 3, 4, 6, 8, 12, 24, 48, 48.5, 49, 50, 51, 52, 54, 56, 60, 72, 96, 120, and 144 hrs.
After collection, blood samples were centrifuged at approximately 3500rpm for 15 mins at 4°C, and the plasma was then separated into two aliquots of 1.0 mL, which were stored at −70°C freezer within 45 mins of collection until shipped to a centralized laboratory. Plasma aprepitant concentrations were determined by WuXi AppTec Co., Ltd (Shanghai, China) using a validated method employing liquid-liquid extraction followed by high-performance liquid chromatography (HPLC) with mass spectrometric (MS) detection. The lower limit of quantitation (LLOQ) for the aprepitant assay was 10.0 ng/mL, with a calibration range of 10.0 to 5000 ng/mL.
Pharmacokinetic Assessments
Pharmacokinetic parameters of aprepitant were calculated using Phoenix® WinNonlin® 6.2. The actual blood collection times were used in the PK analysis. The maximum plasma concentrations (Cmax) and time to maximum plasma concentration (Tmax) were obtained directly from the observed values. The elimination rate constant (ke) was determined by linear regression of the logarithm of the plasma concentrations over time. Terminal half-life (t1/2) was calculated as 0.693/ke. The area under the concentration–time curve from zero to infinity (AUC0-∞) for aprepitant was calculated as AUC0-last + Cest, last/λz, where Cest, last is the estimated concentration at the time of the last quantifiable concentration. For each subject, λz, the apparent first-order terminal elimination rate constant, was calculated by regression of the terminal log-linear portion of the plasma concentration-time profile.
Safety Assessments
The safety and tolerability of aprepitant were assessed with adverse events (AEs), laboratory safety tests, ECGs, vital signs, and physical examinations. Throughout the study, the subjects were also asked to self-report AEs to any investigator. Any serious AEs, or follow up to a serious AE, including death due to any cause to any subject from the time the consent is signed through 15 days following cessation of the treatment, were reported.
Statistical Analyses
In period 1 (i.e., single-dose period), the AUC0-∞ and Cmax values were natural log-transformed prior to analysis. The AUC0-∞ and Cmax were analyzed with a one-way ANOVA model with group effect (Chinese vs Caucasian) as the main factor. Back-transformed summary statistics and inferential results were reported for pharmacokinetic parameters on the normal scale. The 90% confidence intervals (CIs), based on the t-distribution, were generated from the one-way ANOVA model for the geometric mean ratio (GMR, [Chinese/Caucasian]) for AUC0-∞ and Cmax of aprepitant. In period 2 (i.e., multiple-dose period), descriptive statistics (arithmetic mean, standard deviation, geometric mean, geometric percent CV, 95% CIs) were provided for each PK parameter of aprepitant [e.g., AUC0–24hr, Cmax, Tmax (on both Day 1 and Day 3) and apparent terminal t1/2 (on Day 3 only)] following aprepitant 125 mg on Day 1, and 80 mg on Day 2 and Day 3 (period 2), respectively.
Safety was evaluated following administration of aprepitant in healthy Chinese and Caucasian subjects by clinical assessment of AEs and other safety parameters. All AES were coded according to the latest available version of the MedDRA. Safety statistical analyses were performed by PAREXEL Early Phase Biostatistics using SAS® (SAS Institute Inc., Cary, North Carolina, USA), Version 9.3.
Results
Study Subjects
In this study, a total of 24 subjects were enrolled, and all completed the study. The summary demographic information for the 24 subjects entered into the study is provided in Table 1. The age, body weight, height, and body mass index (BMI) were approximately matched and comparable between these two ethnic groups. The average age, body weight, height, and BMI were 26 years, 59.9 kg, 164.8 cm, and 22.1 kg/m2 in Chinese subjects, respectively; 25.1 years, 64.4kg, 171.7cm, and 21.7 kg/m2 in Caucasian subjects, respectively.
 |
Table 1 Summary of Demographics and Baseline Characteristics |
Pharmacokinetics
Single-Dose Pharmacokinetics
Following a single-dose administration of 125 mg aprepitant, the drug was absorbed with a median Tmax of 4 hrs and eliminated with the bi-exponential decline with t1/2 of approximately 12 hrs. The mean plasma concentration-time profiles in healthy Chinese and Caucasian subjects are presented in Figure 1 and were comparable and largely overlapped.
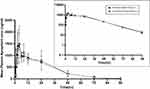 |
Figure 1 Comparison of aprepitant exposures in healthy adult Chinese and Caucasian subjects following a single oral dose of 125 mg of aprepitant in normal and semi-log scale. |
Table 2 presents the results of the statistical analysis of the PK data for Chinese and Caucasian subjects in the single-dose period (Period 1). For the comparison of PK between Chinese and Caucasians subjects, the GMR (Chinese/Caucasian) of AUC0-∞ and Cmax were used. The GMR (Chinese/Caucasian) and corresponding 90% CI for AUC0-∞ and Cmax were determined as 1.00 (0.78, 1.28) and 1.03 (0.79, 1.35), respectively. The variability (geometric CV%) associated with AUC0-∞ and Cmax was moderate (35.6% to 38.3%). The geometric mean t1/2of 125 mg aprepitant was comparable between Chinese and Caucasian subjects; Cmax was reached at a median of 4.00 hrs for both ethnic groups. All four primary PK endpoints (i.e., AUC0-∞, Cmax, Tmax and t1/2) were largely comparable between the two ethnicities.
Multiple-Dose Pharmacokinetics
The mean profiles of period 2 in healthy Chinese subjects after 3-day regimen are displayed in Figure 2. Absorption of aprepitant was relatively rapid, with peak plasma concentrations attained 4 hrs after drug administration. In addition, aprepitant plasma concentrations were well maintained. The descending phase represented to be biphasic, which showed a relatively steep initial descending phase followed with a gradual terminal phase. Table 3 presents the descriptive statistical summary of the aprepitant PK parameters after multi-dose in healthy Chinese subjects. The median of Tmax was 4.00 hrs on both Day 1 and Day 3. Geometric mean AUC0–24hr on Day 1 and Day 3 were 19,446 hr·ng/mL and 27,843 hr·ng/mL, respectively. The geometric mean Cmax on Day 1 and Day 3 were 1423 ng/mL and 1757 ng/mL accordingly. The apparent terminal t1/2 was 11.26 hrs following multiple-dose administration. The AUC0–24hr and Cmax on Day 3 were higher than that of Day 1, suggested slight accumulation in Chinese after multiple doses administered.
 |
Figure 2 Aprepitant exposures in healthy adult Chinese subjects on day 1 and day 3 following a 3-day regimen of 125 mg aprepitant on day 1 and 80 mg on days 2 and 3. |
Safety
Among the 24 subjects in this study, 12 subjects experienced 18 mild or moderate AEs. All these AEs were transient in nature, and no subject withdrew because of an AE; no serious AEs occurred in this study. All AEs were judged to be drug-related by the investigator. The incidence of AEs was comparable between Chinese (5/12) and Caucasian subjects (7/12) in Table 4. Therefore, single-dose aprepitant is generally safe and well tolerated in healthy Chinese and Caucasian subjects, in addition, multiple doses in healthy Chinese as well.
 |
Table 4 Subjects with Drug-Related Adverse Events (Incidence > 0% in One or More Treatment Groups) |
Discussion
This was the first aprepitant PK study among subjects of Chinese and Caucasian ethnicity, which was conducted to support comparison across these ethnic groups. Following administration of single dose (125 mg) aprepitant in healthy Chinese subjects and healthy Caucasian subjects under fasted condition, all four primary PK endpoints (i.e., AUC0-∞, Cmax, Tmax and t1/2) were comparable between the two ethnicities. Aprepitant exposure after a single dose in healthy Chinese subjects in this trial was generally comparable to non-Chinese subjects observed from a previous study;17 however after clinical 3-day regimen administered, the previous non-Chinese subjects’ data of AUC0–24h, Cmax and t1/2 on Day 3 were lower than Chinese subjects on Day 3. The PK profile in Chinese subjects following the 3-day regimen shows that the exposure on Day 3 is slightly higher than that of Day 1, suggesting slight accumulation, which was not observed in the previous study. The reason for the differences is not clear and not clinically meaningful. A population PK study24 shows that body weight, age, blood urea nitrogen, and alanine aminotransferase may have an effect on the clearance of aprepitant. Therefore, we designed a well-controlled study, which reduced those influences and eliminated the bias of cross-study comparison.
Aprepitant is a low-extraction drug cleared by hepatic metabolism with minimal renal excretion of the parent drug, and the Cytochrome P450 3A4 enzyme plays a major role in the metabolism of aprepitant.18,25,26 Therefore, it is consistent with the data of CYP3A4, which is relatively non-polymorphic, and hence significant differences between Chinese and Caucasian subjects would not be expected and were not apparent in our study.
Conclusion
In summary, the PK profile in healthy Chinese subjects and the effect of ethnicity on the pharmacokinetics of aprepitant were studied. Moreover, the present study confirmed aprepitant was well tolerated in both Chinese and Caucasian subjects.
Data Sharing Statement
- We do intend to share individual deidentified participant data;
- Individual participant data that underlie the results reported in this article could be shared after deidentification (text, tables, figures, and appendices);
- According to Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA’s data sharing policy, including restrictions, the data is available at http://engagezone.msd.com/ds_documentation.php.
- There will be no other study-related documents shared;
- The data will be available beginning 9 months and ending 36 months following article publication.
Acknowledgments
The authors wish to thank the sponsor (Merck Sharp & Dohme Corp.) for designing the study and reviewing the manuscript, PAREXEL for performing safety statistical analyses, Rebecca Wrishko, Anne Chain, Bhavna Kantesaria, and Karyn Davis, Kristen Lewis (Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA) and Ying Song and Yanqiao Zang (of MSD R&D [China] Ltd., Beijing, China) for Editorial assistance. The authors also would like to thank all of the subjects and medical staff for their participation.
Disclosure
Funding for this research was provided by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA. The concept of the project was originated and the protocol was reviewed before any funding was issued. Funds received paid for medications administered, research personnel, pharmacy administrative fees, IRB fees, and statistical analysis. The manuscript was reviewed by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA before submission. The authors report no other conflicts of interest in this work.
References
1. Jordan K, Sippel C, Schmoll HJ. Guidelines for antiemetic treatment of chemotherapy-induced nausea and vomiting: past, present, and future recommendations. Oncologist. 2007;12(9):1143–1150. doi:10.1634/theoncologist.12-9-1143
2. Roila EBF. Impact of nausea and vomiting on quality of life in cancer patients during chemotherapy. Health Qual Life Outcomes. 2003;1(1):46. doi:10.1186/1477-7525-1-46
3. Aapro M. CINV: still troubling patients after all these years. Support Care Cancer. 2018;26(Suppl 1):5–9. doi:10.1007/s00520-018-4131-3
4. Guo L, Peng H, Cai HL, et al. Effect of aprepitant administration on CINV caused by cisplatin multi-day chemotherapy and pharmacokinetics of docetaxel. Cancer Chemother Pharmacol. 2019;83(4):727–734. doi:10.1007/s00280-019-03777-7
5. Hsieh RK, Chan A, Kim HK, et al. Baseline patient characteristics, incidence of CINV, and physician perception of CINV incidence following moderately and highly emetogenic chemotherapy in Asia Pacific countries. Support Care Cancer. 2015;23(1):263–272. doi:10.1007/s00520-014-2373-2
6. Navari RM. Management of chemotherapy-induced nausea and vomiting. Drugs. 2016;73:249–262.
7. Hilarius DL, Kloeg PH, Van der Wall E, Gundy CM, Aaronson NK. Chemotherapy-induced nausea and vomiting in daily clinical practice: a community hospital-based study. Support Care Cancer. 2012;20(1):107–117. doi:10.1007/s00520-010-1073-9
8. Molassiotis A, Aapro M, Dicato M, et al. Evaluation of risk factors predicting chemotherapy-related nausea and vomiting: results from a European prospective observational study. J Pain Symptom Manage. 2014;47(5):839–848.e834. doi:10.1016/j.jpainsymman.2013.06.012
9. Jordan K, Gralla R, Jahn F, Molassiotis A. International antiemetic guidelines on chemotherapy induced nausea and vomiting (CINV): content and implementation in daily routine practice. Eur J Pharmacol. 2014;722:197–202. doi:10.1016/j.ejphar.2013.09.073
10. Iihara H, Fujii H, Yoshimi C, et al. Control of chemotherapy-induced nausea in patients receiving outpatient cancer chemotherapy. Int J Clin Oncol. 2016;21(2):409–418. doi:10.1007/s10147-015-0908-2
11. Rapoport B, Smit T. Clinical pharmacology of neurokinin-1 receptor antagonists for the treatment of nausea and vomiting associated with chemotherapy. Expert Opin Drug Saf. 2017;16(6):697. doi:10.1080/14740338.2017.1325868
12. Aapro M, Carides A, Rapoport BL, Schmoll HJ, Zhang L, Warr D. Aprepitant and fosaprepitant: a 10-year review of efficacy and safety. Oncologist. 2015;20(4):450–458. doi:10.1634/theoncologist.2014-0229
13. Milnes V, Gonzalez A, Amos V. Aprepitant: a new modality for the prevention of postoperative nausea and vomiting: an evidence-based review. J PeriAnesth Nurs. 2015;30(5):406–417. doi:10.1016/j.jopan.2014.11.013
14. Campos D, Pereira JR, Reinhardt RR, et al. Prevention of cisplatin-induced emesis by the oral neurokinin-1 antagonist, MK-869, in combination with granisetron and dexamethasone or with dexamethasone alone. J Clin Oncol. 2001;19(6):1759–1767. doi:10.1200/JCO.2001.19.6.1759
15. Simon VB, Lichinitser MR, Navari RM, et al. Prevention of cisplatin-induced acute and delayed emesis by the selective neurokinin-1 antagonists, L-758,298 and MK-869. Cancer Chemother Pharmacol. 2002;94(11):3032–3041.
16. Aapro M, Molassiotis A, Dicato M, et al. The effect of guideline-consistent antiemetic therapy on chemotherapy-induced nausea and vomiting (CINV): the Pan European Emesis Registry (PEER). Ann Oncol. 2012;23(8):1986–1992. doi:10.1093/annonc/mds021
17. Majumdar AK, Howard L, Goldberg MR, et al. Pharmacokinetics of aprepitant after single and multiple oral doses in healthy volunteers. J Clin Pharmacol. 2006;46(3):291–300. doi:10.1177/0091270005283467
18. Bubalo JS, Cherala G, McCune JS, Munar MY, Tse S, Maziarz R. Aprepitant pharmacokinetics and assessing the impact of aprepitant on cyclophosphamide metabolism in cancer patients undergoing hematopoietic stem cell transplantation. J Clin Pharmacol. 2012;52(4):586–594. doi:10.1177/0091270011398243
19. Salman FT, DiCristina C, Chain A, Afzal AS. Pharmacokinetics and pharmacodynamics of aprepitant for the prevention of postoperative nausea and vomiting in pediatric subjects. J Pediatr Surg. 2018;54:1384–1390.
20. Yeo W, Mo FKF, Suen JJS, et al. A randomized study of aprepitant, ondansetron and dexamethasone for chemotherapy-induced nausea and vomiting in Chinese breast cancer patients receiving moderately emetogenic chemotherapy. Breast Cancer Res Treat. 2008;113(3):529–535. doi:10.1007/s10549-008-9957-9
21. Hu Z, Cheng Y, Zhang H, et al. Aprepitant triple therapy for the prevention of chemotherapy-induced nausea and vomiting following high-dose cisplatin in Chinese patients: a randomized, double-blind, placebo-controlled Phase III trial. Support Care Cancer. 2014;22(4):979–987. doi:10.1007/s00520-013-2043-9
22. Zhang L, Lu S, Feng J, et al. A randomized phase III study evaluating the efficacy of single-dose NEPA, a fixed antiemetic combination of netupitant and palonosetron, versus an aprepitant regimen for prevention of chemotherapy-induced nausea and vomiting (CINV) in patients receiving highly emetogenic chemotherapy (HEC). Ann Oncol. 2018;29(2):452–458. doi:10.1093/annonc/mdx698
23. Chen LK, Cheng Y, Zhang HY, et al. Efficacy of aprepitant in preventing high-dose cisplatin-induced nausea and vomiting in Chinese patients with lung cancer. Chin J New Drugs Clin Remedies. 2015;32(10):757–763. doi:10.14109/j.cnki.xyylc.2015.10.006
24. Nakade S, Ohno T, Kitagawa J, et al. Population pharmacokinetics of aprepitant and dexamethasone in the prevention of chemotherapy-induced nausea and vomiting. Cancer Chemother Pharmacol. 2008;63(1):75–83. doi:10.1007/s00280-008-0713-y
25. Massaro AM, Lenz KL. Aprepitant: a novel antiemetic for chemotherapy-induced nausea and vomiting. Ann Pharmacother. 2005;39(1):77–85. doi:10.1345/aph.1E242
26. Sanchez RI, Wang RD, Bakhtiar R, et al. Cytochrome P450 3A4 is the major enzyme involved in the metabolism of the substance P receptor antagonist aprepitant. Drug Metabo Dispos. 2004;32(11):1287–1292. doi:10.1124/dmd.104.000216
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


