Back to Journals » Journal of Pain Research » Volume 14
Comparison of Percutaneous Transforaminal Endoscopic Decompression and Transforaminal Lumbar Interbody Fusion in the Treatment of Single-Level Lumbar Disc Herniation with Modic Type I Changes
Authors Li P, Yang F , Tong Y, Chen Y, Song Y
Received 10 September 2021
Accepted for publication 1 November 2021
Published 9 November 2021 Volume 2021:14 Pages 3511—3517
DOI https://doi.org/10.2147/JPR.S338342
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Krishnan Chakravarthy
Pengfei Li, Fengkai Yang, Yuexin Tong, Ying Chen, Youxin Song
Department of Orthopedic, Affiliated Hospital of Chengde Medical University, Chengde, Hebei, 067000, People’s Republic of China
Correspondence: Youxin Song
Department of Orthopedic, Affiliated Hospital of Chengde Medical University, No. 36 Nanyingzi St, Chengde, Hebei, 067000, People’s Republic of China
Email [email protected]
Background: Modic changes (MC) are generally considered to be related to degenerative disc disease, and there is no uniform standard for surgical methods for lumbar disc herniation (LDH) accompanied by Modic type I changes (MC I). The purpose of this study was to observe the clinical results of percutaneous transforaminal endoscopic decompression (PTED) and transforaminal lumbar interbody fusion (TLIF) for treatment of LDH accompanied by MC I.
Methods: Of the 53 consecutive patients included, 29 underwent PTED and 24 underwent TLIF. All patients were followed up for at least 24 months. Preoperative demographic characteristics, perioperative outcomes, and clinical outcomes were recorded. Visual analog scale (VAS) scores, Oswestry disability index (ODI) scores, and modified Macnab criteria were used to assess clinical results.
Results: The mean age was 53.7± 9.2 years in the PTED group and 53.6± 9.6 years in the TLIF group. The scores of VAS legs, VAS back and ODI in the two groups after operation were significantly improved compared with those before operation (P< 0.05). Notably, the VAS back pain score and ODI in the PTED group showed an increasing trend with time. And the VAS back pain scores and ODI of the two groups were statistically different at 1 year and 2 years postoperatively (P< 0.05). In addition, compared with the TLIF group, the PTED group showed less operation time, blood loss, and postoperative hospital stay (P< 0.05). At the final follow-up, the excellent rates were 91.7% and 86.2% in the fusion and PTED groups, respectively.
Conclusion: Both PTED and TLIF procedures significantly improved the clinical symptoms of single-level LDH patients with MC I. Compared with TLIF, MC I may affect the improvement of low back pain and functional status after PTED.
Keywords: PTED, fusion, Modic change, lumbar disc herniation, back pain
Introduction
Modic changes (MC) are changes in the signal intensity of the vertebral endplates and adjacent bone marrow on MRI. The earliest systematic classification was performed by Modic et al1,2 Based on the differences in MRI signals, they were classified as type I (MC I), type II (MC II), and type III (MC III). Compared to the adjacent normal bone marrow, MC I represents a bone marrow inflammatory response, MC II represents a bone marrow fatty infiltration, and MC III represents a sclerotic change of the bone marrow. These three types of MC may be different stages of the degenerative process of the vertebral body.3 Although the etiology of MC is still unclear,4 microfracture of the endplate is thought to be a key link in MC formation.5 As the cartilage endplate of the vertebral body changes, the herniated disc associated with degenerative disc disease will also change.2 Among the different MC types, MC I is often considered to have a high correlation with clinical symptoms.3,6,7 Pathology shows that the bone-disc junction in MC I is filled with vascularized granulation tissue, which is considered a sign of inflammation.4 This may be a source of specific low back pain in patients with MC I. Patients with LDH usually choose lumbar discectomy if conservative treatment fails. However, there is still controversy regarding the choice of discectomy or fusion surgery for patients whose MRI signal at the corresponding level shows MC I. Because different surgical procedures may affect the clinical outcome, especially low back pain and recurrence.8–10
It is well known that transforaminal lumbar interbody fusion (TLIF) has become a popular and well-established technique for the treatment of degenerative lumbar spine disease. Not stopping at the results of traditional surgery, the most important trend in lumbar discectomy has been to minimize the stripping of soft tissue.11 In recent years, with the development of minimally invasive spine technology and equipment, percutaneous transforaminal endoscopic decompression (PTED) surgery provides a less traumatic approach to solving lumbar disc herniation (LDH). PTED has become an effective alternative to traditional open discectomy due to its advantages of minimal trauma, high accuracy, and rapid recovery. Although PTED minimizes damage to bone and soft tissue, its efficacy in patients with LDH with MC I has not been thoroughly described. The purpose of this study was to observe the clinical outcomes of PTED and TLIF in the treatment of single-level LDH with MC I.
Methods and Materials
Participants
From June 2017 to June 2019, a total of 53 patients were retrospectively included. All patients provided written consent. Our hospital institutional review board approved the study. All procedures were performed by the same surgical team. The inclusion criteria were as follows: (1) Low back pain with radiating pain in the legs; (2) Single-level LDH with MC I; (3) Imaging examination is consistent with clinical symptoms; (4) Conservative treatment is ineffective for more than 3 months. The exclusion criteria were as follows: (1) Combined with other types of MC; (2) Combined with spinal stenosis; (3) Segmental instability on preoperative dynamic radiographs; (4) History of previous lumbar spine surgery; (5) Pathological conditions such as tumor, trauma, and infection. Preoperative demographic characteristics, perioperative conditions, and clinical outcomes were recorded.
Surgical Procedure
PTED group: Local infiltration anesthesia is selected, and the surgical position is lateral. The surgical procedure included three steps: (1) Puncture: the puncture site depends on the patient’s body type. It is usually 1–3 cm above the iliac crest and 8–12 cm horizontally from the midline of the posterior spinous process. The puncture needle points to the intersection of the coronal plane connecting the upper articular process and the horizontal plane of the responsible intervertebral disc. Based on the protruding position of the nucleus pulposus shown by preoperative imaging, under the guidance of the C-arm, the puncture needle reaches the corresponding target area. (2) Foramplasty: The foramina is appropriately formed by a bone drill as needed. (3) Discectomy: After insertion of a working trocar, an endoscope is placed. The protruding nucleus pulposus is removed using a clamp under the protection of a trocar. Then, the nerve root is explored and released. The nerve root was seen to be pulsating freely with the heartbeat and the procedure was completed.
TLIF group: The procedure was completed under general anesthesia. The patient is positioned prone and a posterior median incision is selected. The responsible segmental structures are fully exposed and the pedicle screws are placed with the assistance of a C-arm. Some of the upper and lower articular processes and the vertebral plate were removed, and the dural sac and nerve roots were exposed. After complete decompression of the dural sac and nerve roots, the nucleus pulposus is removed with forceps. The endplate cartilage is then scraped off with a curette. The intervertebral space was flushed and the intervertebral fusion device was placed. Finally, bilateral fixation rods were installed and the pedicle nails were tightened.
Evaluation Indicators
Preoperative demographic characteristics and perioperative outcomes were compared. VAS and ODI scores were used to evaluate pre- and post-operative clinical outcomes. In addition, a modified Macnab criterion was used to assess surgical satisfaction at the final follow-up.
Statistical Assessments
Statistical calculations were performed using the SPSS 26 program (IBM, Armonk, USA). Demographic characteristics, perioperative indicators, and clinical outcomes of the two groups were analyzed using the chi-square test, Student’s t-test, and Mann–Whitney U-test. The significance level was defined as p < 0.05.
Results
Preoperative Demographic Characteristics and Outcomes
The preoperative demographic characteristics are shown in Table 1. The average follow-up time for all patients is at least 24 months. A total of 53 patients participated in this study. The PTED group included 16 males and 13 females, with an average age of 53.6±9.6 years. The TLIF group included 13 males and 11 females, with an average age of 53.7±9.2 years. There were no statistical differences between the two groups in terms of age, gender, body mass index (BMI), proportion of smokers, and level of surgery.
 |
Table 1 Demographic Characteristics of the TLIF Group and PTED Group |
Various Indicators During Perioperative Period
Perioperative indicators are shown in Table 2. The operation time, intraoperative blood loss, and postoperative hospital stay in the TLIF group were longer than those in the PTED group, and the difference between the two groups was statistically significant (P<0.05). However, in terms of major complications, there was no statistically significant difference between the two groups (P>0.05).
 |
Table 2 Operation Characteristics of the Two Groups |
Clinical Results
Statistical improvement in clinical outcomes before and after surgery was assessed by VAS scores and ODI scores (Figure 1). The mean VAS leg pain score at each follow-up time point was similarly improved in both the PTED and TLIF groups compared with the preoperative period (P < 0.05), and there was no statistical difference between the two groups (P > 0.05). The back pain and ODI scores of the TLIF group decreased from 5.3±1.1 and 63.3±7.6 preoperatively to 1.9±0.9 and 22.3±2.5 at 3 months postoperatively, and tended to stabilize at later follow-up time points. The back pain and ODI scores of the PTED group decreased from 5.1±1.0 and 59.4±10.5 before surgery to 2.2±0.7 and 21.6±2.5 at 3 months postoperatively. However, at later follow-up time points, the back pain and ODI scores of the PTED group showed an upward trend. In addition, the back pain and ODI scores of the two groups were statistically different at 1 year and 2 years after surgery (P<0.05).
 |
Figure 1 The clinical outcomes of the TLIF group and the PTED group at different follow-up time points. (A) VAS back pain score. (B) VAS leg pain score. (C) Oswestry Disability Index. |
According to the modified MacNab standard, in the last follow-up, the excellent and good rate of PTED group was 86.2%, and that of TLIF group was 91.7% (Table 3). There was no statistical difference between the two groups (P>0.05).
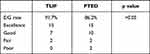 |
Table 3 Modified Mac Nab Criteria |
Discussion
In recent years, MC seems to have become a new topic of interest for spine surgeons. This is because there is increasing evidence that the low back pain of patients with MC is often special.12 Although clinical data from many scholars suggest that MC is closely associated with specific low back pain,13–15 the etiology of MC remains unclear. Previous studies have shown that the pathogenesis of MC has two main aspects. (1) Biomechanical alterations: microfractures of the endplate and subendplate bone occur under spinal loading,4,16 which in turn lead to inflammation of the endplate and adjacent bone marrow;17 (2) Infectious factors: Inflammation of the vertebral endplates is caused by an associated bacterial infection.18,19 After injury, the disc undergoes an inflammatory response and forms new capillaries. This may be a “port” for anaerobic bacteria to enter the disc.19 Among the three types of MC, MC I is often considered to have a high degree of correlation with clinical symptoms. Some scholars have reported that patients with MC I have worse results after discectomy.20,21 It has even been suggested that MC I is related to hyperactivity, which may indicate the need for additional fusion surgery.21 However, some scholars have reported that MC has nothing to do with the clinical outcome of LDH patients.22,23 The most suitable surgical approach for patients with LDH with preoperative MC I remains uncertain. The clinical results obtained by different surgical methods are still controversial.
As we all know, lumbar discectomy is a safe and effective surgical method for the treatment of LDH. In the treatment of cases with MC, previous studies have also reported successful results. Bostelmann et al24 retrospectively analyzed the clinical data of 278 patients undergoing discectomy and they found that different types of MC were not associated with clinical outcomes. Udby et al23 conducted a 2-year follow-up study and found that MC was not associated with quality of life, pain, or patient satisfaction at 2 years after discectomy. The important trend in discectomy has been to reduce soft tissue disruption, and PTED surgery meets this need. As a minimally invasive surgical approach, PTED preserves the posterior ligament complex and other biomechanical structures.25 It has received many promising reports in the treatment of degenerative diseases of the lumbar spine.26,27 In this study, we found that PTED surgery significantly improved leg pain in patients with MC I. However, part of the back pain still remains. Moreover, the VAS back pain and ODI scores of the PTED group were higher than those of the TLIF group at 1 year and 2 years after the operation (P<0.05). To our knowledge, MC is often underestimated as a source of pain. In cases with MC, the use of PTED may be limited. This is because PTED only addresses the nerve compression factors and hardly addresses vertebral endplate inflammation. This may be the cause of residual back pain in patients with LDH accompanied by MC I. This phenomenon has been similarly reported in other studies. Splendiani et al28 evaluated 38 patients with MC I who had non-specific low back pain. They found that MC I was associated with increased pain from the supine position to the standing position. Xu et al29 retrospectively analyzed the clinical results of endoscopic discectomy for LDH patients with MC. They found that postoperative low back pain and functional status of MC patients tended to deteriorate over time, especially MC I.
In addition, regarding the surgical methods of LDH, there is not enough evidence that minimally invasive discectomy is better than traditional surgery.30,31 In particular, the clinical outcome of discectomy alone may be inconclusive when treating patients with LDH with MC. Yao et al32 retrospectively analyzed 116 patients who had recurrence after endoscopic discectomy and found that MC was a potential risk factor for postoperative recurrence. Hao et al33 reported that recurrence following percutaneous endoscopic lumbar discectomy preferentially occurs when MC are present. In this study, during the 2-year follow-up period, we observed that 2 patients in the PTED group had relapses. However, the recurrence rate between the two groups was not statistically different. Interestingly, MC I does not seem to have a bad effect on the fusion surgery. Esposito et al34 studied 60 patients who underwent single-segment lumbar fusion for degenerative disc disease. They found that patients with MC I have a better prognosis. Vital et al35 reported that internal fixation and fusion has achieved good results in the treatment of MC I, and surgery seems to accelerate the dynamic process of MC I. In this study, TLIF surgery appeared to demonstrate better clinical outcomes than PTED surgery for patients with LDH with MC I during the 2-year follow-up period. We may need to fully recognize that PTED is ineffective for healing endplate microfractures. This is because postoperative weight-bearing exercises may prevent the healing of microfractures. In contrast to PTED, fusion surgery is beneficial to the treatment of extensively innervated cartilage endplates. At the same time, internal fixation and fusion can improve the dysfunction caused by the biomechanical changes of the vertebral body.36 This may be the reason why the TLIF group obtained better back pain and ODI scores in this study.
At the last follow-up, the excellent and good rates of TLIF group and PTED group were 91.7% and 86.2%, respectively. The presence of preoperative MC I did not affect the improvement of radicular pain in the two groups. Even so, for patients with single-segment LDH with MC I undergoing PTED surgery, the spine surgeon should explain to the patient that there may be residual back pain and the potential risk of recurrence after surgery.
However, our study also has some limitations. First, the small patient sample size resulted in limited ability to observe clinical outcomes. Second, the learning curve for PTED surgery is high, and performing the procedure by junior physicians may affect the comparison of clinical outcomes. Finally, MC is a dynamic process, and the long-term outcome of patients with MC I requires longer follow-up.
Conclusion
Patients with single-level LDH with MC I can benefit from PTED and TLIF. MC I may affect the degree of improvement in low back pain and functional status after PTED compared to TLIF. But PTED showed less operation time, blood loss, and postoperative hospital stay.
Abbreviations
MC, Modic changes; TLIF, Transforaminal lumbar interbody fusion; PTED, Percutaneous transforaminal endoscopic discectomy; LDH, Lumbar disc herniation; VAS, Visual analog scale; ODI, Oswestry disability index.
Data Sharing Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
This research was approved by the ethics committee of Affiliated Hospital of Chengde Medical University, and the guidelines outlined in the Declaration of Helsinki were followed. Written informed consent were obtained from all the participants.
Consent for Publication
Written informed consent was obtained from all participants.
Acknowledgments
We would like to thank all the participants in the studies.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests.
References
1. Modic MT, Masaryk TJ, Ross JS, Carter JR. Imaging of degenerative disk disease. Radiology. 1988;168(1):177–186. doi:10.1148/radiology.168.1.3289089
2. Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166(1 Pt 1):193–199. doi:10.1148/radiology.166.1.3336678
3. Thompson KJ, Dagher AP, Eckel TS, Clark M, Reinig JW. Modic changes on MR images as studied with provocative diskography: clinical relevance–a retrospective study of 2457 disks. Radiology. 2009;250(3):849–855. doi:10.1148/radiol.2503080474
4. Dudli S, Fields AJ, Samartzis D, Karppinen J, Lotz JC. Pathobiology of Modic changes. Eur Spine J. 2016;25(11):3723–3734. doi:10.1007/s00586-016-4459-7
5. Lan M, Ou Y, Wang C, et al. Patients with Modic type 2 change have a severe radiographic representation in the process of lumbar degeneration: a retrospective imaging study. J Orthop Surg Res. 2019;14(1):298. doi:10.1186/s13018-019-1355-y
6. Järvinen J, Karppinen J, Niinimäki J, et al. Association between changes in lumbar Modic changes and low back symptoms over a two-year period. BMC Musculoskelet Disord. 2015;16:98. doi:10.1186/s12891-015-0540-3
7. Bailly F, Maigne JY, Genevay S, et al. Inflammatory pain pattern and pain with lumbar extension associated with Modic 1 changes on MRI: a prospective case-control study of 120 patients. Eur Spine J. 2014;23(3):493–497. doi:10.1007/s00586-013-3036-6
8. Schistad EI, Espeland A, Rygh LJ, Røe C, Gjerstad J. The association between Modic changes and pain during 1-year follow-up in patients with lumbar radicular pain. Skeletal Radiol. 2014;43(9):1271–1279. doi:10.1007/s00256-014-1928-0
9. Shahmohammadi MR, Behrouzian S. Effect of preoperative Modic change in the outcome of patients with low back pain following posterior spinal fusion or laminectomy. Asian J Neurosurg. 2019;14(2):432–435. doi:10.4103/ajns.AJNS_41_18
10. Sørlie A, Moholdt V, Kvistad KA, et al. Modic type I changes and recovery of back pain after lumbar microdiscectomy. Eur Spine J. 2012;21(11):2252–2258. doi:10.1007/s00586-012-2419-4
11. Truumees E. A history of lumbar disc herniation from Hippocrates to the 1990s. Clin Orthop Relat Res. 2015;473(6):1885–1895. doi:10.1007/s11999-014-3633-7
12. Kjaer P, Korsholm L, Bendix T, Sorensen JS, Leboeuf-Yde C. Modic changes and their associations with clinical findings. Eur Spine J. 2006;15(9):1312–1319. doi:10.1007/s00586-006-0185-x
13. Jensen TS, Karppinen J, Sorensen JS, Niinimäki J, Leboeuf-Yde C. Vertebral endplate signal changes (Modic change): a systematic literature review of prevalence and association with non-specific low back pain. Eur Spine J. 2008;17(11):1407–1422. doi:10.1007/s00586-008-0770-2
14. Xia W, Liu C, Duan S, et al. The influence of spinal-pelvic parameters on the prevalence of endplate Modic changes in degenerative thoracolumbar/lumbar kyphosis patients. PLoS One. 2018;13(5):e0197470. doi:10.1371/journal.pone.0197470
15. Herlin C, Kjaer P, Espeland A, et al. Modic changes-Their associations with low back pain and activity limitation: a systematic literature review and meta-analysis. PLoS One. 2018;13(8):e0200677. doi:10.1371/journal.pone.0200677
16. Liu J, Hao L, Suyou L, et al. Biomechanical properties of lumbar endplates and their correlation with MRI findings of lumbar degeneration. J Biomech. 2016;49(4):586–593. doi:10.1016/j.jbiomech.2016.01.019
17. Schmid G, Witteler A, Willburger R, Kuhnen C, Jergas M, Koester O. Lumbar disk herniation: correlation of histologic findings with marrow signal intensity changes in vertebral endplates at MR imaging. Radiology. 2004;231(2):352–358. doi:10.1148/radiol.2312021708
18. Stirling A, Worthington T, Rafiq M, Lambert PA, Elliott TS. Association between sciatica and Propionibacterium acnes. Lancet. 2001;357(9273):2024–2025. doi:10.1016/s0140-6736(00)05109-6
19. Albert HB, Kjaer P, Jensen TS, Sorensen JS, Bendix T, Manniche C. Modic changes, possible causes and relation to low back pain. Med Hypotheses. 2008;70(2):361–368. doi:10.1016/j.mehy.2007.05.014
20. Lurie JD, Moses RA, Tosteson AN, et al. Magnetic resonance imaging predictors of surgical outcome in patients with lumbar intervertebral disc herniation. Spine. 2013;38(14):1216–1225. doi:10.1097/BRS.0b013e31828ce66d
21. Ohtori S, Yamashita M, Yamauchi K, et al. Low back pain after lumbar discectomy in patients showing endplate Modic type 1 change. Spine. 2010;35(13):E596–E600. doi:10.1097/BRS.0b013e3181cd2cb8
22. MacLean MA, Kureshi N, Shankar J, Stewart SA, Christie SD. Modic change and clinical assessment scores in patients undergoing lumbar surgery for disk herniation. Clin Spine Surg. 2021;34(4):E205–e210. doi:10.1097/bsd.0000000000001076
23. Udby PM, Ohrt-Nissen S, Bendix T, et al. Are Modic changes associated with health-related quality of life after discectomy: a study on 620 patients with two-year follow-up. Spine. 2020;45(21):1491–1497. doi:10.1097/brs.0000000000003618
24. Bostelmann R, Petridis A, Fischer K, Vajkoczy P, Bostelmann T, Barth M. New insights into the natural course and clinical relevance of Modic changes over 2 years following lumbar limited discectomy: analysis of prospective collected data. Eur Spine J. 2019;28(11):2551–2561. doi:10.1007/s00586-019-05988-1
25. Shin SH, Bae JS, Lee SH, Keum HJ, Kim HJ, Jang WS. Transforaminal endoscopic decompression for lumbar spinal stenosis: a novel surgical technique and clinical outcomes. World Neurosurg. 2018;114:e873–e882. doi:10.1016/j.wneu.2018.03.107
26. Chen Q, Zhang Z, Liu B, Liu S. Evaluation of percutaneous transforaminal endoscopic discectomy in the treatment of lumbar disc herniation: a retrospective study. Orthop Surg. 2021;13(2):599–607. doi:10.1111/os.12839
27. Yu P, Zan P, Zhang X, et al. Comparison of percutaneous transforaminal endoscopic discectomy and microendoscopic discectomy for the surgical management of symptomatic lumbar disc herniation: a multicenter retrospective cohort study with a minimum of 2 years’ follow-up. Pain Physician. 2021;24(1):E117–E125.
28. Splendiani A, Bruno F, Marsecano C, et al. Modic I changes size increase from supine to standing MRI correlates with increase in pain intensity in standing position: uncovering the “biomechanical stress” and “active discopathy” theories in low back pain. Eur Spine J. 2019;28(5):983–992. doi:10.1007/s00586-019-05974-7
29. Xu J, Li Y, Wang B, et al. Percutaneous endoscopic lumbar discectomy for lumbar disc herniation with Modic changes via a transforaminal approach: a retrospective study. Pain Physician. 2019;22(6):E601–E608.
30. Lubelski D, Mihalovich KE, Skelly AC, et al. Is minimal access spine surgery more cost-effective than conventional spine surgery? Spine. 2014;39(22Suppl 1):S65–S74. doi:10.1097/brs.0000000000000571
31. Kim CH, Easley K, Lee JS, et al. Comparison of minimally invasive versus open transforaminal interbody lumbar fusion. Global Spine J. 2020;10(2Suppl):143s–150s. doi:10.1177/2192568219882344
32. Yao Y, Liu H, Zhang H, et al. Risk factors for recurrent herniation after percutaneous endoscopic lumbar discectomy. World Neurosurg. 2017;100:1–6. doi:10.1016/j.wneu.2016.12.089
33. Hao L, Li S, Liu J, Shan Z, Fan S, Zhao F. Recurrent disc herniation following percutaneous endoscopic lumbar discectomy preferentially occurs when Modic changes are present. J Orthop Surg Res. 2020;15(1):176. doi:10.1186/s13018-020-01695-6
34. Esposito P, Pinheiro-Franco JL, Froelich S, Maitrot D. Predictive value of MRI vertebral end-plate signal changes (Modic) on outcome of surgically treated degenerative disc disease. Results of a cohort study including 60 patients. Neurochirurgie. 2006;52(4):315–322. doi:10.1016/s0028-3770(06)71225-5
35. Vital JM, Gille O, Pointillart V, et al. Course of Modic 1 six months after lumbar posterior osteosynthesis. Spine. 2003;28(7):
36. Lang P, Chafetz N, Genant HK, Morris JM. Lumbar spinal fusion. Assessment of functional stability with magnetic resonance imaging. Spine. 1990;15(6):581–588. doi:10.1097/00007632-199006000-00028
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
