Back to Journals » International Journal of Women's Health » Volume 8
Comparison of lipid profile parameters and oxidized low-density lipoprotein between normal and preeclamptic pregnancies in a tertiary care hospital in Nepal
Authors Timalsina S, Gyawali P, Bhattarai A
Received 21 July 2016
Accepted for publication 14 September 2016
Published 26 October 2016 Volume 2016:8 Pages 627—631
DOI https://doi.org/10.2147/IJWH.S117850
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
This paper has been retracted.
Santosh Timalsina, 1 Prajwal Gyawali, 2 Aseem Bhattarai 2
1Department of Biochemistry, Chitwan Medical College, Bharatpur, 2Department of Biochemistry, Maharajgunj Medical Campus, Maharajgunj, Kathmandu, Nepal
Introduction: Preeclampsia is a pregnancy-specific complication that significantly contributes to maternal and perinatal morbidity and mortality worldwide, even more so in developing countries such as Nepal. The potential contribution of dyslipidemia and elevated levels of oxidized low-density lipoprotein (oxLDL) in the pathogenesis of preeclamptic pregnancies has been observed in several studies. The aim of this study was to compare the maternal lipid profile parameters and particularly oxLDL between preeclamptic and healthy pregnancies and also correlate oxLDL with other lipid profile parameters.
Patients and methods: A total of 54 preeclamptic women were selected as cases for this cross-sectional study. Age and gestational week-matched 60 pregnant women were enrolled as controls. Preeclampsia was defined as per Australasian Society Consensus Statement research definition. The serum lipid parameters were measured using automated enzymatic systems and a competitive enzyme-linked immunosorbent assay was used to determine oxLDL concentrations in the serum. Student’s t-test was used to compare oxLDL levels between preeclamptic and healthy pregnancies, and Pearson’s correlation analysis was carried out to assess the relation between oxLDL and other variables.
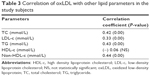
Results: The mean values of serum total cholesterol, triglyceride, non-high-density lipoprotein-cholesterol (non-HDL-c) and oxLDL were significantly higher in the preeclamptic cases (P< 0.01). However, the levels of low-density lipoprotein cholesterol (LDL-c and HDL-c) did not significantly differ between the two groups. oxLDL had a significant positive correlation (P< 0.01) with total cholesterol, triglyceride, LDL-c and non-HDL-c, and a negative correlation with HDL-c.
Conclusion: The atherogenic type of dyslipidemia and high oxLDL levels are associated with preeclamptic pregnancies. The lipid parameters, however, seem to be poor markers of the severity of preeclampsia. Further prospective studies are needed to see if the observed dyslipidemia has a causal role in preeclampsia and imparts a long-term cardiovascular risk.
Keywords: preeclampsia, oxLDL, dyslipidemia, Nepal
Introduction
Preeclampsia is a pregnancy-specific complication characterized by an onset of hypertension, proteinuria, and edema, occurring in the late second trimester (after 20 weeks of gestation). It complicates 5%–6% of all pregnancies and remains a major cause of maternal and perinatal morbidity and mortality worldwide.1 The incidence of hypertensive disorders along with the maternal mortality rates and preterm births related to preeclampsia in the developing countries is higher than those reported in developed countries.2 In Nepal, the incidence of preeclampsia or eclampsia was 20 cases to 1,000 hospital deliveries.3
The upregulation of antiangiogenic factors in the placenta (leading to poor placentation) along with maternal endothelial dysfunction is considered to be one of the most plausible explanations for the pathogenesis and clinical manifestations of preeclampsia.4 There is also a well-established relation between preeclampsia and increased oxidative stress due to endothelial dysfunction, which in turn is potentially contributed by the abnormal lipid profile present in these women.5 The oxidized low-density lipoprotein (oxLDL) results from one of the biologically relevant modifications in LDL in the form of oxidation. The link between oxLDL and cardiovascular diseases has been well established, and interests have developed in finding its association with the pathogenesis of preeclampsia. Dyslipidemia has been found to be one of the strongest predictors of levels of oxLDL in middle-aged adults,6 and the effect seems to be amplified in pregnant women with preeclampsia, where the dyslipidemia is even more pronounced.5
The aim of this study was to compare the maternal lipid profile parameters, particularly oxLDL, between preeclamptic and healthy pregnancies and also correlate oxLDL with other lipid parameters.
Material and methods
This cross-sectional case–control study was conducted in Institute of Medicine, Tribhuvan University Teaching Hospital, Nepal. The tertiary care hospital is situated at approximately 1,400 m (4,600 ft) above the sea level. A total of 54 preeclamptic women (cases) and 60 pregnant women (controls) were enrolled after the written informed consent and ethical approval from the Institutional Review Board of Institute of Medicine. Preeclampsia was defined as new onset of hypertension after 20 weeks of gestation with proteinuria; hypertension was defined as systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg, and proteinuria was considered to be present if the 24-hour urinary total protein excretion was ≥300 mg/24 hours. The preeclamptic cases were categorized as “severe” if severe hypertension was associated with proteinuria or if hypertension was associated with severe proteinuria. The criteria for severe hypertension and severe proteinuria were, respectively: 1) systolic blood pressure ≥160 mmHg or diastolic blood pressure ≥110 mmHg and 2) proteinuria >5 g/24-hour as per Australasian Society Consensus Statement research definition.7 The preeclamptic cases not meeting the aforementioned criteria were categorized as “mild”. Primigravid women diagnosed to have preeclampsia were explained about the study and were enrolled from the maternity ward of the hospital. Age and gestational week-matched pregnant controls were selected from women who visited antenatal checkup clinic.
Serum and urine samples from the cases were collected within 24 hours of diagnosis. In all patients, blood samples were obtained by trained phlebotomist from the most accessible vein taking aseptic precautions and then placed in ethylenediaminetetraacetic acid-containing vials. Blood samples were centrifuged at 4,000 rpm for 5 minutes at room temperature and the separated serum was stored at −40°C until the assays were performed.
The concentrations of the serum lipids (total cholesterol [TC], high-density lipoprotein cholesterol [HDL-c], and triglycerides [TG]) were assayed using automated system (Biotecnica Chemistry Analyzer 3000, Italy) with standard enzymatic assays. LDL-c was calculated using Friedewald’s formula. A competitive enzyme-linked immunosorbent assay (OxLDL ELISA kit, Bio-Ekon, Beijing, People’s Republic of China) was used to determine oxLDL concentrations in the serum.
Data analyses included standard descriptive statistics using SPSS version 20 (IBM Corporation, Armonk, NY, USA), with variables expressed as mean ± standard deviation or medians and range as appropriate. Shapiro–Wilk test was used to test the normality in the distribution of variables. Unpaired Student’s t-test was used for comparison of means between groups for normally distributed variables and Mann–Whitney U-test for comparison of variables that did not follow normal distribution. Pearson’s correlation analysis was performed to examine the association between oxLDL and other variables. A P-value of <0.05 was considered statistically significant.
Results
The case and control groups were not statistically different in age and weeks of gestation. The levels (mean values) of TC, TG, non-HDL-c, and oxLDL were significantly higher in the preeclamptic cases than in pregnant controls. However, the levels of low-density lipoprotein cholesterol (LDL-c) and HDL-c did not significantly differ between the two groups (Table 1).
There was no statistically significant difference in the various lipid parameters while comparing mild and severe preeclampsia cases, except for LDL-c and non-HDL-c (Table 2). The mean values of these two parameters were significantly higher in the severe preeclamptic cases.
There was no correlation of oxLDL with age and gestational period. Table 3 shows the correlation of ox-LDL with other parameters of the lipid profile when all the subjects were considered. A significant positive correlation (P<0.00) between oxLDL and TC, LDL-c, TG, and non-HDL-c was observed (Table 3). OxLDL was negatively correlated with HDL-c (Pearson’s r=−0.06), although not statistically significant.
Discussion
Preeclampsia is a pregnancy-specific condition with evident lipid alterations, somewhat exaggerated than the “physiological” dyslipidemia that occurs in the normal pregnant women. In the current study, significantly higher concentrations of serum TC, TG, and non-HDL-c were found in the preeclamptic cases compared to pregnant controls. The hypertriglyceridemia along with increase in TC and LDL-c observed in this study is in agreement with other studies.8,9 A few studies, however, are not in complete agreement with this.10,11
The role of high-serum TG in the pathogenesis of preeclampsia is a subject of controversy. Earlier studies have hypothesized that hypertriglyceridemia, in preeclampsia, may lead to increased endothelial TG accumulation and generation of small, dense LDL particles, contributing to the endothelial dysfunction.12 The high levels of serum TG in preeclamptic women are believed to be due to high circulating levels of apolipoprotein E that interfere with TG clearance by interfering with lipoprotein lipase activator, apolipoprotein C-II.11 Although elevated TG levels are consistent with preeclamptic cases, no direct relationship has been observed between the TG levels and severity of preeclampsia,13 also evidenced from our study.
Except for the LDL-c and non-HDL-c values, the rest of the lipid parameters were not significantly different between mild and severe preeclampsia. It can be concluded from this study and other studies that the lipid parameters seem to be poor markers of the severity of preeclampsia. Though a rise in LDL-c and a decrease in HDL-c levels were observed in preeclamptic women in this study, the difference with normal pregnant women did not reach statistical significance. Significant changes in LDL-c and HDL-c levels in preeclamptic women have been increasingly suggested as important risk factors for the development of atherosclerosis.14
Belo et al observed higher mean serum TG concentrations and lower HDL-c concentrations with an increased proportion of atherogenic small dense LDL in the preeclamptic women in the third trimester compared with healthy pregnant women.5 Therefore, the physiological “atherogenic” lipid profile in normal pregnancy has been observed to be enhanced in preeclampsia. However, whether, this dyslipidemia is a “cause” or “effect” of endothelial dysfunction, still remains to be answered. Enquobahrie et al concluded that early pregnancy dyslipidemia, especially increased levels of serum TG and serum LDL-c, is associated with an increased risk of preeclampsia.8 It has therefore also been suggested that higher serum TG in pregnant women may warrant further investigation for preeclampsia.15
The contribution of oxLDL in the initiation and progression of the atherosclerotic process and its association with other cardiovascular diseases have been observed in several studies.16,17 In addition, its role in the pathogenesis of preeclampsia has been further sought after. In an early study, oxLDL was found in both villous trophoblasts and placental endothelium, but no significant differences were found in their expression intensities when placental paraffin sections of preeclampsia and controls were compared.10 The circulating levels of oxLDL depend both on the degree of oxidative stress and the number of LDL particles.18 Several studies have shown a strong positive correlation of oxLDL with LDL-c. One such study done on 624 cohorts demonstrated a strong correlation between the two parameters (r=0.67, P<0.001) and also concluded that LDL-c is one of the major determinants of the oxLDL concentration.19 In the current study, along with LDL-c, oxLDL levels also demonstrated a positive correlation with TC, TG, and non-HDL-c levels (Pearson’s r ranging from 0.42–0.44, P-values all <0.01). Similar findings were also evident in the study by Sanchez et al.20
The negative association between HDL-c and oxLDL, although not very strong in our study, is in accordance with studies elsewhere.19 The role of HDL in relation to oxLDL seems to be related with two of the HDL-associated enzymes: paraoxonase 1(PON1) and platelet-activating factor acetylhydrolase. PON1, which is exclusively located in HDL, contributes to the protective effect to oxidative damage by causing the hydrolysis of the LDL lipid peroxides.21 Enhanced serum levels of oxLDL have been shown to be predictive for endothelial dysfunction, with the fact that oxLDL itself induces vascular oxygen radical formation.22 Majority of atherosclerosis studies have demonstrated the relationship between oxLDL and endothelial dysfunction and, the same might hold true in the pathogenesis of preeclampsia. A study by Qiu et al showed that women with elevated oxLDL concentrations (≥50 U/L) had a 2.9-fold increased risk of preeclampsia when compared with women with lower oxLDL concentrations. The risk further increased when the women also had elevated TG concentrations (OR =8.9).23
Preeclampsia is a condition of dyslipidemia that could have possible implications for the development of cardiovascular diseases in later life. In fact, our study demonstrated higher values of atherogenic lipid parameters (TC, TG, non-HDL-c, and oxLDL) in the preeclamptic cases compared with the pregnant controls. Higher oxLDL level in preeclampsia is not just a marker for oxidative stress but could also be a possible risk factor for cardiovascular risk in the future. Previously considered to be a disease of short duration (because of the resolution of symptoms after delivery), preeclampsia is supposed to have an effect that is long term. The principal underlying abnormality, endothelial dysfunction, has been shown to persist in preeclamptic women and further contribution by the dyslipidemia (notably the increase in TG and LDL-c along with the decrease in HDL-c) influences the risk of late-life cardiovascular risk in these women.24 However, further prospective studies are needed to determine whether dyslipidemia in pregnancy, particularly hypertriglyceridemia and elevated LDL-c levels or elevated oxLDL concentrations can predict the occurrence of preeclampsia. Relevant studies are also needed to explore the relationship between this particular type of dyslipidemia and long-term cardiovascular risk.
Acknowledgments
The authors thank Professor Bharat Jha (Head, Department of Biochemistry, Institute of Medicine, Nepal) and Professor Jyoti Sharma (Department of Gynecology and Obstetrics, Institute of Medicine, Nepal) for their insight and encouragement.
Disclosure
The authors report no conflicts of interest in this work.
References
Caritis S, Sibai B, Hauth J, et al. Low-dose aspirin to prevent preeclampsia in women at high risk. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1998;338(11):701–705. | ||
Walker JJ. Pre-eclampsia. Lancet. 2000;356(9237):1260–1265. | ||
Manandhar BL, Chongstuvivatwong V, Geater A. Antenatal care and severe pre-eclampsia in Kathmandu valley. J Chitwan Med College. 2013;3(6):43–47. | ||
Young BC, Levine RJ, Karumanchi SA. Pathogenesis of preeclampsia. Annu Rev Pathol. 2010;5:173–192. | ||
Belo L, Caslake M, Gaffney D, et al. Changes in LDL size and HDL concentration in normal and preeclamptic pregnancies. Atherosclerosis. 2002;162(2):425–432. | ||
Holvoet P, Mertens A, Verhamme P, et al. Circulating oxidized LDL is a useful marker for identifying patients with coronary artery disease. Arterioscler Thromb Vasc Biol. 2001;21(5):844–848. | ||
Brown MA, Hague WM, Higgins J, et al; Australasian Society for the Study of Hypertension in Pregnancy. The detection, investigation and management of hypertension in pregnancy: executive summary. Aust N Z J Obstet Gynaecol. 2000;40(2):133–138. | ||
Enquobahrie DA, Williams MA, Butler CL, Frederick IO, Miller RS, Luthy DA. Maternal plasma lipid concentrations in early pregnancy and risk of preeclampsia. Am J Hypertens. 2004;17(7):574–581. | ||
Kocyigit Y, Atamer Y, Atamer A, Tuzcu A, Akkus Z. Changes in serum levels of leptin, cytokines and lipoprotein in pre-eclamptic and normotensive pregnant women. Gynecol Endocrinol. 2004;19(5):267–273. | ||
Pecks U, Caspers R, Sosnowsky K, et al. Determination of maternal and foetal serum lipid profile and placental oxidised low density lipoprotein accumulation in preeclampsia and normotensive pregnancies. [German]. Z Geburtshilfe Neonatol. 2012;216(5):220–225. | ||
Chalas J, Audibert F, Francoual J, Le Bihan B, Frydman R, Lindenbaum A. Concentrations of apolipoproteins E, C2, and C3 and lipid profile in preeclampsia. Hypertens Pregnancy. 2002;21(3):199–204. | ||
Sattar N, Bendomir A, Berry C, Shepherd J, Greer IA, Packard CJ. Lipoprotein subfraction concentrations in preeclampsia: pathogenic parallels to atherosclerosis. Obstet Gynecol. 1997;89(3):403–408. | ||
Mikhail MS, Basu J, Palan PR, Furgiuele J, Romney SL, Anyaegbunam A. Lipid profile in women with preeclampsia: relationship between plasma triglyceride levels and severity of preeclampsia. J Assoc Acad Minor Phys. 1995;6(1):43–45. | ||
Bayhan G, Kocyigit Y, Atamer A, Atamer Y, Akkus Z. Potential atherogenic roles of lipids, lipoprotein(a) and lipid peroxidation in preeclampsia. Gynecol Endocrinol. 2005;21(1):1–6. | ||
Siddiqui IA. Maternal serum lipids in women with pre-eclampsia. Ann Med Health Sci Res. 2014;4(4):638–641. | ||
Toshima S, Hasegawa A, Kurabayashi M, et al. Circulating oxidized low density lipoprotein levels. A biochemical risk marker for coronary heart disease. Arterioscler Thromb Vasc Biol. 2000;20(10):2243–2247. | ||
Ehara S, Ueda M, Naruko T, et al. Elevated levels of oxidized low density lipoprotein show a positive relationship with the severity of acute coronary syndromes. Circulation. 2001;103(15):1955–1960. | ||
Burgos Alves MI, Aviles Plaza F, Martinez-Tomas R, et al. Oxidized LDL and its correlation with lipid profile and oxidative stress biomarkers in young healthy Spanish subjects. J Physiol Biochem. 2010;66(3):221–227. | ||
van der Zwan LP, Teerlink T, Dekker JM, et al. Circulating oxidized LDL: determinants and association with brachial flow-mediated dilation. J Lipid Res. 2009;50(2):342–349. | ||
Sanchez SE, Williams MA, Muy-Rivera M, Qiu C, Vadachkoria S, Bazul V. A case-control study of oxidized low density lipoproteins and preeclampsia risk. Gynecol Endocrinol. 2005;21(4):193–199. | ||
Mackness MI, Durrington PN, Mackness B. How high-density lipoprotein protects against the effects of lipid peroxidation. Curr Opin Lipidol. 2000;11(4):383–388. | ||
Galle J, Hansen-Hagge T, Wanner C, Seibold S. Impact of oxidized low density lipoprotein on vascular cells. Atherosclerosis. 2006;185(2):219–226. | ||
Qiu C, Phung TT, Vadachkoria S, Muy-Rivera M, Sanchez SE, Williams MA. Oxidized low-density lipoprotein (Oxidized LDL) and the risk of preeclampsia. Physiol Res. 2006;55(5):491–500. | ||
Charlton F, Tooher J, Rye KA, Hennessy A. Cardiovascular risk, lipids and pregnancy: preeclampsia and the risk of later life cardiovascular disease. Heart Lung Circ. 2014;23(3):203–212. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.