Back to Journals » OncoTargets and Therapy » Volume 9
Comparison of internal target volumes defined on 3-dimensional, 4-dimensonal, and cone-beam CT images of non-small-cell lung cancer
Authors Li F, Li J, Ma Z, Zhang Y, Xing J, Qi H, Shang D
Received 23 April 2016
Accepted for publication 20 September 2016
Published 17 November 2016 Volume 2016:9 Pages 6945—6951
DOI https://doi.org/10.2147/OTT.S111198
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Min Li
Fengxiang Li,1 Jianbin Li,1 Zhifang Ma,1 Yingjie Zhang,1 Jun Xing,1 Huanpeng Qi,1 Dongping Shang2
1Department of Radiation Oncology, 2Department of Big Bore CT Room, Shandong Cancer Hospital Affiliated to Shandong University, Shandong Academy of Medical Sciences, Jinan, Shandong, People’s Republic of China
Purpose: The purpose of this study was to compare the positional and volumetric differences of internal target volumes defined on three-dimensional computed tomography (3DCT), four-dimensional CT (4DCT), and cone-beam CT (CBCT) images of non-small-cell lung cancer (NSCLC).
Materials and methods: Thirty-one patients with NSCLC sequentially underwent 3DCT and 4DCT simulation scans of the thorax during free breathing. The first CBCT was performed and registered to the planning CT using the bony anatomy registration during radiotherapy. The gross tumor volumes were contoured on the basis of 3DCT, maximum intensity projection (MIP) of 4DCT, and CBCT. CTV3D (clinical target volume), internal target volumes, ITVMIP and ITVCBCT, were defined with a 7 mm margin accounting for microscopic disease. ITV10 mm and ITV5 mm were defined on the basis of CTV3D: ITV10 mm with a 5 mm margin in left–right (LR), anterior–posterior (AP) directions and 10 mm in cranial–caudal (CC) direction; ITV5 mm with an isotropic internal margin (IM) of 5 mm. The differences in the position, size, Dice’s similarity coefficient (DSC) and inclusion relation of different volumes were evaluated.
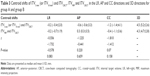
Results: The median size ratios of ITV10 mm, ITV5 mm, and ITVMIP to ITVCBCT were 2.33, 1.88, and 1.03, respectively, for tumors in the upper lobe and 2.13, 1.76, and 1.1, respectively, for tumors in the middle-lower lobe. The median DSCs of ITV10 mm, ITV5 mm, ITVMIP, and ITVCBCT were 0.6, 0.66, and 0.83 for all patients. The median percentages of ITVCBCT not included in ITV10 mm, ITV5 mm, and ITVMIP were 0.1%, 1.63%, and 15.21%, respectively, while the median percentages of ITV10 mm, ITV5 mm, and ITVMIP not included in ITVCBCT were 57.08%, 48.89%, and 20.04%, respectively.
Conclusion: The use of the individual ITV derived from 4DCT merely based on bony registration in radiotherapy may result in a target miss. The ITVs derived from 3DCT with isotropic margins have a good coverage of the ITV from CBCT, but the use of those would result in a high proportion of normal tissue being irradiated unnecessarily.
Keywords: non-small-cell lung cancer, cone-beam CT, four-dimensional CT, three-dimensional CT, internal target volume, volume comparison
Introduction
Accurate target definition is essential for high precision radiation therapy (HPRT) of non-small-cell lung cancer (NSCLC).1,2 Respiration-induced tumor motion not only reduces the accuracy of target delineation on volumetric images but increases the uncertainty in treatment planning and delivery.3 It is extraordinarily important to account for tumor motion in target definition.
For conventional treatment planning based on three-dimensional computed tomography (3DCT), a population-based margin is used to estimate tumor motion, which would result in a high proportion of normal tissue being irradiated unnecessarily or a geometric miss.4 Four-dimensional CT (4DCT) is commonly used to access tumor motion throughout respiratory cycle. The individual internal target volumes (ITVs) were generated based on 10 phases or maximum intensity projection (MIP) of 4DCT.5,6 Although the use of 4DCT ITVs significantly reduces target volumes in treatment planning compared to 3DCT ITVs,4,7 researchers question the accuracy of 4DCT ITVs8,9 since they are not sure whether the individual ITVs acquired in simulation accord with the real targets in radiation delivery.
The scan time of cone-beam CT (CBCT) mounted on the gantry of accelerator takes more than 60 s and spans several respiratory cycles. Individual online ITVs can be generated based on CBCT images.10,11 The use of CBCT for online setup corrections has been confirmed. However, because of rapid development of HPRT, merely using CBCT for setup corrections has not met our demands. There is growing interest in the use of CBCT images in image-guided radiation therapy and adaptive radiation therapy including CBCT-based target delineation, target definition, dose calculation, and so on.12–15
In the present study, the differences in target position, volume, similarity, and inclusion relation of the conventional ITVs defined on 3DCT, the individual ITV on the MIP of 4DCT, and the individual online ITV on CBCT were analyzed. The aim of this study was to evaluate the accuracy of ITVs defined on 3DCT and 4DCT and investigate the use of CBCT combined with 3DCT and 4DCT in the definition of target volumes.
Materials and methods
Patient characteristics
Thirty-one patients with peripheral NSCLC underwent axial 3DCT and 4DCT simulation scanning for treatment planning between March 2010 and May 2015 in Shandong Cancer Hospital affiliated to Shandong University. The study was approved by the Institutional Review Board. All the patients provided written informed consent prior to treatment planning. Patient and tumor characteristics are listed in Table 1.
  | Table 1 Patient and tumor characteristics |
CT simulation and image acquisition
During simulation, all the patients were immobilized using vacuum bags in the supine position with the arms raised above the head. For each patient, an axial 3DCT scan of the thoracic region was performed, followed by a 4DCT scan during free breathing on Brilliance Bores CT simulator (Philips Medical Systems, Highland Heights, OH, USA). The 3DCT and 4DCT acquisition protocols have been reported in a previous study.4 The 4DCT images were sorted into 10 bins according to the phase of the breathing signal. MIPs of the 4DCT data sets were then generated, which contain the maximum Hounsfield unit (HU) in each geometric voxel across all time-resolved data sets.6,16 All the CT images were reconstructed with a thickness of 3 mm and then transferred to Eclipse treatment planning system (Eclipse 8.6; Varian Medical Systems, Palo Alto, CA, USA). For all the patients, three-dimensional conformal radiotherapy or intensity-modulated radiation therapy treatment planning was performed on the basis of 3DCT.
Online image acquisition
On the linear accelerator, the patients were aligned according to the skin tattoos by using the in-room laser system. The CBCT images were acquired with the gantry-mounted onboard imager (Varian Medical Systems). The first CBCT image was acquired immediately after setup. The scan time takes ~60 s, and ~650 2D kV images are captured during the full 360° rotation. CBCT images were reconstructed with a thickness of 2.5 mm. The CBCT scan was rigidly registered to the planning CT scan. An automatic registration of the bony anatomy was performed using a user-defined region of interest including the spinal cord. The registration was evaluated by the radiation therapists and manually corrected if necessary. Then, the registered CBCT images were automatically transferred to Eclipse treatment planning system.
Target delineation
The gross tumor volumes (GTVs) were manually delineated on 3DCT, CBCT, 10 phases, and MIP of the 4DCT and by a radiation oncologist. The targets were delineated according to the following protocol: 1) The GTVs were delineated using lung window setting (window width: 1,600 HU and window level: −600 HU). 2) The use of the mediastinum window (40/400 HU) was allowed for information purposes to avoid the inclusion of adjacent vessels and mediastinal or chest wall structures.12 3) Blurring in the periphery of the tumor, representing the “partial volume effect” and “partial projection effect for moving objects,” was included in the GTVs.17 The GTVs contoured on the basis of 3DCT, 4DCT, MIP, and CBCT of Patient 19 showed in Figure 1.
Definition of PTVs
CTV3D, ITVMIP, and ITVCBCT were defined by adding a 7 mm margin to GTVs delineated on 3DCT, 4DCT, MIP, and CBCT accounting for microscopic disease. ITV10 mm and ITV5 mm were defined on the basis of CTV3D: ITV10 mm with a 5 mm margin in LR, AP directions, and 10 mm in CC direction; ITV5 mm with an isotropic internal margin (IM) of 5 mm.
Tumor motion
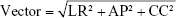
The coordinates in left–right (LR), anterior–posterior (AP), and cranial–caudal (CC) directions of the center of mass (COM) of GTVs in 10 phases of 4DCT were measured. The peak-to-peak displacement of COM in three directions was calculated on the basis of the coordinates, which represents the tumor motion. The 3D motion vector (vector) of COM was calculated as follows:
|
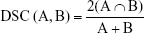
Comparison of ITVs
Position, volume, Dice’s similarity coefficient (DSC),2 and inclusion relation between ITV10 mm, ITV5 mm, ITVMIP, and ITVCBCT were compared, respectively. Positions of ITVs are represented by COM coordinates. The DSC of volume A and B is defined as the ratio of the volume of their intersection to their average volume, with a value of 1 indicating identical and 0 indicating no overlap of two volumes. The formula is as follows:
|
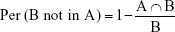
The percentage of B not included in A [Per (B not in A)] is used to indicate the inclusion relation between two volumes. Assumed volume A was reference for the real volume irradiated. If the treatment planning was based on volume B, there would be Per (A not in B) of volume A missing irradiation and Per (B not in A) of volume B being irradiated unnecessarily. The formula is as follows:
|
Statistical analysis
Statistical analysis was performed using the SPSS 16.0 software package (SPSS Inc., Chicago, IL, USA). The Wilcoxon paired sum test was used for the comparison of tumor motion, position, volume, DSC, and inclusion relation. For the comparison of data between groups A and B, the Wilcoxon independent sum test was used. The Spearman sum test was used for correlation analysis. The level of significance was a two-sided P-value of <0.05 for all the tests.
Results
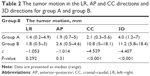
The tumor motions for groups A and B are presented in Table 2. The median tumor motion amplitude in 3D direction was 4 mm for group A and 11.2 mm for group B, with a significant statistical difference (P<0.001). Table 3 presents the centroid shifts between ITV5 mm (or ITV10 mm) and ITVCBCT, ITVMIP, and ITVCBCT. Two related sample tests indicated the difference of centroid coordinates between ITVMIP and ITVCBCT in LR direction, ITV5 mm and ITVCBCT in CC direction is approximately significant (P=0.083 and 0.07).
ITV size and the size ratios of ITV10 mm, ITV5 mm, ITVMIP to ITVCBCT are listed in Table 4. A significant inverse correlation was found for the ratio of ITV5 mm to ITVCBCT to tumor motion vector for all the patients (r=−0.373, P=0.039).
Figure 2 illustrates the DSCs of ITV10 mm and ITVCBCT, ITV5 mm and ITVCBCT, and ITVMIP and ITVCBCT for each patient. The median DSC of ITVMIP and ITVCBCT was 0.83 (range 0.61–0.92), which was greater than the DSC of ITV10 mm and ITVCBCT (median 0.60 and range 0.46–0.79; P<0.001) and DSC of ITV5 mm and ITVCBCT (median 0.66 and range 0.50–0.83; P<0.001). The DSCs of ITV10 mm and ITVCBCT, ITV5 mm and ITVCBCT, and ITVMIP and ITVCBCT showed no correlation to tumor motion vector (P>0.05, respectively).
The percentages of ITV10 mm, ITV5 mm, and ITVMIP not included in ITVCBCT and the percentages of ITVCBCT not in ITV10 mm, ITV5 mm, and ITVMIP are presented in Table 5. Percentage of ITVMIP not in ITVCBCT was less than percentage of ITV10 mm not in ITVCBCT (P<0.001) and percentage of ITV5 mm not in ITVCBCT (P<0.001). Percentage of ITVCBCT not in ITV10 mm was less than percentage of ITVCBCT not in ITV5 mm (P<0.001) and percentage of ITVCBCT not in ITVMIP (P<0.001).
Discussion
The centroid shifts of targets could directly influence the DSC and the inclusion relation between targets. In the present study, the difference in centroid position between ITVs was initially evaluated. The relatively large standard deviation (SD) (1.9–4.1 mm) to the mean in centroid position indicated a great difference in the shifts of ITVs among individual patient. The large centroid shifts of ITVs in 3D direction (mean, ~5 mm) also demonstrated it. The centroid shifts of ITVs in CC direction were greater than the shifts in LR or AP direction (P<0.05, respectively), which indicated that the respiration-induced tumor motion could impact on the centroid shifts of targets due to the large tumor motion in CC direction. Additionally, using bony registration may increase the centroid shifts of ITVs. Wulf et al18 showed a poor correlation in the position between mobile soft tissue tumors and bony anatomy. The SDs of the shifts of mobile soft tissue tumors and the bony anatomy were 3.3, 5.2, and 4.5 mm in LR, AP, and CC directions, respectively. Yeung et al19 reported the difference in the couch shifts between bony and soft tissue registration was 5.4±5.7 mm in 3D direction.
4DCT has been considered as a reliable tool for assessing tumor motion.20,21 Comparing ITVCBCT size with ITVMIP contributes to evaluate the respiratory motion information encompassed in CBCT images. Our study indicated a median of 3% increase of ITVMIP size than ITVCBCT for group A (P=0.055) and a median of 10% increase for group B (P=0.005). Recent data by other authors10,11 support this observation. Wang et al10 showed that the volumetric difference between ITVs from CBCT and 4DCT was within 8.7% and 8.0% for the phantom and clinical cases, respectively. Liu et al11 reported that the ITV from CBCT has a median 11.8% (range, −49.8 to +24.3%, P<0.001) reduction by the ITV derived from end-inhale and end-exhale respiratory phase of 4DCT. They found that the relative target motion was not the significant factor (P=0.323) causing underestimation of ITV in CBCT. The present study also found the ratio of ITVMIP to ITVCBCT which showed no correlation with the motion vector (P=0.153), and the difference of the ratio of ITVMIP to ITVCBCT for groups A and B was not significant (P>0.05). Therefore, the tumor motion could not impact the relative motion information included in CBCT compared to 4DCT. The CBCT images can be used to account for the individual online tumor motion well, but the motion information in CBCT is less than that in 4DCT.
Analyzing the DSC and inclusion relation of targets which integrate the position and size with shape information can reveal geometric features of different targets.2,4,5 This study indicated a good similarity between ITVMIP and ITVCBCT with a median DSC of 0.83. Nonetheless, there would be a median of 15.21% of ITVCBCT missing irradiation and 20.04% ITVMIP being irradiated unnecessarily, if ITVMIP is used in the treatment planning. These results challenged the accuracy of the individual ITV defined on 4DCT. The difference in size did not significantly change the inclusion relation of targets, since ITVCBCT size has a median of only 6% decrease than ITVMIP for all patients. So the position and shape of targets may be the major factors influencing on the inclusion relation. Respiratory variations in simulation and radiation delivery could cause changes in the position and shape of targets. The registration error based on bony anatomy may increase the centroid shifts of targets.18,19 Therefore, expanding another margin/using soft tissue registration and visual rectification between planning CT and CBCT may improve the accuracy of 4DCT ITV.19,22,23
In addition, our data showed that ITV10 mm and ITV5 mm sizes were far larger than ITVCBCT for both groups. The large difference in size inevitably results in poor DSCs of ITV10 mm and ITVCBCT and ITV5 mm and ITVCBCT. It was also found that there would be a median of 57.08% of ITV10 mm or 48.89% of ITV5 mm being irradiated unnecessarily if treatment planning was created on ITV10 mm or ITV5 mm. The target size being irradiated unnecessarily was far larger than that when treatment planning was created on ITVMIP. However, the risk of missing irradiation was very small if radiation delivery was based on ITV10 mm or ITV5 mm, with a median of 0.1% of ITV10 mm or 1.63% of ITV5 mm missing irradiation.
For group A, the median percentage of ITVCBCT not in ITV5 mm was 1.24% (range, 0%–17.88%), and the median tumor motion in CC direction was 2.1 mm. It is reasonable to add a 5 mm margin in CC direction accounting for tumor motion. The median percentage of ITVCBCT not in ITV5 mm was 5.8% (range, 0%–21.42%) for group B, which was not significantly greater than that for group A (P=0.404). Hence, it is feasible to add a 5 mm margin in CC direction for tumors in the middle-lower lobe in most cases. But using a 5 mm margin should be cautious for tumors with large motion due to the negative correlation between the ratio of ITV5 mm to ITVCBCT and tumor motion (r=−0.373, P=0.039).
The ITVs derived from 3DCT based on isotropic margins have a good coverage of on time tumor motion, which have no special requirement for the pattern of registration. But the ITVs are not suitable for Stereotactic body radiotherapy (SBRT) due to a high proportion of normal tissue being possibly irradiated unnecessarily. The individual ITV from 4DCT can usually encompass the tumor motion in treatment. However, its usage is required for soft tissue registration and visual rectification. The individual ITV can be used for highly precise SBRT, which can increase the biological dose effect of radiation and the local tumor control rate.
It should be noted that the poor quality of CBCT images may increase the delineation error. This study established a strict delineation standard, and all the delineations were performed by an oncologist in order to reduce error. The ITVs delineated based on CBCT and MIP images may not fully encompass the tumor motion if an adjacent structure has equal or greater density.11,16 In addition, the ITVs may be underestimated in both 4DCT and CBCT images due to irregular breathing patterns.23,24
Conclusion
In the present study, the CBCT can encompass tumor motion well, but the respiratory motion information included in CBCT is less than that in 4DCT. The individual ITV derived from 4DCT can generally encompass the tumor motion in treatment, but the use of it in radiotherapy merely based on bony registration may result in a target miss. The ITVs from 3DCT with isotropic margins have a good coverage of tumor motion, while use of it may lead to a high proportion of normal tissue being irradiated unnecessarily. It may be feasible to generate the population-based ITV with an isotropic IM of 5 mm for tumors in the middle-lower lobe in most cases.
Disclosure
The authors report no conflicts of interest in this work.
References
Li G, Citrin D, Camphausen K, et al. Advances in 4D medical imaging and 4D radiation therapy. Technol Cancer Res Treat. 2008;7:67–81. | ||
van Dam IE, van Sörnsen de Koste JR, Hanna GG, et al. Improving target delineation on 4-dimensional CT scans in stage I NSCLC using a deformable registration tool. Radiother Oncol. 2010;96:67–72. | ||
Purdie TG, Moseley DJ, Bissonnette JP, et al. Respiration correlated cone-beam computed tomography and 4DCT for evaluating target motion in Stereotactic Lung Radiation Therapy. Acta Oncol. 2006;45:915–922. | ||
Li FX, Li JB, Xing J, et al. Analysis of the advantage of individual PTVs defined on axial 3D CT and 4D CT images for liver cancer. J Appl Clin Med Phys. 2012;13:62–71. | ||
Ezhil M, Vedam S, Balter P, et al. Determination of patient-specific internal gross tumor volumes for lung cancer using four-dimensional computed tomography. Radiat Oncol. 2009;4. | ||
Muirhead R, McNee SG, Featherstone C, et al. Use of Maximum Intensity Projections (MIPs) for target outlining in 4DCT radiotherapy planning. J Thorac Oncol. 2008;3:1433–1438. | ||
Li FX, Li JB, Zhang YJ, et al. Comparison of the planning target volume based on three-dimensional CT and four-dimensional CT images of non-small-cell lung cancer. Radiother Oncol. 2011;99:176–180. | ||
Britton KR, Starkschall G, Tucker SL, et al. Assessment of gross tumor volume regression and motion changes during radiotherapy for non-small-cell lung cancer as measured by four-dimensional computed tomography. Int J Radiat Oncol Biol Phys. 2007;68:1036–1046. | ||
James SS, Mishra P, Hacker F, et al. Quantifying ITV instabilities arising from 4DCT: a simulation study using patient data. Phys Med Biol. 2012;57:L1–L7. | ||
Wang Z, Wu J, Marks LB, et al. Cone-beam CT localization of internal target volumes for stereotactic body radiotherapy of lung lesions. Int J Radiat Oncol Biol Phys. 2007;69:1618–1624. | ||
Liu HW, Khan R, D’Ambrosi R, et al. The influence of target and patient characteristics on the volume obtained from cone beam CT in lung stereotactic body radiation therapy. Radiother Oncol. 2013;160:312–316. | ||
Altorjai G, Fotina I, Lütgendorf-Caucig C, et al. Cone-beam CT-based delineation of stereotactic lung targets: the influence of image modality and target size on interobserver variability. Int J Radiat Oncol Biol Phys. 2012;82:e265–e272. | ||
Hawkins MA, Brooks C, Hansen VN, et al. Cone beam computed tomography-derived adaptive radiotherapy for radical treatment of esophageal cancer. Int J Radiat Oncol Biol Phys. 2010;77:378–383. | ||
Yoo S, Yin FF. Dosimetric feasibility of cone-beam CT-based treatment planning compared to CT-based treatment planning. Int J Radiat Oncol Biol Phys. 2006;66:1553–1561. | ||
Harsolia A, Hugo GD, Kestin LL, et al. Dosimetric advantages of four-dimensional adaptive image-guided radiotherapy for lung tumors using online cone-beam computed tomography. Int J Radiat Oncol Biol Phys. 2008;70:582–589. | ||
Underberg RWM, Lagerwaard FJ, Slotman BJ, et al. Use of maximum intensity projections (MIP) for target volume generation in 4DCT scans for lung cancer. Int J Radiat Oncol Biol Phys. 2005;63:253–260. | ||
Persson GF, Nygaard DE, Munck AF, Rosenschöld P. Artifacts in conventional computed tomography (CT) and free breathing four-dimensional CT induce uncertainty in gross tumor volume determination. Int J Radiat Oncol Biol Phys. 2011;80:1573–1580. | ||
Wulf J, Hadinger U, Oppitz U, et al. Stereotactic radiotherapy of extracranial targets: CT-simulation and accuracy of treatment in the stereotactic body frame. Radiother Oncol. 2000;57:225–236. | ||
Yeung AR, Li JG, Shi W, et al. Tumor localization using cone-beam CT reduces setup margins in conventionally fractionated radiotherapy for lung tumors. Int J Radiat Oncol Biol Phys. 2009;74:1100–1107. | ||
Weiss E, Wijesooriya K, Dill SV, Keall PJ. Tumor and normal tissue motion in the thorax during respiration: analysis of volumetric and positional variations using 4D CT. Int J Radiat Oncol Biol Phys. 2007;67:296–307. | ||
Liu HH, Balter P, Tutt T, et al. Assessing respiration-induced tumor motion and internal target volume using four-dimensional computed tomography for radiotherapy of lung cancer. Int J Radiat Oncol Biol Phys. 2007;68:531–540. | ||
Cai J, McLawhorn R, Read PW, et al. Effects of breathing variation on gating window internal target volume in respiratory gated radiation therapy. Med Phys. 2010;37:3927–3934. | ||
Clements N, Kron T, Franich RT, et al. The effect of irregular breathing patterns on internal target volumes in four-dimensional CT and cone-beam CT images in the context of stereotactic lung radiotherapy. Med Phys. 2013;40:021904. | ||
Vergalasova I, Maurer J, Yin FF. Potential underestimation of the internal target volume (ITV) from free-breathing CBCT. Med Phys. 2011;38:4. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.