Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 15
Comparison of in vitro Killing Effect of N, N-Diethyl-Meta-Toluamide (DEET) versus Permethrin on Demodex folliculorum
Authors Paichitrojjana A , Chalermchai T
Received 27 May 2022
Accepted for publication 6 July 2022
Published 9 July 2022 Volume 2022:15 Pages 1301—1307
DOI https://doi.org/10.2147/CCID.S376454
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Anon Paichitrojjana, Thep Chalermchai
School of Anti-Aging and Regenerative Medicine, Mae Fah Luang University, Bangkok, Thailand
Correspondence: Thep Chalermchai, School of Anti-Aging and Regenerative Medicine, Mae Fah Luang University, 36/87-88 PS Tower 25Fl, Asoke Road, Sukhumvit 21, Klong Toey Nua, Wattana, Bangkok, 10110, Thailand, Tel +66-2-6644360, Email [email protected]
Background: There is no single effective treatment for demodicosis; successful treatment requires a multimodal approach. Relapse or recurrence of demodicosis is relatively high, making the therapy challenging. Several reports have documented the successful treatment of demodicosis with acaricidal agents, which aimed at reducing the excessive number of Demodex mites and improving the patients’ symptoms. Reports of irritation and resistance to topical acaricidal agents have led to the search for effective alternative treatments.
Materials and Methods: A total of 100 standardized skin surface biopsy (SSSB) biopsy slides from 100 patients with demodicosis were randomly divided into five groups, each with 20 slides exposed to immersion oil, N, N-diethyl-meta-toluamide (DEET) 5%, 10%, 20%, and permethrin 1%, respectively. The microscopic evaluation started immediately after the test agents exposed the mites. The survival time (ST) was defined as the interval between the first exposure of Demodex folliculorum to the test agents to the time the movements ceased.
Results: The differences between the median ST of DEET 5% (44 min), 10% (22 min), and 20% (14 min) were significant when compared to the negative control group (240 min) with p< 0.001, < 0.001, < 0.001, respectively. While the median ST of permethrin 1% (42 min) was not significantly different from the median ST of DEET 5% (p=0.7395).
Conclusion: This study demonstrated the dose-related acaricidal effect of DEET on D. folliculorum. The survival times of DEET 5%, 10%, and 20% were significantly shorter than the negative control (immersion oil). DEET 5% had a comparable in vitro killing effect as permethrin 1%. Further in vivo studies are necessary to determine the clinical efficacy in patients with demodicosis.
Keywords: Demodex mites, demodicosis, N, N-diethyl-meta-toluamide, DEET, permethrin, in vitro killing effect
Introduction
Demodex mite can cause a variety of skin disorders known as demodicosis. Clinical signs of demodicosis include dry, itchy, scaly skin, redness, increased skin sensitivity, burning, stinging sensation, rough skin like sandpaper, papulopustular lesions, and blepharitis. Demodicosis should be considered in differential diagnoses of unexplained eczema, seborrheic dermatitis, bacterial folliculitis, acne, perioral dermatitis, eosinophilic folliculitis, and blepharitis.1 Furthermore, many studies revealed that rosacea patients also have a significantly higher density of Demodex mites than the average population.2–4 The density of Demodex mites is an important factor in the appearance of clinical symptoms. Demodicosis can be diagnosed by clinical presentations and standardized skin surface biopsy (SSSB), which is abnormal when there are more than 5 mites/cm2.5–9
Several reports have documented the successful treatment of demodicosis and rosacea with acaricidal agents, which aimed to reduce the excessive number of Demodex mites and improve the patients’ symptoms.10–16 Many topical acaricidal agents can cause mild to moderate irritation.10,13 Moreover, resistance to these medications in Pediculus humanus capitis and Sarcoptes scabiei has been reported.17–19
The limitations of topical acaricidal agents have urged a search for an alternative treatment.
N, N-diethyl-meta-toluamide (DEET) has been registered for commercial use as an insect repellent for more than six decades.20,21 Recently, the in vitro Sarcoptes scabiei killing ability of DEET has been reported, but the in vitro Demodex mite killing effect has never been investigated.22
Permethrin is a commonly prescribed agent for demodicosis and scabies in Thailand. Studies have demonstrated that topical permethrin, crotamiton, benzyl benzoate, and ivermectin are effective in the treatment of demodicosis and all significantly decreased the Demodex count.13–16 A review included randomized controlled trials demonstrating no difference in permethrin effectiveness compared to systemic or topical ivermectin for scabies.23 Thus, the authors had permethrin as a positive control agent in the current study.
Although permethrin 1% is safer than 5%, the in vitro Demodex killing effect of permethrin 1% has not been explored. The authors included permethrin 1% as a positive control agent in this study. This study aims to investigate the in vitro killing effect of different concentrations of DEET versus permethrin 1% on D. folliculorum from SSSB slides of demodicosis patients.
Materials and Methods
Materials
Permethrin 1% solution is produced by HUNTER GROUP LIMITED PARTNERSHIP (Thailand). DEET 20% solution is a product from The British Dispensary (L.P.) Co., Ltd. (Thailand) and diluted with propylene glycol to the other study concentrations of 10% and 5%.
Demodex Mites
The SSSB was performed during the consultation to determine the density of Demodex mites, by pressing two glass slides containing a drop of cyanoacrylate glue against the skin surface on both cheeks of the patients, one slide on each cheek, for 1 min before slowly and gently peeling them off. The first slide was exposed to immersion oil and covered with a coverslip to evaluate the density of Demodex mites, the second slide was randomly exposed to immersion oil or test agents and covered with a coverslip immediately for this trial under a microscope. The investigator selected only one D. folliculorum, the most active mite from each slide, as the study’s subject for observation. The initiation of the microscopic evaluation occurred immediately after the mites were contacted with immersion oil or test agents.
Methods
A total of 100 SSSB slides from 100 patients with demodicosis were randomly divided into five groups, each with 20 slides. The positive control group was exposed directly to permethrin 1%, while the negative control group was exposed to immersion oil. The last three test groups were directly applied with DEET 5%, 10%, and 20%, respectively. The investigator was unaware of the test agent in each slide observed under a microscope. Viability was evaluated for 240 min by periodic observation of each slide for the movement of D. folliculorum’s head, body, and legs through the microscope. The observation period was 1 min in every 2 min of the first hour, and after that occurred every 10 min of the second hour and every 30 min of the third and the fourth hour of the study. Definition of the survival time (ST) is the interval between the first exposure of D. folliculorum to the test agents to the time the movements ceased. This cessation described the absence of any motion over two consecutive observation periods (2 min). The average ST from each study group was compared to evaluate the in vitro killing effect.
Statistical Analysis
Statistical analyses were performed using statistical software for data science, STATA for Windows, version 11.1. Numerical variables were shown as median, interquartile range, mean, and standard deviation (SD). The survival analysis using the Kaplan-Meier method demonstrated ST between the test agents. The comparison of ST between groups was evaluated by a Log rank test, p-value less than 0.05 was considered significant in all comparisons.
Results
The median ST of DEET 5%, 10%, 20%, and permethrin 1% were 44 min (IQR: 40–48 min), 22 min (IQR: 20–24 min), 14 min (IQR: 14–16 min) and 42 min (IQR: 40–46 min), respectively. All test agents were able to kill the mites within the first hour of exposure, except for two mites in permethrin 1% that had ST at 80 min. While all the mites survived in the negative control group (immersion oil) for up to 240 min of observation. The ST showed an inverse correlation with the DEET concentration, confirming the dose-related acaricidal effect among all DEET groups (Table 1).
 |
Table 1 The Survival Time of D. folliculorum from Standardized Skin Surface Biopsy Slides in Different Test Agents |
The differences between the median ST of DEET 5%, 10%, 20%, and permethrin 1% were statistically significant compared to the negative control group (p<0.001). The median ST of DEET 10% and 20% were significantly shorter than permethrin 1% (p<0.001, p<0.001, respectively), while DEET 5% did not show significant difference from permethrin 1% (p=0.7395) (Table 2). Kaplan-Meier cumulative D. folliculorum survival curves of the five test agent groups are presented in Figure 1. Comparison of the differences in the median ST between test agents using the Log rank test are shown in Figure 2.
 |
Table 2 To Compare the Median Survival Time Difference Between the Pairs Using the Log Rank Test |
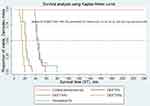 |
Figure 1 Kaplan-Meier, survival curve to demonstrate the survival time between the test agents. Abbreviation: DEET, N,N-diethyl-meta-toluamide. |
 |
Figure 2 To compare the median survival time difference between the pairs using the Log rank test. Abbreviation: DEET, N,N-diethyl-meta-toluamide. |
Discussion
This trial was performed in the adult form of D. folliculorum only because the SSSB collects mainly D. folliculorum, and previous studies have found that D. folliculorum is more tolerable to acaricidal agents than D. brevis.24–26 Although permethrin 5% is widely used because it is more available in the market, many dermatologists prefer to use permethrin 1% as it has less skin irritation and side effects. A previous study showed the mean ST of Demodex mites in permethrin 5% was 12.5 ± 1.9 min, while the mean ST in permethrin 1% was 47.2 ±12.3 min (in this trial) which led to the conclusion that permethrin has a dose-related acaricidal effect.27
Interestingly, two of the Demodex mites in permethrin 1% survived up to 80 min, while the remaining 18 mites in the same group had median ST at 42 min. It is possible that they were younger than the others, or the concentration of permethrin 1% may not be sufficient to kill all Demodex mites, or these mites may be less responsive or resistant to permethrin treatment, as had been reported in lice and scabies before.17–19
DEET has been used as an active ingredient in insect-repellent products for the US Army since 1946 and registered for public commercial use in 1957.21 Products registered for human use can have a percentage of DEET from 4 to 100%. However, the most common concentration of products on the market is 30–40%.28 DEET has become one of the most popular insect repellents, with 200 million applications annually worldwide for preventing bites from arthropods such as mosquitoes, black flies, ticks, mites, and fleas.20 The mechanism of action of DEET is not fully understood, with several reports showing that odor, contact, and ingestion can prevent insect bites.21 Insect repellents generally work by preventing insects from landing on human skin. However, many studies have shown that DEET also has insecticidal and acaricidal effects.29,30 There is evidence showing that DEET works by interacting with insect’s odorant and gustatory receptors.31 DEET is likely targeting octopaminergic synapses and disrupting the calcium equilibrium in the nerve cells to induce neuroexcitation and toxicity in insects. The low potency of DEET for inhibiting human acetylcholinesterase makes it unlikely to cause toxicity in humans by this mechanism.32
The United States Environmental Protection Agency revealed minor side effects of DEET depending on the exposure route. DEET was classified to be as low toxicity (category III) based on the oral study, very low toxicity (category IV) based on an inhalation LC50 study, low toxicity for the eye, and very low toxicity for dermal irritation. Chronic toxicity studies did not show evidence of carcinogenicity.33 Furthermore, there is a study about the effects of DEET exposure on human health using population-based data demonstrated that there was no significant correlation between DEET metabolite levels and biomarkers related to systemic inflammation (high sensitivity C-reactive protein), immune function (lymphocyte), liver function (aspartate aminotransferase, alanine aminotransferase, and γ-glutamyl transferase), and kidney function (estimated glomerular filtration rate).21
This study discovered that the ST of DEET 5% was equivalent to permethrin 1%, while the ST of DEET 10% and 20% were shorter in duration. DEET could be another option for demodicosis treatment. Since the most important thing in managing demodicosis is balancing the acaricidal effect and the safety of the treatment, the authors suggest that DEET 10% is probably the appropriate concentration for the further clinical trial.
The limitations of this study are the small number of Demodex mites, the age of the different mites at the beginning of the observation was not known, and comparison with propylene glycol alone (added to dilute) and other acaricidal agents (ivermectin, benzyl benzoate) was not performed.
Conclusion
The survival times of DEET 5%, 10%, and 20% were significantly shorter than the negative control (immersion oil). DEET 5% had a comparable in vitro killing effect as permethrin 1%. This is the first study that demonstrated the dose-dependent acaricidal effect of DEET. The findings of this study are limited to in vitro experiments and do not entirely reflect the efficacy of these agents in clinical practice; further in vivo investigations are necessary to determine the treatment efficacy of DEET in patients with demodicosis.
Data Sharing Statement
Unavailable data, but the reader can personally request to access the data via Dr. Anon Paichitrojjana; E-mail: [email protected].
Statement of Ethics
The study was conducted in accordance with the World Medical Association Declaration of Helsinki. This study protocol was reviewed and approved by the Ethical Research Committee of Mae Fah Luang University, approval number COE 042/2022.
Acknowledgment
All authors would like to thank the school of anti-aging and regenerative medicine, Mae Fah Luang University, for its research facilities.
Funding
This study did not receive any funding.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Paichitrojjana A. Demodex: the worst enemies are the ones that used to be friends. Dermatol Rep. 2022. doi:10.4081/dr.2022.9339
2. Rather PA, Hassan I. Human Demodex mite: the versatile mite of dermatological importance. Indian J Dermatol. 2014;59(1):60–66. doi:10.4103/0019-5154.123498
3. Chang YS, Huang YC. Role of Demodex mite infestation in rosacea: a systematic review and meta-analysis. J Am Acad Dermatol. 2017;77(3):441–447.e6. doi:10.1016/j.jaad.2017.03.040
4. Foley R, Kelly P, Gatault S, Powell F. Demodex: a skin resident in man and his best friend. J Eur Acad Dermatol Venereol. 2021;35(1):62–72. doi:10.1111/jdv.16461
5. Erbagˇci Z, Özgöztaşi O. The significance of Demodex folliculorum density in rosacea. Int J Dermatol. 1998;37(6):421–425. doi:10.1046/j.1365-4362.1998.00218.x
6. Kligman AM, Christensen MS. Demodex folliculorum: requirements for understanding its role in human skin disease. J Invest Dermatol. 2011;131:8–10. doi:10.1038/jid.2010.335
7. Forton F, Seys B. Density of Demodex folliculorum in rosacea: a case-control study using standardized skin-surface biopsy. Br J Dermatol. 1993;128:650–659. doi:10.1111/j.1365-2133.1993.tb00261.x
8. Marks R, Dawber RP. Skin surface biopsy: an improved technique for the examination of the horny layer. Br J Dermatol. 1971;84(2):117–123. doi:10.1111/j.1365-2133.1971.tb06853.x
9. Aşkin U, Seçkin D. Comparison of the two techniques for measurement of the density of Demodex folliculorum: standardized skin surface biopsy and direct microscopic examination. Br J Dermatol. 2010;162(5):1124–1126. doi:10.1111/j.1365-2133.2010.09645.x
10. Jacob S, VanDaele MA, Brown JN. Treatment of Demodex-associated inflammatory skin conditions: a systematic review. Dermatol Ther. 2019;32(6):
11. Forton FMN. The pathogenic role of Demodex mites in rosacea: a potential therapeutic target already in erythematotelangiectatic rosacea? Dermatol Ther. 2020;10(6):1229–1253. doi:10.1007/s13555-020-00458-9
12. Raoufinejad K, Mansouri P, Rajabi M, Naraghi Z, Jebraeili R. Efficacy and safety of permethrin 5% topical gel vs. placebo for rosacea: a double-blind randomized controlled clinical trial. J Eur Acad Dermatol Venereol. 2016;30(12):2105–2117. doi:10.1111/jdv.13801
13. Sarac G. A comparison of the efficacy and tolerability of topical agents used in facial Demodex treatment. J Cosmet Dermatol. 2019;18(6):1784–1787. doi:10.1111/jdv.13801
14. Trave I, Merlo G, Cozzani E, Parodi A. Real-life experience on effectiveness and tolerability of topical ivermectin in papulopustular rosacea and antiparasitic effect on Demodex mites. Dermatol Ther. 2019;32(6):e13093. doi:10.1111/dth.13093
15. Schaller M, Gonser L, Belge K, et al. Dual anti-inflammatory and anti-parasitic action of topical ivermectin 1% in papulopustular rosacea. J Eur Acad Dermatol Venereol. 2017;31(11):1907–1911. doi:10.1111/jdv.14437
16. Forton FMN, De Maertelaer V. Effectiveness of benzyl benzoate treatment on clinical symptoms and Demodex density over time in patients with rosacea and demodicosis: a real life retrospective follow-up study comparing low- and high-dose regimens. J Dermatolog Treat. 2022;33:456–465. doi:10.1080/09546634.2020.1770168
17. Heukelbach J, Feldmeier H. Ectoparasites–the underestimated realm. Lancet. 2004;363(9412):889–891. doi:10.1016/S0140-6736(04)15738-3
18. Gunning K, Kiraly B, Pippitt K. Lice and scabies: treatment update. Am Fam Physician. 2019;99(10):635–642.
19. Khalil S, Abbas O, Kibbi AG, Kurban M. Scabies in the age of increasing drug resistance. PLoS Negl Trop Dis. 2017;11(11):e0005920. doi:10.1371/journal.pntd.0005920
20. Chen-Hussey V, Behrens R, Logan JG. Assessment of methods used to determine the safety of the topical insect repellent N,N-diethyl-m-toluamide (DEET). Parasit Vectors. 2014;7:173. doi:10.1186/1756-3305-7-173
21. Haleem ZM, Yadav S, Cushion ML, Tanner RJ, Carek PJ, Mainous AG. Exposure to N,N-Diethyl-Meta-Toluamide insect repellent and human health markers: population based estimates from the national health and nutrition examination survey. Am J Trop Med Hyg. 2020;103(2):812–814. doi:10.4269/ajtmh.20-0226
22. Fang F, Bernigaud C, Candy K, et al. Efficacy assessment of biocides or repellents for the control of Sarcoptes scabiei in the environment. Parasit Vectors. 2015;8:416. doi:10.1186/s13071-015-1027-7
23. Manjhi PK, Sinha RI, Kumar M, Sinha KI. Comparative study of efficacy of oral ivermectin versus some topical antiscabies drugs in the treatment of scabies. J Clin Diagn Res. 2014;8(9):HC01–HC04. doi:10.7860/JCDR/2014/9092.4878
24. Liu JX, Sun YH, Li CP. Volatile oils of Chinese crude medicines exhibit anti-parasitic activity against human Demodex with no adverse effects in vivo. Exp Ther Med. 2015;9(4):1304–1308. doi:10.3892/etm.2015.2272
25. Zhao Y, Guo N. The pesticidal effect and mechanism of peppermint oil in vitro against Demodex. Chin Bull Entomol. 2007;44(1):74–77.
26. Song B, Liu J, Liu T. Effect of galangal essential oil on killing human Demodex in vitro. J Path Biol. 2010;5(2):155–160.
27. Yurekli A, Botsali A. The comparative in vitro killing activity of tea tree oil versus permethrin on Demodex folliculorum of rosacea patients. J Cosmet Dermatol. 2022;21:2268–2272. doi:10.1111/jocd.14701
28. Diaz JH. Wilderness chemical and plant-based insect repellents: efficacy, safety, and toxicity. Environ Med. 2016;27(1):153–163. doi:10.1016/j.wem.2015.11.007
29. Licciardi S, Herve JP, Darriet F, Hougard JM, Corbel V. Lethal and behavioural effects of three synthetic repellents (DEET, IR3535 and KBR 3023) on Aedes aegypti mosquitoes in laboratory assays. Med Vet Entomol. 2006;20(3):288–293. doi:10.1111/j.1365-2915.2006.00630.x
30. Faulde MK, Albiez G, Nehring O. Insecticidal, acaricidal and repellent effects of DEET- and IR3535-impregnated bed nets using a novel long-lasting polymer-coating technique. Parasitol Res. 2010;106(4):957–965. doi:10.1007/s00436-010-1749-6
31. Dickens JC, Bohbot JD. Mini review: mode of action of mosquito repellents. Pestic Biochem Physiol. 2013;106:149–155. doi:10.1016/j.pestbp.2013.02.006
32. Swale DR, Sun B, Tong F, Bloomquist JR. Neurotoxicity and mode of action of N, N-diethyl-meta-toluamide (DEET). PLoS One. 2014;9(8):e103713. doi:10.1371/journal.pone.0103713
33. U.S. Environmental Protection Agency. Reregistration eligibility decision DEET. Washington DC, USA: United States Environmental Protection Agency Office of Pesticide Programs Special Review and Reregistration Division; 1998. EPA738-R-98–010:1–118. Available from: http:==www.epa.gov=oppsrrd1=REDs=0002red.pdf.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
