Back to Journals » OncoTargets and Therapy » Volume 11
Comparison of efficacy and toxicity between nedaplatin and cisplatin in treating malignant pleural effusion
Authors Zhong LZ, Xu HY, Zhao ZM, Zhang GM, Lin FW
Received 16 March 2018
Accepted for publication 24 May 2018
Published 5 September 2018 Volume 2018:11 Pages 5509—5512
DOI https://doi.org/10.2147/OTT.S168391
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Carlos E Vigil
Li-Zhe Zhong,1 Hong-Yan Xu,2 Zhong-Min Zhao,3 Guang-Mei Zhang,2 Feng-Wu Lin4
1Department of Cardiothoracic Surgery, Affiliated Hospital of Beihua University, Jilin, China; 2Department of Medical Oncology, The Second Hospital of Jilin, Jilin, China; 3Department of Pain, Jilin City Central Hospital, Jilin, China; 4Department of Thoracic Surgery, China-Japan Union Hospital of Jilin University, Changchun, China
Objective: To evaluate the efficacy and safety of nedaplatin versus cisplatin in treating malignant pleural effusion (MPE) caused by cancers.
Methods: The clinical data of 219 MPE patients treated from January 2013 to December 2016 were retrospectively reviewed. Intrapleural infusion with nedaplatin 80 mg/m2 (n=110) or with cisplatin 40 mg/m2 (n=109) were used as the treatment.
Results: There was no significant difference in the overall response rate between the nedaplatin group (62.73%) and the cisplatin group (54.13%) (P=0.154). The nedaplatin group had significantly lower rates of gastrointestinal side effects and significantly less incidence of increased serum creatinine levels in comparison with the cisplatin group. The overall rate of toxicity in the nedaplatin group (40.00%) was significantly lower than in the cisplatin group (78.90%) (P<0.001).
Conclusion: The efficacy of pleural perfusion with nedaplatin is noninferior to cisplatin in treating malignancy-induced MPE. Nedaplatin is associated with less toxicity in comparison with cisplatin.
Keywords: malignant pleural effusion, pleural perfusion, platinum-based drug, toxicity
Introduction
Malignant pleural effusion (MPE) is a common complication in patients with advanced malignancies. This condition can severely compromise heart and lung functions, and significantly decrease the quality of life in patients. Due to its poor response to systemic treatment, MPE is usually managed with intrapleural perfusion chemotherapy. Cisplatin and carboplatin are the mostly used drugs in treating MPE, and their efficacy is well-established. However, these 2 drugs are associated with gastrointestinal side effects and myelosuppression, which has limited their clinical use.1–4
Nedaplatin is a second-generation platinum-based drug. The present study aimed to investigate the efficacy and toxicity of nedaplatin versus cisplatin in treating MPE caused by malignant tumors.
Materials and methods
Patients
The clinical data of 219 consecutive patients with MPE caused by malignant tumors were retrospectively reviewed. These patients were treated from January 2013 to December 2016 at our hospital. There were 114 males and 105 females with a mean age of 52 years (age range, 28–77 years). Our study was approved by the ethics committee of China–Japan Union Hospital of Jilin University. Patient consent to review their medical records was not required by the institutional review board because the review of the patient data was anonymous.
Intrapleural perfusion
The location of pleural effusion was identified using ultrasonography. A central venous catheter was inserted under ultrasound guidance. The pleural fluid was drained for 3–5 days at a rate of 800–2,000 mL/d. Albumin was infused in the meantime. One hundred and ten patients received intrapleural infusion with nedaplatin 80 mg/m2 in 50 mL normal saline, and 109 patients received intrapleural infusion with cisplatin 40 mg/m2 in 50 mL normal saline. Granisetron 5 mg was used 30 min prior to the intrapleural infusion for antiemetic purpose. The patient was instructed to change body position every 10 min after the intrapleural infusion for 1 hr to disperse the drug in the pleural cavity. Drainage was resumed after 72 h and was performed weekly for at least 2 consecutive weeks.
Evaluation of efficacy
Complete remission was a complete disappearance of the pleural effusion for 4 consecutive weeks. Partial remission was a reduction in the pleural effusion ≥50% accompanied by symptom improvement ≥4 weeks. Progressive disease was an increase in the pleural effusion >25%. Stable disease was a reduction in the pleural effusion <50% or an increase <25%. Overall response rate was the sum of complete remission rate and partial remission rate. Treatment-associated toxicity was evaluated using the World Health Organization anticancer drug toxicity criteria.
Statistical analysis
The continuous data are presented as mean ± standard deviation. The normally distributed data were compared using the paired sample t-test, and the nonnormally distributed data were compared using the Wilcoxon 2-sample test. The categorical data were presented as frequencies or percentages and compared using the Fisher’s exact test. Efficacy and adverse events were compared using the Cochran–Mantel–Haenszel test. All statistical analyses were performed using the SAS 9.3 software (SAS Institute Inc., Cary, NC, USA). A P-value <0.05 was considered statistically significant.
Results
Patients’ general information
All patients had an ECOG score ≤3 and a medium or large volume of intrapleural fluid evaluated as assessed using ultrasound. The underlying malignancy included 115 cases of lung cancer, 52 cases of breast cancer, and 52 cases of gastrointestinal cancer. Systemic chemotherapy was administered 6 months earlier in 162 patients, within 1 month in 39 patients, and concomitantly with the intrapleural perfusion treatment in 18 patients.
The cisplatin group and the nedaplatin group were not significantly different with regard to gender, age, body mass index, diabetes, and cardiovascular disease (Table 1). The 2 groups also did not differ significantly in Karnofsky score, underlying malignancy, tumor pathology, mediastinal metastasis, and pleural effusion volume (Table 2).
  | Table 1 General characteristics of the patients |
  | Table 2 Comparison of the underlying diseases between the 2 groups |
Efficacy and toxicity
The overall response rate of the MPE treatment was 62.73% in the nedaplatin group versus 54.13% in the cisplatin group, which was not significantly different (P=0.154). The 2 drugs also did not differ significantly in MPE treatment efficacy in patients with lung cancer, other cancers, or any cancer (Table 3).
The nedaplatin group had significantly lower rates of gastrointestinal side effects and significantly less incidence of increased serum creatinine levels in comparison with the cisplatin group (Table 4). The overall rate of toxicity in the nedaplatin group (40.00%) was significantly lower than that in the cisplatin group (78.90%). These results suggested that nedaplatin is superior to cisplatin in toxicity in the treatment of MPE.
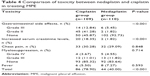  | Table 4 Comparison of toxicity between nedaplatin and cisplatin in treating MPE |
Discussion
MPE is commonly seen in patients with end-stage tumors when the pleural cavity is involved. Normally, 3–15 mL fluid is present in the pleural cavity and functions as lubricant. About 500–1,000 mL pleural fluid is secreted and absorbed daily, to maintain a dynamic balance. Malignant diseases may disrupt this balance and cause MPE. Excessive pleural fluid can severely affect patient breathing, and even result in apnea. Effective control of MPE is essential for improving the quality of life of patients with end-stage disease. Surgical pleurodesis is available for the management of MPE but is not popular in practice due to its traumatic nature.5,6 Conservative treatment is usually preferred to treat MPE, which consists of pleural effusion drainage as the first step and intrapleural perfusion with drugs as the second step. The drugs for intrapleural perfusion include chemotherapeutic agents or immunosuppressants, or the both in combination.4,7,8 Intrapleural perfusion with chemotherapeutic agents causes pleural adhesion, reduces pleural permeability, and decreases pleural effusion. In addition, cytotoxicity of the chemotherapeutic agents also helps control the intrapleural metastasis.9
Nedaplatin has been approved in Japan for the treatment of various solid tumors of the esophagus, ovary, cervix, bladder, lung, and head and neck.10 Nedaplatin has the same therapeutic mechanisms as cisplatin but is 10 times more water-soluble than cisplatin. Due to its lower gastrointestinal side effects and renal toxicity in comparison with cisplatin, nedaplatin is being used increasingly in chemotherapy.
Nedaplatin was used in the present study as an intrapleural perfusion drug for the treatment of MPE. Because nedaplatin is not metabolized by the liver, it can maintain a high concentration in the pleural fluid, and constantly kills the tumor cells in the pleural membrane and fluid.
The present study found that the overall response rate of the nedaplatin group was 62.73%, which was not significantly different from the 54.13% overall response rate in the cisplatin group. The 2 drugs also did not differ significantly in MPE treatment efficacy in patients with lung cancer, breast cancer, or gastrointestinal cancer. However, nedaplatin was associated with significantly lower rates of gastrointestinal side effects and significantly less incidence of increased serum creatinine levels in comparison with cisplatin, suggesting that nedaplatin is superior to cisplatin in toxicity in the treatment of MPE. These results were consistent with previous findings that nedaplatin is superior to cisplatin in toxicity.11–15 Less toxicity means better tolerability and better patient compliance, which can help to achieve better treatment efficacy.
The present study has some limitations. First, this was a retrospective study and the patient selection and treatment assignment might be affected by confounding factors. Second, the sample size was relatively small. Third, the patient survival results were not available for the analysis.
Conclusion
In conclusion, the efficacy of pleural perfusion with nedaplatin was found to be noninferior to cisplatin in treating malignancy-induced MPE. Nedaplatin is associated with less toxicity in comparison with cisplatin. These results need further confirmation with well-designed prospective studies.
Acknowledgment
Li-Zhe Zhong and Hong-Yan Xu are co-first authors for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
Jiang L, Li P, Gong Z, et al. Effective treatment for malignant pleural effusion and ascites with combined therapy of bevacizumab and cisplatin. Anticancer Res. 2016;36(3):1313–1318. | ||
Masters GA, Argiris AE, Hahn EA, et al. A randomized phase II trial using two different treatment schedules of gemcitabine and carboplatin in patients with advanced non-small-cell lung cancer. J Thorac Oncol. 2006;1(1):19–24. | ||
Miller AA, Case D, Atkins JN, Giguere JK, Bearden JD. Phase II study of carboplatin, irinotecan, and thalidomide in patients with advanced non-small cell lung cancer. J Thorac Oncol. 2006;1(8):832–836. | ||
Sakaguchi H, Ishida H, Nitanda H, Yamazaki N, Kaneko K, Kobayashi K. Pharmacokinetic evaluation of intrapleural perfusion with hyperthermic chemotherapy using cisplatin in patients with malignant pleural effusion. Lung Cancer. 2017;104:70–74. | ||
Fysh ET, Tan SK, Read CA, et al. Pleurodesis outcome in malignant pleural mesothelioma. Thorax. 2013;68(6):594–596. | ||
Marrazzo A, Noto A, Casa L, et al. Video-thoracoscopic surgical pleurodesis in the management of malignant pleural effusion: the importance of an early intervention. J Pain Symptom Manage. 2005;30(1):75–79. | ||
Feng X, Zhu L, Xiong X, et al. Therapeutical effect of intrapleural perfusion with hyperthermic chemotherapy on malignant pleural effusion under video-assisted thoracoscopic surgery. Int J Hyperthermia. 2018;34(4):1–7. | ||
Hu R, Jiang H, Li H, Wei D, Wang G, Ma S. Intrapleural perfusion thermo-chemotherapy for pleural effusion caused by lung carcinoma under VATS. J Thorac Dis. 2017;9(5):1317–1321. | ||
Desoize B, Madoulet C. Particular aspects of platinum compounds used at present in cancer treatment. Crit Rev Oncol Hematol. 2002;42(3):317–325. | ||
Dilruba S, Kalayda GV. Platinum-based drugs: past, present and future. Cancer Chemother Pharmacol. 2016;77(6):1103–1124. | ||
Liu Y, Yu S, Liu S, et al. Comparison of nedaplatin-based versus cisplatin-based chemotherapy for advanced non-small cell lung cancer among East Asian populations: a meta-analysis. Sci Rep. 2015;5:10516. | ||
Pang H, Feng T, Lu H, et al. Efficacy and safety of nedaplatin in advanced breast cancer therapy. Cancer Invest. 2016;34(4):167–172. | ||
Shan J, Xiong Y, Wang D, et al. Nedaplatin-versus cisplatin-based chemotherapy in the survival time of patients with non-small cell lung cancer. Mol Clin Oncol. 2015;3(3):543–549. | ||
Tang C, Wu F, Wang R, et al. Comparison between nedaplatin and cisplatin plus docetaxel combined with intensity-modulated radiotherapy for locoregionally advanced nasopharyngeal carcinoma: a multicenter randomized phase II clinical trial. Am J Cancer Res. 2016;6(9):2064–2075. | ||
Zhang F, Wang Y, Wang ZQ, et al. Efficacy and safety of cisplatin-based versus nedaplatin-based regimens for the treatment of metastatic/recurrent and advanced esophageal squamous cell carcinoma: a systematic review and meta-analysis. Dis Esophagus. 2017;30(2):1–8. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

