Back to Journals » Journal of Pain Research » Volume 13
Comparison of Effectiveness of Ropivacaine Infusion Regimens for Continuous Femoral Nerve Block for Recovery After Total Knee Arthroplasty: A Randomized Double-Blind Trial
Authors Zhang Y, Liu L, Zheng L, Chen J, Huang L, Wang Q, Shi K
Received 24 January 2020
Accepted for publication 27 March 2020
Published 12 May 2020 Volume 2020:13 Pages 997—1005
DOI https://doi.org/10.2147/JPR.S247158
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Robert B. Raffa
Yujian Zhang,* Le Liu,* Liangyu Zheng, Jiali Chen, Lvdan Huang, Quanguang Wang, Kejian Shi
Department of Anesthesiology, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, Zhejiang, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Kejian Shi; Quanguang Wang
Department of Anesthesiology, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, Zhejiang, People’s Republic of China
Tel +86 13868889697
; +86 13736935500
Fax +86 57755578999+669697
; +86 57755578999+655500
Email [email protected]; [email protected]
Purpose: Continuous femoral nerve block (cFNB) is effective for analgesia after total knee arthroplasty (TKA). However, it is not clear which low-dose regimen of ropivacaine infusion for cFNB provides adequate analgesia and enables rapid recovery. The aim of this study was to compare the effects of different cFNB regimens on rehabilitation of patients after TKA.
Patients and Methods: Sixty patients scheduled for TKA were enrolled in this trial. After surgery, patients in the 0.1%, 0.15%, and 0.2% groups received infusion of 10 mL of 0.1%, 6.7 mL of 0.15%, and 5 mL of 0.2% ropivacaine per hour, respectively (n=20), at the dose of 10 mg/h for 48 h. The primary endpoint was time to readiness for discharge. The secondary endpoints were time to first walk, manual muscle testing (MMT) scores, numerical rating scale (NRS) scores at rest and movement, morphine consumption, rescue analgesia, and the incidence of adverse events.
Results: The time to readiness for discharge and the time to first walk of the 0.1% group were significantly longer than that of the 0.15% and 0.2% groups. MMT scores of the 0.2% group at 18 h after surgery were significantly lower than those of the 0.1% group. MMT scores of the 0.2% group at 24 and 48 h after surgery were also significantly lower than those of the 0.1% and 0.15% groups. NRS scores at rest and at movement in the 0.1% group were significantly higher than those in the 0.15% and 0.2% groups.
Conclusion: Patients administered the regimens of 0.15% and 0.2% ropivacaine infusion for cFNB were ready for discharge earlier than the 0.1% group after TKA, at the dose of 10 mg/h for 48 h. The regimen of 0.15% ropivacaine, which is associated with less quadriceps muscle strength weakness than 0.2%, is recommended for postoperative analgesia after TKA.
Keywords: analgesia, ultrasound, regional anesthesia, quadriceps muscle strength
Introduction
With the aging of the population, the incidence of total knee arthroplasty (TKA) has increased rapidly as an intervention to achieve functional restoration and improve quality of life dramatically.1 However, patients may suffer severe postoperative pain after TKA, which may affect postoperative recovery. Regional anesthesia is effective for providing postoperative analgesia after TKA. In particular, multimodal analgesia in combination with regional anesthesia is beneficial for early functional exercise to promote postoperative rehabilitation and reduce the risk of postoperative complications.2,3
Postoperative rehabilitation of TKA involves pain management and functional exercise, and therefore dependence on analgesics, in order to promote patient recovery. Although continuous femoral nerve block (cFNB) relieves pain and reduces dependence on analgesics, and is considered the gold standard for analgesia after TKA,4 mitigation of the effect of cFNB on quadriceps muscle strength remains a challenge. Previous studies have shown that the use of 0.2% ropivacaine5–7 at a relatively large dose of 10–20 mg/h5–10 for cFNB resulted in reduction in quadriceps muscle strength. Other studies have shown that the effectiveness of cFNB is not altered as a result of changes to the concentration and volume of ropivacaine at a fixed dose of 12 mg/h.9,10 But the total amount of ropivacaine administered likely plays the most significant role in determining the quadriceps muscle strength of cFNB. The continuous infusion of low-dose local anesthetic for cFNB may represent an optimal regimen of to improve the effect of postoperative analgesia and enable early functional exercise after TKA, with adequate provision of analgesia and reduced quadriceps muscle weakness.
The present trial was designed to compare the effectiveness of different regimens of 0.1%, 0.15%, and 0.2% of ropivacaine, at the fixed dose of 10 mg/h, for cFNB for postoperative analgesia in patients undergoing TKA. The primary endpoint was time to readiness for discharge. The secondary endpoints were time to first walk, manual muscle testing (MMT) scores, numerical rating scale (NRS) scores at rest and movement, morphine consumption, rescue analgesia, and the incidence of adverse events.
Patients and Methods
This randomized double-blind trial was approved by the Ethics Committee of The First Affiliated Hospital of Wenzhou Medical University (No. 119, 2017). Written informed consent was obtained from all participants. The trial was registered prior to patient enrollment at the Chinese Clinical Trial Registry (ChiCTR-IOD-17012678).
Enrollment
Inclusion criteria included age between 40 and 80 years, American Society of Anesthesiologists (ASA) physical status score of I or II, and body mass index (BMI) between 18.5 and 40 kg/m2, undergoing TKA, and willingness to receive cFNB for analgesia. Exclusion criteria included allergy to ropivacaine or other drugs used in this trial, a history of opioid abuse or analgesic dependence, peripheral neuropathy, current chronic pain treatment, or pregnancy. Sixty patients scheduled for TKA were enrolled in this randomized double-blind Trial. A CONSORT checklist was used for patient enrollment and allocation (Figure 1). Patients were randomized into three groups: 0.1% group, 0.15% group, and 0.2% group (n=20 per group) according to a random number table generated using SPSS 22.0 statistical software (IBM Corporation, Armonk, NY, USA).
 |
Figure 1 CONSORT flow diagram. |
Regional Anesthesia
An ultrasound-guided femoral nerve block was performed in the preoperative preparation room, prior to surgery, by an attending anesthesiologist, who was blinded to patient grouping and was not involved in follow-up assessments. Midazolam (1 mg) and fentanyl (50μg) were intravenously administered for sedation and analgesia, respectively. After routine disinfection and towel draping, a high-frequency (6–12 MHz) linear probe (SonoSite X-Porte; SonoSite Inc., Bothell, WA, USA) was used to locate the femoral artery and femoral nerve in the inguinal area. After local infiltration with 1% lidocaine, a needle was inserted using longitudinal and in-plane technique toward the femoral nerve, and a catheter (PlexoLong NanoLine acc. Meier, Facet 19G×50 mm, PAJUNK®, The Germany) was advanced through the needle to a distance of 2–3 cm beyond the needle tip. The location was confirmed by injecting 1–2 mL of saline under ultrasound; then, the catheter was secured. The femoral nerve block was established with an initial bolus of 20 mL of 0.25% ropivacaine (LBKL; AstraZeneca AB, Sweden).
Intraoperative Management
The surgeries were completed under general anesthesia by anesthesiologists who were not involved in the study and blinded to grouping. Propofol (1.5–2.5 mg/kg), sufentanil (0.3μg/kg), and cis-atracurium (0.15 mg/kg) were used for induction, and a laryngeal mask was used to control the airway during surgery. Anesthesia was maintained using propofol (2–6 mg·kg−1·h−1), remifentanil (0.1–0.2 μg·kg−1·min−1), and sevoflurane (1–2% in oxygen), and the bispectral index value was maintained at 40–60. Tropisetron (5 mg) was intravenously administered about 30 min before the end of surgery.
Postoperative Analgesia
After surgery, all patients were transferred to the post-anesthesia care unit. A patient-controlled analgesia pump (ZZB-I automatic injection pump driver; Nantong Aipu Medical Instrument Co., Ltd., Nantong, China) was connected to the catheter and initiated for cFNB with different regimens of ropivacaine infusion. The pump screens were covered with tape. Patients in the 0.1% group, 0.15% group, and 0.2% group received infusion of 10 mL 0.1% ropivacaine, 6.7 mL 0.15% ropivacaine, and 5 mL 0.2% ropivacaine per hour, respectively, with a total dosage of 10 mg ropivacaine per hour. Another patient-controlled analgesia pump containing 50 mg of morphine, diluted with saline to a volume of 100 mL, was placed with venous access and programmed to deliver a bolus dose of 1 mg of morphine when NRS scores >3, without background infusion, with a lockout of 3 minutes and a limit of 10 mg/h.
Medications used for the multimodal analgesia protocol included celecoxib (200 mg every 12 h for 3 days) and tramadol (100 mg every day for 5 days). If NRS scores exceeded 4 points, patients were administered intramuscularly injected bucinnazine (100 mg) for rescue analgesia.
Data Collection
Demographic characteristics including age and sex, as well as BMI, ASA classification, and surgery duration were recorded by an investigator who did not participate in postoperative evaluations and record-keeping. Follow-up and evaluation were performed at 6 h, 18 h, and 24 h, 48 h and at 14:00 on day 3, day 4, and day 5 after surgery by another investigator. All patients performed functional rehabilitation exercise after surgery and were encouraged to ambulate as soon as possible. At each evaluation, patients were asked to provide NRS scores ranging from 0 to 10 both at rest and on movement (0 = no pain, 10 = worst imaginable pain). Manual muscle testing (MMT) scores were also evaluated and recorded (the grading was recorded from 0 to 5), with patients in the sitting position and knee extended against gravity from the flexed position.11 After physical therapy, each of the three discharge criteria12 (adequate analgesia (NRS score <4), independence from intravenous opioids or rescue analgesia in the previous 12 h, and ambulation of at least 30 m) were evaluated, and the time in which the three discharge criteria were met was defined as time to readiness for discharge. The time to first walk, morphine consumption, cases of rescue analgesia, nausea and vomiting, peripheral nerve injury, or other adverse event were recorded.
Statistical Analysis
All data were analyzed using SPSS 22.0 statistical software. The Shapiro–Wilk test was used for normal distribution analysis. Measured normally distributed data were expressed as mean (standard deviation), and non-normally distributed data were expressed as median (interquartile range). Frequencies were used in categorical variables.
The NRS scores at rest and on movement were analyzed by two-way repeated-measures analysis. Age, BMI, surgical duration, and morphine consumption were analyzed using one-way analyses of variance. The post hoc Bonferroni test was used for multiple two-group comparisons. Time to readiness for discharge and time to first walk were plotted as Kaplan–Meier survival curves and compared using the Log-rank tests. Sex, ASA classification, and case of rescue analgesia were determined using chi-square tests or Fisher’s exact tests, as appropriate. Statistical significance was considered to be indicated by P<0.05. MMT scores were compared using Kruskal–Wallis H-tests, and multiple testing was performed using Mann–Whitney U-tests. To reduce type I error, P<0.017 was considered to represent statistically significant data.
Sample Size Calculation
The primary endpoint was the time to readiness for discharge. In the preliminary study, 15 patients were assigned to 0.1% group, 0.15% group, and 0.2% group (n=5), and the time to readiness for discharge was 4.4±0.89, 3.2±0.83, and3.8±1.10 days, respectively. A sample size of 15 per group was obtained using PASS 11.0 (NCSS Statistical Software, Kaysville, UT, USA) with α=0.05 and β=0.1. We planned to recruit 20 patients per group considering the loss potential and errors.
Results
There were no statistically significant differences in age, sex, BMI, ASA classification, or surgery duration between the three groups (P>0.05) (Table 1).
 |
Table 1 Demographic and Intraoperative Characteristics |
Time to Readiness for Discharge
The median of time to readiness for discharge was 5 (4–5) days, 3 (3–4) days, and 4 (3–4.75) days in the 0.1% group, 0.15% group, and 0.2% group, respectively. The time to readiness for discharge of the 0.1% group was significantly longer than that of the 0.15% and 0.2% groups (P=0.003 and P=0.012). Kaplan–Meier curves demonstrated earlier readiness for discharge (Figure 2A) among patients in the 0.15% group and 0.2% group than that in 0.1% group (P=0.005 and P=0.001).
Time to First Walk
The median of time to first walk was 4 (3–5) days, 2 (2–3) days, and 2 (2–3) days in the 0.1% group, 0.15% group, and 0.2% group, respectively. The time to first walk of the 0.1% group was significantly longer than that of 0.15% and 0.2% groups (P<0.001 and P=0.001). Kaplan–Meier curves demonstrated earlier walking (Figure 2B) among patients in the 0.15% group and 0.2% group than among those in the 0.1% group (P=0.002 and P=0.004).
Manual Muscle Testing
MMT scores for the three groups are shown in Figure 3. MMT scores of the 0.2% group at 18 h after surgery were significantly lower than those of the 0.1% group (P<0.001). MMT scores of the 0.2% group at 24 and 48 h after surgery were also significantly lower than those of the 0.1% and 0.15% group (P=0.001, P=0.006, at 24 h after surgery; both P<0.001, at 48 h after surgery).
Pain Scores
NRS scores at rest and on movement are shown in Figure 4. The 0.1% group had significantly higher NRS scores at rest and at movement after TKA than the 0.15% group and the 0.2% group (P<0.001 and P<0.001 at rest; P=0.005 and P=0.009 at movement).
Postoperative Morphine Consumption and Rescue Analgesia
Morphine consumption among the three groups over 48 h is shown in Table 2. There were no significant differences between the three groups in terms of morphine consumption over 48 h (P=0.309), as shown in Table 2. Although the cases of rescue analgesia in the 0.1% group were more frequent than in the 0.15% and 0.2% groups (7, 2, and 3, respectively), there was no significant difference between the three groups (P=0.116) (Table 2).
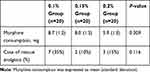 |
Table 2 Morphine Consumption and Cases of Rescue Analgesia |
Adverse Events
The incidence rates of nausea and vomiting were 6 (30%), 4 (20%), and 4 (20%), in the 0.1% group, 0.15% group, and 0.2% group, respectively (P=0.918). No other adverse effects were observed in the three groups.
Discussion
The results of this study showed that, although patients with cFNB achieved satisfactory analgesic effects during infusion with 0.1%, 0.15%, and 0.2% ropivacaine at a dose of 10 mg/h over 48 h after surgery, pain recurred in patients in the 0.1% group when ropivacaine infusion was stopped. The time to readiness for discharge and time to first walk was significantly earlier in the 0.15% and 0.2% groups than in the 0.1% group. In consideration of the lower MMT scores of the 0.2% group relative to the 0.15% group at 24 and 48 h after surgery, the regimen of 0.15% ropivacaine at 10 mg/h for cFNB is recommended for postoperative analgesia after TKA.
The most optimal regimen for local anesthetic infusion for cFNB remains elusive; furthermore, the administration method and dose of local anesthetic used differ between studies. Studies have shown that although 0.2% ropivacaine provides satisfactory analgesia after TKA, quadriceps muscle weakness following a larger dose at 10–20mg/h has also reported.5–8 Bauer et al reported similar analgesic effects of 0.1% and 0.4% ropivacaine for cFNB at the dose of 12 mg/h, suggesting that the dose of local anesthetic is the primary determinant of perineural infusion effects.10 In contrast, Brodner et al demonstrated that 0.1% ropivacaine for cFNB provided ineffective analgesia under the base dose of 10 mg/h, even with frequent infusion adjustments.13 The variation in the results between the two studies may be attributable to differences in trial design. In this study, almost all of the NRS scores at rest were lower than or equal to three; therefore, despite the statistical differences, there were no clinical differences. Adequate analgesia was achieved at a dose of 10 mg/h when ropivacaine infusion was implemented. The NRS scores in 0.1% group at movement were significantly higher than the 0.15% and 0.2% groups, especially rebounded at the third to fifth days after TKA and cFNB infusion was ceased. The reasons for this observation may be that a relatively larger amount (10 mL/h) of local anesthetic was absorbed, not only by the femoral nerve but also surrounding tissues, compared with that for the 6.7 mL/h dose in the 0.15% group and 5 mL/h in the 0.2% group. Additionally, the sensory perception in the 0.1% group may have recovered earlier than that for patients in the 0.15% and 0.2% groups after infusion was stopped. Therefore, at the dose of 10 mg/h, the ropivacaine concentration of 0.1% is not recommended for cFNB owing to the inadequate analgesic effect.
Pain, mobility, or muscle strength are generally used as measures for the assessment of cFNB after TKA, but the three measures are used independently of each other. The time to readiness for discharge, with three discharge criteria (adequate analgesia, independence from opioids, and ambulation of at least 30 m) offer a more comprehensive assessment of rehabilitation reflecting the effect of TKA.6,14,15 In this study, the longer median time to readiness for discharge of patients in 0.1% group compared with that for the 0.15% and 0.2% groups may be attributed to the higher pain scores, lower MMT scores, and later ambulation. Although the MMT scores of the 0.2% group were lower than those of the 0.15% group, consistent with the findings of Yang et al,16 these scores mainly reflected the muscle strength in the first 2 days, which had little effect on the overall follow-up and may be attributed to the small sample size. Usually patients undergoing TKA have different degrees of arthrogenic muscle inhibition, so the MMT scores may not accurately reflect the degree of motor nerve block. However, it should be noted that the use of minimal concentrations of local anesthetics remains a strategy worthy of consideration. Patients with exacerbated pain refused to walk because of rebound pain, which may have affected postoperative training and caused patients to question the effectiveness of this training. Therefore, in this study, rebound pain may be the primary cause for delayed time to first walk. At the dose of 10 mg/h, the ropivacaine concentration of 0.15% is more strongly recommended for cFNB owing to the earlier time to readiness for discharge, shorter time to first walk, and less quadriceps muscle weakness achieved with this concentration.
Postoperative pain in TKA is not attributable to the surgery itself, but to postoperative functional exercise.17,18 Blockade of various steps of pain signaling pathways by combining various analgesics and analgesic methods is recommended.2 Therefore, consistent with other studies of postoperative analgesia after TKA, multimodal analgesia based on cFNB was used in this trial. Rescue analgesia relieves postoperative pain, but reflects the inadequate analgesia and delayed readiness for discharge. Although the cases of rescue analgesia in the 0.1% group was more than that in the 0.15% and 0.2% groups (7, 2, and 3, respectively), there was no significant difference; a larger sample size may be required to confirm this finding.
This study had several limitations: 1) The femoral nerve and sciatic nerve both innervate the knee joint from the anterior and posterior, respectively. In this study, we did not distinguish between anterior and posterior pain; it was also difficult for patients to distinguish between these two sources of pain. 2) Although the sample size calculation for the 60 patients was sufficient for the purposes of this study, future efforts should be aimed at carrying out multicenter studies with a larger sample size. 3) Volume is responsible for spread of local anesthetics and concentration is responsible for density of the block. In this study, the varying volume as the concentration varied also may affect the analgesia or quadriceps muscle strength.
Future Research
This study only evaluates the effect of a 10mg/h dose of ropivacaine concentration on cFNB. Future studies should aim to explore whether adjuvants such as dexmedetomidine, epinephrine, or dexamethasone allow for the reduction of the dose or concentration of local anesthetics. Although cFNB is the current gold standard for postoperative analgesia for TKA, adductor canal block is a recently developed technique that enables the retention of more muscle strength, but with relative poorer pain relief, than cFNB,11,19,20 which may affect postoperative rehabilitation. A randomized controlled trial comparing time to readiness for discharge between these two techniques is warranted.
Conclusion
Patients administered the regimens of 0.15% and 0.2% ropivacaine infusion for cFNB were ready for discharge earlier than the 0.1% group after TKA, at the dose of 10 mg/h for 48 h. The regimen of 0.15% ropivacaine, which is associated with less quadriceps muscle strength weakness than 0.2%, is recommended for postoperative analgesia after TKA.
Abbreviations
ASA, American Society of Anesthesiologists; BMI, body mass index; cFNB, continuous femoral nerve block; MMT, manual muscle testing; NRS, numerical rating scale; TKA, total knee arthroplasty.
Data Sharing Statement
The corresponding author ([email protected]) will be ready to send all related data for any authority on request by an email message. The data will be available this way for up to 6 months after the paper is published.
Ethical Statement
The authors declare that all patients gave written informed consent before initiation of the study protocol and was conducted in accordance with the Declaration of Helsinki. The study was approved by the Ethics Committee of The First Affiliated Hospital of Wenzhou Medical University (No. 119, 2017).
Author Contributions
All authors contributed to conception and design, acquisition and analysis of data, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This work is supported by the National Natural Science Foundation of China (Grant No. 81900231, Beijing, China), and by Wenzhou Science and Technology Bureau (Y20170645, Wenzhou, China).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Varacallo M, Luo TD, Johanson NA. Total Knee Arthroplasty (TKA) techniques. In: Johanson N, ed. StatPearls. Treasure Island (FL); 2019.
2. Elmallah RK, Chughtai M, Khlopas A, et al. Pain control in total knee arthroplasty. J Knee Surg. 2018;31(6):504–513. doi:10.1055/s-0037-1604152
3. Lewis GN, Rice DA, McNair PJ, Kluger M. Predictors of persistent pain after total knee arthroplasty: a systematic review and meta-analysis. Br J Anaesth. 2015;114(4):551–561. doi:10.1093/bja/aeu441
4. Hadzic A, Houle TT, Capdevila X, Ilfeld BM. Femoral nerve block for analgesia in patients having knee arthroplasty. Anesthesiology. 2010;113(5):1014–1015. doi:10.1097/ALN.0b013e3181f4b43d
5. Carli F, Clemente A, Asenjo JF, et al. Analgesia and functional outcome after total knee arthroplasty: periarticular infiltration vs continuous femoral nerve block. Br J Anaesth. 2010;105(2):185–195. doi:10.1093/bja/aeq112
6. Ilfeld BM, Le LT, Meyer RS, et al. Ambulatory continuous femoral nerve blocks decrease time to discharge readiness after tricompartment total knee arthroplasty: a randomized, triple-masked, placebo-controlled study. Anesthesiology. 2008;108(4):703–713. doi:10.1097/ALN.0b013e318167af46
7. Seet E, Leong WL, Yeo AS, Fook-Chong S. Effectiveness of 3-in-1 continuous femoral block of differing concentrations compared to patient controlled intravenous morphine for post total knee arthroplasty analgesia and knee rehabilitation. Anaesth Intensive Care. 2006;34(1):25–30. doi:10.1177/0310057X0603400110
8. Shum CF, Lo NN, Yeo SJ, Yang KY, Chong HC, Yeo SN. Continuous femoral nerve block in total knee arthroplasty: immediate and two-year outcomes. J Arthroplasty. 2009;24(2):204–209. doi:10.1016/j.arth.2007.09.014
9. Ilfeld BM, Moeller LK, Mariano ER, et al. Continuous peripheral nerve blocks: is local anesthetic dose the only factor, or do concentration and volume influence infusion effects as well? Anesthesiology. 2010;112(2):347–354. doi:10.1097/ALN.0b013e3181ca4e5d
10. Bauer M, Wang L, Onibonoje OK, et al. Continuous femoral nerve blocks: decreasing local anesthetic concentration to minimize quadriceps femoris weakness. Anesthesiology. 2012;116(3):665–672. doi:10.1097/ALN.0b013e3182475c35
11. Elkassabany NM, Antosh S, Ahmed M, et al. The risk of falls after total knee arthroplasty with the use of a femoral nerve block versus an adductor canal block: a double-blinded randomized controlled study. Anesth Analg. 2016;122(5):1696–1703. doi:10.1213/ANE.0000000000001237
12. Enloe LJ, Shields RK, Smith K, Leo K, Miller B. Total hip and knee replacement treatment programs: a report using consensus. J Orthop Sports Phys Ther. 1996;23(1):3–11. doi:10.2519/jospt.1996.23.1.3
13. Brodner G, Buerkle H, Van Aken H, et al. Postoperative analgesia after knee surgery: a comparison of three different concentrations of ropivacaine for continuous femoral nerve blockade. Anesth Analg. 2007;105(1):256–262. doi:10.1213/01.ane.0000265552.43299.2b
14. Machi AT, Sztain JF, Kormylo NJ, et al. Discharge readiness after tricompartment knee arthroplasty: adductor canal versus femoral continuous nerve blocks-A dual-center, randomized trial. Anesthesiology. 2015;123(2):444–456. doi:10.1097/ALN.0000000000000741
15. Sztain JF, Machi AT, Kormylo NJ, et al. Continuous adductor canal versus continuous femoral nerve blocks: relative effects on discharge readiness following unicompartment knee arthroplasty. Reg Anesth Pain Med. 2015;40(5):559–567. doi:10.1097/AAP.0000000000000279
16. Yang X, Kang W, Xiong W, et al. The effect of dexmedetomidine as adjuvant to ropivacaine 0.1% for femoral nerve block on strength of quadriceps muscle in patients undergoing total knee arthroplasty: a double-blinded randomized controlled trial. J Pain Res. 2019;12:3355–3363. doi:10.2147/JPR.S217283
17. Yu S, Dundon J, Solovyova O, Bosco J, Iorio R. Can multimodal pain management in TKA eliminate patient-controlled analgesia and femoral nerve blocks? Clin Orthop Relat Res. 2018;476(1):101–109. doi:10.1007/s11999.0000000000000018
18. Rice DA, Kluger MT, McNair PJ, et al. Persistent postoperative pain after total knee arthroplasty: a prospective cohort study of potential risk factors. Br J Anaesth. 2018;121(4):804–812. doi:10.1016/j.bja.2018.05.070
19. Ghodki PS, Shalu PS, Sardesai SP. Ultrasound-guided adductor canal block versus femoral nerve block for arthroscopic anterior cruciate ligament repair under general anesthesia. J Anaesthesiol Clin Pharmacol. 2018;34(2):242–246. doi:10.4103/joacp.JOACP_172_17
20. Kuang MJ, Ma JX, Fu L, He WW, Zhao J, Ma XL. Is adductor canal block better than femoral nerve block in primary total knee arthroplasty? A GRADE analysis of the evidence through a systematic review and meta-analysis. J Arthroplasty. 2017;32(10):3238–3248 e3233. doi:10.1016/j.arth.2017.05.015
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



