Back to Journals » Clinical Ophthalmology » Volume 15
Comparison of Early- and Late-Onset NMOSD-Related Optic Neuritis in Thai Patients: Clinical Characteristics and Long-Term Visual Outcomes
Authors Thongmee W , Narongkhananukul C, Padungkiatsagul T , Jindahra P, Vanikieti K
Received 8 December 2020
Accepted for publication 14 January 2021
Published 4 February 2021 Volume 2021:15 Pages 419—429
DOI https://doi.org/10.2147/OPTH.S295769
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Watcharaporn Thongmee,1 Chanomporn Narongkhananukul,1 Tanyatuth Padungkiatsagul,1 Panitha Jindahra,2 Kavin Vanikieti1
1Department of Ophthalmology, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand; 2Department of Medicine, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Correspondence: Kavin Vanikieti Email [email protected]
Objective: To compare demographic data, clinical and radiological characteristics, treatments, and long-term visual outcomes between patients with late-onset neuromyelitis optica spectrum disorder-related optic neuritis (LO-NMOSD-ON) (age at onset ≥ 50 years) and patients with early-onset neuromyelitis optica spectrum disorder-related optic neuritis (EO-NMOSD-ON) (age at onset < 50 years).
Patients and Methods: This retrospective study included 47 patients (69 eyes) who were diagnosed with neuromyelitis optica spectrum disorder-related optic neuritis (NMOSD-ON) over a 12-year period. There were 14 patients (21 eyes) and 33 patients (48 eyes) in the LO-NMOSD-ON and EO-NMOSD-ON groups, respectively.
Results: LO-NMOSD-ON–affected eyes exhibited significantly worse median nadir visual acuity (VA) at optic neuritis (ON) onset, compared with EO-NMOSD-ON–affected eyes (2.7 logMAR (range 2.6– 2.9 logMAR) vs 1.95 logMAR (range 0.4– 2.9 logMAR); p = 0.03). Similarly, 100% of LO-NMOSD-ON–affected eyes demonstrated a nadir VA of worse than or equal to 1.0 logMAR, compared with 62.5% of EO-NMOSD-ON–affected eyes (p = 0.03). LO-NMOSD-ON–affected eyes had a worse median final VA, compared with EO-NMOSD-ON–affected eyes (1.3 logMAR (range 0– 2.9 logMAR) vs 0.3 logMAR (range 0– 2.9 logMAR); adjusted p = 0.037). LO-NMOSD-ON–affected eyes more frequently exhibited a final VA of worse than or equal to 1.0 logMAR, compared with EO-NMOSD-ON–affected eyes (57.1% vs 27.0%; adjusted p = 0.039). A positive correlation was observed between age at ON onset of each eye and the final VA (logMAR) (Spearman r = 0.34, p = 0.0075). The remaining parameters did not significantly differ between the two groups.
Conclusion: Patients with LO-NMOSD-ON had significantly worse nadir VA at ON onset and significantly worse final VA, relative to patients with EO-NMOSD-ON. Age at ON onset of each eye was positively correlated with final VA (logMAR). Despite the difference in common age at onset, NMOSD-ON should be included in the differential diagnosis of late-onset acute to subacute optic neuropathy, along with ischemic optic neuropathy.
Keywords: late-onset, optic neuritis, neuromyelitis optica spectrum disorder, Thai
Introduction
Neuromyelitis optica spectrum disorder (NMOSD) is a group of severe demyelinating diseases of the central nervous system.1 These diseases include optic neuritis (ON) and longitudinally extensive transverse myelitis, as well as area postrema, brainstem, diencephalon, and cerebral syndromes. One of the most common initial manifestations is acute-onset ON, which tends to be severe.
The typical age range at NMOSD onset is 32 to 41 years; however, this disorder has also been encountered in children and older adults.2–4 Older age at NMOSD onset is reportedly associated with worse disease prognosis, higher mortality rate, and greater susceptibility to disability.5 When it occurs in older patients (age at NMOSD onset ≥ 50 years), the disorder is known as late-onset neuromyelitis optica spectrum disorder (LO-NMOSD). Notably, one retrospective study demonstrated a relationship between age at ON onset and final visual outcomes; later onset of neuromyelitis optica spectrum disorder-related optic neuritis (NMOSD-ON) was associated with worse final visual outcome.6
Few studies have investigated the epidemiological and clinical characteristics of LO-NMOSD.5,7–13 Some have compared these aspects with early-onset NMOSD (EO-NMOSD; age at NMOSD onset < 50 years).5,10–13 To the best of our knowledge, no studies have been performed to specifically compare clinical characteristics and long-term visual outcomes between patients with late-onset neuromyelitis optica spectrum disorder-related optic neuritis (LO-NMOSD-ON) and those with early-onset neuromyelitis optica spectrum disorder-related optic neuritis (EO-NMOSD-ON). Therefore, this study was performed to comprehensively compare demographic data, clinical and radiological characteristics, treatments, and long-term visual outcomes between patients with LO-NMOSD-ON and patients with EO-NMOSD-ON.
Patients and Methods
Patients
This study protocol followed the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of the Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand. All patients provided informed consent prior to inclusion in the study and their privacy was protected throughout the analysis. Electronic medical records were retrospectively reviewed for patients who had been diagnosed with NMOSD-ON in the Neuro-Ophthalmology Clinic, Faculty of Medicine Ramathibodi Hospital, between January 2008 and June 2020. The diagnosis of NMOSD was performed in accordance with the international consensus diagnostic criteria for NMOSD, with or without aquaporin-4 (AQP4) antibodies.14 All AQP4 antibody testing was performed using a cell-based assay (CBA) (Fixed cells: cell-based indirect immunofluorescence assays utilizing M1-AQP4-transfected HEK293 cells [commercial AQP4-CBA kit; Euroimmun, Lubeck, Germany]). Patients who had NMOSD-ON onset at the age of ≥50 years were diagnosed with LO-NMOSD-ON, while those who had NMOSD-ON onset at the age of <50 years were diagnosed with EO-NMOSD-ON. All included eyes had experienced at least one episode of NMOSD-ON. Exclusion criteria included patients who were <18 years at NMOSD-ON onset and/or affected eyes with visually significant cataract or other ocular diseases that could affect visual acuity (VA). Flow chart of the study selection based on the inclusion and exclusion criteria is demonstrated in Figure 1.
 |
Figure 1 Flow chart of the study selection based on the inclusion and exclusion criteria. |
Data Collection and Outcomes
The following data were collected from the patients’ medical records: sex, age at ON onset, ON follow-up interval, non-ON demyelinating events (prior to or concurrent with ON onset), presence of antinuclear antibody, concurrent autoimmune diseases, and clinical characteristics at ON onset (ie, laterality, presence of pain, nadir VA, and presence of optic disc edema). The magnetic resonance imaging (MRI) of the anterior visual pathway (AVP) was performed at ON onset on two different scanners, a 3.0T scanner (Ingenia; Philips Healthcare, Best, the Netherlands) and a 1.5T scanner (Signa TwinSpeed; GE Healthcare). Each AVP scan was composed of five segments: orbital optic nerve, intracanalicular optic nerve, intracranial optic nerve, optic chiasm, and optic tract.15 Axial and coronal contrast-enhanced T1-weighted images with fat suppression (CE-T1W/FS) were assessed for the presence of enhancement in each segment. Data were also collected concerning acute-phase treatment of each ON episode and maintenance-phase treatment (ie, immunosuppressive drugs used at the last follow-up). Finally, long-term visual outcomes were evaluated. To determine the final VA (primary long-term visual outcome), the last follow-up data were collected at least 6 months after the most recent ON episode. Other parameters as secondary long-term visual outcomes assessed were the presence of ON relapse, ON annualized relapse rate (ie, the ratio of the number of ON episodes to the number of years since ON onset, excluding patients with ON follow-up interval < 1 year), and interval from ON onset to first ON relapse.
Statistical Analysis
Categorical data were summarized using proportions and percentages, then analyzed using the chi-squared test or Fisher’s exact test, as appropriate. Continuous data were summarized using means ± standard deviations (normally distributed data) or medians and ranges (non-normally distributed data). Differences between two groups were analyzed using two-sample t-tests (normally distributed data) or the Mann–Whitney U-test (non-normally distributed data). Snellen VA measurements were converted to the logarithm of the minimum angle of resolution (logMAR) for statistical analysis. For analysis of counting fingers, hand motion, light perception, and no light perception, these VA values were defined as 2.6, 2.7, 2.8, and 2.9 logMAR, respectively.16,17 Final VA (logMAR) and subgroup analysis of affected eye with final VA that was worse than or equal to 1.0 logMAR between LO-NMOSD-ON- and EO-NMOSD-ON-affected eyes were adjusted for possible confounding factors; number of ON episodes (eyes with ON relapse vs without ON relapse) and nadir VA at ON onset of each affected eye (eyes with nadir VA at ON onset that was worse than or equal to 1.0 logMAR vs better than 1.0 logMAR) by linear regression and binary logistic regression analysis, respectively. Statistical analyses were performed using STATA software, version 16.0 (StataCorp LLC, College Station, TX, USA). A value of p < 0.05 was considered statistically significant. Correlation analysis was used to evaluate the relationship between age at ON onset of each eye and the final VA (logMAR).
Results
Demographic Data
In total, 47 patients (69 eyes) were included in this study: 14 patients (21 eyes) and 33 patients (48 eyes) in the LO-NMOSD-ON and EO-NMOSD-ON groups, respectively. All patients were of Asian ethnicity (100% Thai). The female: male ratio was 13:1 (92.8% female) in the LO-NMOSD-ON group, whereas all patients were women in the EO-NMOSD-ON group; this sex ratio did not significantly differ between groups (p = 0.29). Overall, AQP4 antibodies were detected in 44 of 47 patients (93.6%). Myelin oligodendrocyte glycoprotein antibodies were assessed in all three AQP4-seronegative patients but were absent from all three patients. The mean age at ON onset was twofold greater in the LO-NMOSD-ON group than in the EO-NMOSD-ON group (64.1 years vs 32.6 years; p < 0.001). There was no statistically significant difference in median ON follow-up interval between the LO-NMOSD-ON and EO-NMOSD-ON groups (59.5 months (range 6–144 months) vs 43 months (range 6–228 months); p = 0.93). In the LO-NMOSD-ON group, two of 10 patients for whom data were available (20%) experienced non-ON demyelinating events prior to or concurrent with ON onset. Similarly, seven of 22 patients with EO-NMOSD-ON for whom data were available (31.8%) experienced non-ON demyelinating events prior to or concurrent with ON onset (p = 0.68). Myelitis was the most common non-ON demyelinating event experienced in both groups. Antinuclear antibodies were detected in approximately half of the patients in both the LO-NMOSD-ON and EO-NMOSD-ON groups (50% vs 57.5%; p = 0.63). In the LO-NMOSD-ON group, concurrent autoimmune diseases were identified in two patients (14.2%): systemic lupus erythematosus (one patient) and Graves’ disease (one patient). In the EO-NMOSD-ON group, nine patients (27.2%) had concurrent autoimmune diseases: most had systemic lupus erythematosus (four patients). However, the proportion of patients with concurrent autoimmune diseases did not significantly differ between the two groups (p = 0.46). Detailed demographic data are provided in Table 1.
 |
Table 1 Comparison of Demographic Characteristics in Patients with LO-NMOSD-ON and Patients with EO-NMOSD-ON |
Clinical Characteristics at ON Onset
Data regarding clinical characteristics at ON onset were available for 10 patients (10 eyes) and 22 patients (24 eyes) in the LO-NMOSD-ON and EO-NMOSD-ON groups, respectively. Only two patients (9.1%) in the EO-NMOSD-ON group presented with bilateral simultaneous ON, while no patients in the LO-NMOSD-ON group presented with bilateral simultaneous ON (p = 1.00). At ON onset, pain was more frequently observed in EO-NMOSD-ON–affected eyes (79.1%) than in LO-NMOSD-ON–affected eyes (60.0%). However, this difference was not statistically significant (p = 0.39).
Both groups demonstrated poor nadir VA at ON onset. However, the median nadir VA was significantly worse in LO-NMOSD-ON–affected eyes than in EO-NMOSD-ON–affected eyes (2.7 logMAR (range 2.6–2.9 logMAR) vs 1.95 logMAR (range 0.4–2.9 logMAR); p = 0.03). Moreover, all LO-NMOSD-ON–affected eyes demonstrated a nadir VA at ON onset of worse than or equal to 1.0 logMAR, compared with 62.5% of EO-NMOSD-ON–affected eyes (p = 0.03).
Optic disc edema at ON onset was present in 33% of EO-NMOSD-ON–affected eyes and in 0% of LO-NMOSD-ON–affected eyes; this difference was not statistically significant (p = 0.07). A detailed summary of clinical characteristics at ON onset is provided in Table 2.
 |
Table 2 Clinical Characteristics at ON Onset in Patients with LO-NMOSD-ON and Patients with EO-NMOSD-ON |
MRI Characteristics at ON Onset
At ON onset, MRI data were available for 10 AVPs in LO-NMOSD-ON–affected eyes (10 affected eyes) and 24 AVPs in EO-NMOSD-ON–affected eyes (24 affected eyes). Orbital optic nerve enhancement was found in 80% of LO-NMOSD-ON–affected eyes. Conversely, intracanalicular optic nerve enhancement was present in 79.1% of EO-NMOSD-ON–affected eyes. However, there were no statistically significant differences in segmental enhancement or total enhanced segments of AVPs between the two groups at ON onset. EO-NMOSD-ON–affected eyes had a slightly higher proportion of AVPs with ≥2 consecutive enhanced segments, compared with LO-NMOSD-ON–affected eyes; however, this difference was not statistically significant (p = 0.43). A detailed summary of MRI characteristics at ON onset is provided in Table 3.
 |
Table 3 Magnetic Resonance Imaging Characteristics at ON Onset in Patients with LO-NMOSD-ON and Patients with EO-NMOSD-ON: Segmental Enhancement of AVPs |
Treatment
Acute Phase
Acute-phase treatment was performed in 24 LO-NMOSD-ON episodes and 63 EO-NMOSD-ON episodes in our institution. All affected patients were treated with 3–5 consecutive days of intravenous methylprednisolone (IVMP) 1 g/day, followed by slowly tapered prednisolone for 2–3 months. There was no statistically significant difference in the median interval from ON onset to IVMP treatment between the LO-NMOSD-ON group and EO-NMOSD-ON groups (5 days (range 1–45 days) vs 6 days (range 0–45 days); p = 0.62). For patients who did not respond to IVMP treatment, adjunctive plasma exchange was performed as second-line therapy in two LO-NMOSD-ON episodes (8.3%) and five EO-NMOSD-ON episodes (7.9%); however, this difference was not statistically significant (p = 1.00). A detailed summary of acute-phase treatment is provided in Table 4.
 |
Table 4 Acute-Phase Treatment in Patients with LO-NMOSD-ON and Patients with EO-NMOSD-ON |
Maintenance Phase
All patients received immunosuppressive drugs for at least 5 years following the diagnosis of NMOSD-ON or NMOSD. The proportion of patients receiving immunosuppressive drugs at the last follow-up was much greater in patients with EO-NMOSD-ON than in patients with LO-NMOSD-ON (81.8% vs 57.1%). However, this difference was not statistically significant (p = 0.14). Azathioprine and mycophenolate mofetil were the most common immunosuppressive drugs used in patients with LO-NMOSD-ON (50%) and those with EO-NMOSD-ON (44.4%), respectively. A detailed summary of maintenance-phase treatment is provided in Table 5.
 |
Table 5 Maintenance-Phase Treatment in Patients with LO-NMOSD-ON and Patients with EO-NMOSD-ON: Immunosuppressive Drugs Used at the Last Follow-Up |
Long-Term Visual Outcomes
Sixty-nine affected eyes of 47 patients were included in the assessment of final VA. There was a significant difference in median final VA between the two groups: it was 1.3 logMAR (range 0–2.9 logMAR) in LO-NMOSD-ON–affected eyes, whereas it was 0.3 logMAR (range 0–2.9 logMAR) in EO-NMOSD-ON–affected eyes (adjusted p = 0.037). Furthermore, more LO-NMOSD-ON–affected eyes exhibited a final VA of worse than or equal to 1.0 logMAR, compared with EO-NMOSD-ON–affected eyes (57.1% vs 27.0%; adjusted p = 0.039). There were no statistically significant differences between patients with LO-NMOSD-ON and those with EO-NMOSD-ON in terms of the proportion of patients with ON relapse, the ON annualized relapse rate, or the interval from ON onset to first ON relapse.
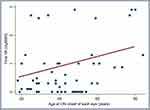
Correlation analysis showed that age at ON onset of each eye was moderately positively correlated with final VA (logMAR) (Spearman r = 0.34, p = 0.0075) (Figure 2). Furthermore, two patients died in the overall cohort; although both were in the LO-NMOSD-ON group, the rate of death did not significantly differ between groups (p = 0.29). The main cause of death in these two patients was septic shock due to pulmonary infection (pulmonary aspergillosis in a 77-year-old patient and bacterial pneumonia in an 85-year-old patient). A detailed summary of long-term visual outcomes is provided in Table 6.
 |
Table 6 Long-Term Visual Outcomes in Patients with LO-NMOSD-ON and Patients with EO-NMOSD-ON |
Discussion
This study compared demographic data, clinical and radiological characteristics, treatments, and long-term visual outcomes between 14 patients with LO-NMOSD-ON and 33 patients with EO-NMOSD-ON. Patients with LO-NMOSD-ON had both significantly worse nadir VA at ON onset and significantly worse final VA, relative to patients with EO-NMOSD-ON. To the best of our knowledge, this is the first study to comprehensively compare these ophthalmic aspects between LO-NMOSD-ON and EO-NMOSD-ON.
Demographic Data
The majority of patients with LO-NMOSD-ON and all patients with EO-NMOSD-ON were women in this study. These results were in agreement with previous findings of strong female predominance in patients with NMOSD.5,7–13 In our LO-NMOSD-ON cohort, the mean age at ON onset was approximately 65 years, which was slightly higher than the ages reported in previous studies (56–59.4 years).5,7–13 However, the mean age at ON onset was 32.6 years in our EO-NMOSD-ON cohort, which is comparable with the typical age at NMOSD onset in previous studies (32–41 years).2–4 Moreover, our previously published article, which studied prognostic factors for visual outcomes following the first episode of ON in each affected eye in overall age group of NMOSD-ON patients, showed that a median age at NMOSD-ON onset was 36 years (range 4–84 years).18 Notably, unlike our previously published article, patients with age < 18 years at NMOSD-ON onset were excluded in this study.
Small proportions of patients in the LO-NMOSD-ON (20%) and EO-NMOSD-ON groups (31.8%) experienced non-ON demyelinating events prior to or concurrent with ON onset; notably, myelitis was the most common event. These results imply that both patients with LO-NMOSD-ON and those with EO-NMOSD-ON were more likely to present with isolated ON as the initial manifestation of NMOSD. Therefore, ophthalmologists should ensure they are familiarized with NMOSD-related ON. This indicates the important roles of both ophthalmologists and neurologists in the establishment of NMOSD diagnosis.
There was no statistically significant difference in the presence of antinuclear antibody between patients with LO-NMOSD-ON and those with EO-NMOSD-ON, as in previous studies.11,13 Nine patients (27.2%) in the EO-NMOSD-ON group and two patients (14.2%) in the LO-NMOSD-ON group had concurrent autoimmune diseases; this finding was comparable with the results of previous studies in which there were no differences between patients with EO-NMOSD-ON and those with LO-NMOSD-ON in terms of concurrent autoimmune diseases.7,8,10–13
Clinical Characteristics at ON Onset
At ON onset, bilateral simultaneous ON was observed in two patients in the EO-NMOSD-ON group, compared with none in the LO-NMOSD-ON group. In contrast, a previous retrospective study reported that 11 of 59 patients with LO-NMOSD-ON (18.6%) experienced bilateral simultaneous ON.11 The difference in results between studies is presumably because our investigation included a smaller number of patients with LO-NMOSD-ON. Furthermore, pain is one of the most frequent symptoms at ON onset; this was observed in approximately three-fifths of both LO-NMOSD-ON–affected eyes and EO-NMOSD-ON–affected eyes. These rates were fairly similar to the findings in a previous study.19
In our study, LO-NMOSD-ON–affected eyes had significantly worse nadir VA at ON onset, compared with EO-NMOSD-ON–affected eyes. Moreover, all LO-NMOSD-ON–affected eyes demonstrated a nadir VA at ON onset of worse than or equal to 1.0 logMAR, compared with 62.5% of EO-NMOSD-ON–affected eyes. These results were consistent with the findings in previous studies, whereby patients with LO-NMOSD had worse Expanded Disability Status Scale scores after first attack, relative to patients with EO-NMOSD.12 Worse nadir VA at ON onset in LO-NMOSD-ON–affected eyes might be the result of a negative relationship between retinal nerve fiber layer thickness and age.20–22 Older patients tend to have thinner retinal nerve fiber layer thickness. ON is one of the core demyelinating events in NMOSD; when this occurs, affected eyes in older patients tend to have more severe destruction of the retinal nerve fiber layer. This destruction presumably causes worse nadir VA at ON onset in LO-NMOSD-ON–affected eyes.
We observed that optic disc edema tended to occur more in EO-NMOSD-ON–affected eyes than in LO-NMOSD-ON–affected eyes, although this difference was not statistically significant. As noted above, older patients tend to have thinner retinal nerve fiber layer thickness,20–22 which might have interfered with clinical detection of optic disc edema. Importantly, we are unaware of studies concerning this manifestation, for which the results could be compared with our current findings.
MRI Characteristics at ON Onset
Although we found no statistically significant difference in segmental enhancement of AVPs between the two groups, we found that the orbital and intracanalicular optic nerve segments, respectively, were most commonly enhanced in LO-NMOSD-ON–affected eyes and EO-NMOSD-ON–affected eyes at ON onset. Previous studies demonstrated a greater tendency toward posterior enhancement of AVPs including the intracranial optic nerve, optic chiasm, and optic tract in patients with NMOSD-ON.14 This disparate finding might be related to differences in intervals from ON onset to MRI examination, which could affect enhancement appearance on MRI. Moreover, most of our patients underwent MRI examinations after the initiation of IVMP treatment, which could interfere with enhancement detection on MRI.
Overall, more than half of the affected eyes in our study demonstrated ≥2 consecutive enhanced segments at ON onset, a result that did not significantly differ between groups. Notably, this radiological finding was consistent with longitudinally extensive involvement of AVPs previously reported in patients with NMOSD-ON.14 However, we did not evaluate the actual length of enhancement, contrary to the approach in the previous study.14
Treatment
Acute Phase
In our institution, IVMP is the first-line acute-phase treatment for NMOSD-ON. Thus, all patients in this study received 3–5 consecutive days of intravenous IVMP 1 g/day, followed by slowly tapered prednisolone for 2–3 months. The interval from ON onset to IVMP treatment was similar in both groups. Adjunctive plasma exchange was our second-line adjunctive treatment, solely administered to patients who did not respond to IVMP. Adjunctive plasma exchange was performed in fewer than 10% of the episodes in each group. This suggested that both patients with LO-NMOSD-ON and those with EO-NMOSD-ON were likely to achieve a satisfactory response to IVMP treatment.
Maintenance Phase
Immunosuppressive drugs tended to be used more often in patients with EO-NMOSD-ON than in patients with LO-NMOSD-ON at the last follow-up, although this difference was not statistically significant. Older adults are more likely to have several comorbidities and experience a risk of adverse drug reactions. The occurrence of immunosuppressive drug-related complications might cause treating physicians to less frequently use immunosuppressive drugs for more than 5 years in older adults.
Because of the existing lack of prospective, randomized controlled trials, there is no consensus regarding standard immunosuppressive drug treatment for patients with NMOSD. In our institution, overall, azathioprine was used as the primary treatment for NMOSD during the study period. Mycophenolate mofetil was the next most common immunosuppressive drug, administered to patients who did not respond to azathioprine or who developed serious side effects (eg, drug-induced hepatitis). Insurance coverage for medical expenses was another factor that presumably influences the selection of immunosuppressive drugs for individual patients.
Long-Term Visual Outcomes
At the last follow-up, median final VA was worse in LO-NMOSD-ON–affected eyes than in EO-NMOSD-ON–affected eyes. Additionally, twofold more LO-NMOSD-ON–affected eyes exhibited final VA of worse than or equal to 1.0 logMAR, compared with EO-NMOSD-ON–affected eyes. These findings were comparable with the results in several Asian and Caucasian population-based studies that found worse Expanded Disability Status Scale scores at the last visit, as well as greater motor disability and wheelchair dependence, in patients with LO-NMOSD than in patients with EO-NMOSD.5,8,13 Additionally, one multicenter study found more frequent severe visual disability (ie, VA worse than or equal to 1.0 logMAR) in patients with LO-NMOSD than in patients with EO-NMOSD.12 Here, we found a positive correlation between age at ON onset of each eye and final VA (logMAR). This was similar to the positive correlations between age at disease onset and Expanded Disability Status Scale score observed in previous studies.5,8 This finding implies that age at disease onset may affect disability outcomes; specifically, older age at disease onset may be associated with worse disability outcomes.
An association between older age and a weakened repair mechanism proposed in a previous study7 is a possible explanation for the worse final VA in LO-NMOSD-ON–affected eyes than in EO-NMOSD-ON–affected eyes in our study. Older patients are more susceptible to disability due to this weakened repair mechanism or reduced immune tolerance, leading to abnormal anti-inflammatory and restorative processes.5,7 Therefore, older patients might be more susceptible to visual disability, consistent with our results.
In our study, we found no statistically significant differences in ON annualized relapse rate or the proportion of patients with ON relapse between the two groups, which matched the findings of several previous studies.5,7,12,13 However, our annualized relapse rate and proportion of patients with relapse were both lower than in those previous studies. This was likely because we exclusively examined ON in our patients; we did not assess other non-ON demyelinating events in patients with NMOSD, whereas such events were assessed in the previous studies.
Although there was no statistically significant difference in mortality rate between the two groups, two patients with LO-NMOSD-ON (14.2%) died during follow-up. The main cause of death in these two patients was septic shock due to respiratory tract infection, a severe adverse event associated with immunosuppressive drug treatment. This result was similar to the findings in several previous studies, where the two main causes of death in patients with LO-NMOSD were infection and extensive central nervous system demyelination (ie, extensive myelitis).7,8,10,13 Accordingly, older adults might be at increased risk of infection during immunosuppressive drug treatment, due to an impaired protective immune response and reduced resistance to infectious diseases.23 Therefore, the cautious use of immunosuppressive drugs and routine screening for opportunistic infection during immunosuppressive therapy are strongly suggested for patients with NMOSD, especially when those patients are older adults.
There were several strengths in this study. First, this study involved the comparison of various demographic characteristics, clinical and radiological characteristics, treatments, and long-term visual outcomes between patients with LO-NMOSD-ON and those with EO-NMOSD-ON. To the best of our knowledge, this was the first comprehensive study involving comparison between these patient groups. Second, the ON follow-up intervals in our cohorts were both sufficient to represent long-term visual outcomes (median 59.5 months (range 6–144 months) vs 43 months (range 6–228 months) in patients with LO-NMOSD-ON and those with EO-NMOSD-ON, respectively). Lastly, our study highlights the gap in differential diagnosis of late-onset acute optic neuropathy and subacute optic neuropathy, in addition to ischemic optic neuropathy (ie, the most common non-glaucomatous optic neuropathy in older adults). We consider an awareness of NMOSD-ON in older adults to be crucial due to its distinct treatment and prognosis, compared with ischemic optic neuropathy. Early diagnosis and prompt treatment preserve better visual outcomes, while preventing further morbidity and mortality.
There were some limitations in this study. First, it had a retrospective design, which presumably resulted in some data loss. Second, all patients in our study were Asian; therefore, the results might not be generalizable to patients of other ethnicities. Third, this study did not assess other elements of visual function (eg, color vision and visual field) or structural characteristics (eg, retinal nerve fiber layer thickness). Lastly, pediatric patients were excluded from our study, so our results cannot be used for guidance of clinical treatment in the pediatric population. In the future, a large prospective study is needed to confirm our findings and provide more conclusive information regarding the ophthalmic aspects of LO-NMOSD-ON, as well as a better understanding of the differences between patients with LO-NMOSD-ON and those with EO-NMOSD-ON.
Conclusions
Patients with LO-NMOSD-ON had both significantly worse nadir VA at ON onset and significantly worse final VA, relative to patients with EO-NMOSD-ON. Age at ON onset of each eye was positively correlated with final VA (logMAR). Despite the difference in common age at onset, NMOSD-ON should be included in the differential diagnosis of late-onset acute to subacute optic neuropathy, along with ischemic optic neuropathy.
Acknowledgments
The authors thank Mr. Nattawut Unwanatham, Department of Clinical Epidemiology and Biostatistics, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand and Dr. Passara Jongkhajornpong, MD, Department of Ophthalmology, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand for their advices on the statistical analyses. The authors also thank Ryan Chastain-Gross, Ph.D., from Edanz Group (https://en-author-services.edanz.com/ac) for editing a draft of this manuscript.
Disclosure
The authors declare that they have no competing interests.
References
1. Fujihara K. Neuromyelitis optica spectrum disorders. Curr Opin Neurol. 2019;32(3):385–394. doi:10.1097/WCO.0000000000000694
2. Mealy MA, Wingerchuk DM, Greenberg BM, et al. Epidemiology of neuromyelitis optica in the United States: a multicenter analysis. Arch Neurol. 2012;69(9):1176–1180. doi:10.1001/archneurol.2012.314
3. Ghezzi A, Bergamaschi R, Martinelli V, et al. Clinical characteristics, course and prognosis of relapsing Devic’s neuromyelitis optica. J Neurol. 2004;251(1):47–52. doi:10.1007/s00415-004-0271-0
4. Kim SH, Kim W, Li XF, et al. Clinical spectrum of CNS aquaporin-4 autoimmunity. Neurology. 2012;78(15):1179–1185. doi:10.1212/WNL.0b013e31824f8069
5. Carnero Contentti E, Daccach Marques V. Soto de Castillo I, et al. Clinical features and prognosis of late-onset neuromyelitis optica spectrum disorders in a Latin American cohort. J Neurol. 2020;267(5):1260–1268. doi:10.1007/s00415-020-09699-2
6. Akaishi T, Nakashima I, Takeshita T, et al. Lesion length of optic neuritis impacts visual prognosis in neuromyelitis optica. J Neuroimmunol. 2016;293:28–33. doi:10.1016/j.jneuroim.2016.02.004
7. Collongues N, Marignier R, Jacob A, et al. Characterization of neuromyelitis optica and neuromyelitis optica spectrum disorder patients with a late onset. Mult Scler. 2013;20(8):1086–1094. doi:10.1177/1352458513515085
8. Cai L, Zhang Q, Zhang Y, et al. Clinical characteristics of very late-onset neuromyelitis optica spectrum disorder. Mult Scler Relat Disord. 2020;46:102515. doi:10.1016/j.msard.2020.102515
9. Fragoso Y, Ruocco H, Dias R, et al. Late onset of neuromyelitis optica spectrum disorders. Neurol Ther. 2019;8(2):477–482. doi:10.1007/s40120-019-0143-2
10. Seok J, Cho H, Ahn S, et al. Clinical characteristics of late-onset neuromyelitis optica spectrum disorder: a multicenter retrospective study in Korea. Mult Scler. 2017;23(13):1748–1756. doi:10.1177/1352458516685416
11. Zhang L, Yang L, Li T, et al. Distinctive characteristics of early-onset and late-onset neuromyelitis optica spectrum disorders. J Neurosci. 2016;127(4):334–338.
12. Sepulveda M, Delgado-García G, Blanco Y, et al. Late-onset neuromyelitis optica spectrum disorder. Neurol Neuroimmunol Neuroinflamm. 2019;6(6):1–9. doi:10.1212/NXI.0000000000000607
13. Mao Z, Yin J, Zhong X, et al. Late-onset neuromyelitis optica spectrum disorder in AQP4-seropositive patients in a Chinese population. BMC Neurol. 2015;15(1):1–7. doi:10.1186/s12883-015-0417-y
14. Wingerchuk D, Banwell B, Bennett J, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015;85(2):177–189. doi:10.1212/WNL.0000000000001729
15. Song H, Zhou H, Yang M, et al. Different characteristics of aquaporin-4 and myelin oligodendrocyte glycoprotein antibody-seropositive male optic neuritis in China. J Ophthalmol. 2019;2019:1–7. doi:10.1155/2019/4015075
16. Grover S, Fishman G, Anderson R, et al. Visual acuity impairment in patients with retinitis pigmentosa at age 45 years or older. Ophthalmology. 1999;106(9):1780–1785. doi:10.1016/S0161-6420(99)90342-1
17. McAnany J, Genead M, Walia S, et al. Visual acuity changes in patients with Leber congenital amaurosis and mutations in CEP290. JAMA Ophthalmol. 2013;131(2):178–182. doi:10.1001/2013.jamaophthalmol.354
18. Thongmee W, Padungkiatsagul T, Jindahra P, et al. Prognostic factors for visual outcomes following the first episode of NMOSD-related optic neuritis in affected eyes. Clin Ophthalmol. 2020;14:4271–4278. doi:10.2147/OPTH.S285443
19. Kim H, Park K, Oh S, et al. Association of optic neuritis with neuromyelitis optica spectrum disorder and multiple sclerosis in Korea. Korean J Ophthalmol. 2019;33(1):82–90. doi:10.3341/kjo.2018.0050
20. Chen C-Y, Huang EJ-C, Kuo C-N, et al. The relationship between age, axial length and retinal nerve fiber layer thickness in the normal elderly population in Taiwan: the Chiayi eye study in Taiwan. PLoS One. 2018;13(3):1–13.
21. Celebi ARC, Mirza GE. Age related change in retinal nerve fiber layer thickness measured with spectral domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2013;54(13):8095–8103. doi:10.1167/iovs.13-12634
22. Jindahra P, Hengsiri N, Witoonpanich P, et al. Evaluation of retinal nerve fiber layer and ganglion cell layer thickness in Alzheimer’s disease using optical coherence tomography. Clin Ophthalmol. 2020;14:2995–3000. doi:10.2147/OPTH.S276625
23. Wick G, Grubeck-Loevenstein B. The aging immune system: primary and secondary alterations of immune reactivity in the elderly. Exp Gerontol. 1997;32(4–5):401–413. doi:10.1016/S0531-5565(96)00152-0
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.