Back to Journals » Clinical Ophthalmology » Volume 16
Comparison of Dose Increments of Botulinum Toxin A with Surgery as Primary Treatment for Infantile Esotropia and Partially Accommodative Esotropia
Authors AlShamlan FT , Alghazal F
Received 15 July 2022
Accepted for publication 23 August 2022
Published 27 August 2022 Volume 2022:16 Pages 2843—2849
DOI https://doi.org/10.2147/OPTH.S382499
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Fatemah T AlShamlan, Fatimah Alghazal
Pediatric Ophthalmology and Strabismus Department, Dhahran Eye Specialist Hospital, Dhahran, Saudi Arabia
Correspondence: Fatemah T AlShamlan, Email [email protected]
Purpose: To compare the effect of increment dose of botulinum toxin (BTX) injection in correlation to the angle of deviation to bilateral medial rectus recession (BMR) in infantile esotropia and partially accommodative esotropia (PAET).
Methods: This was a retrospective study that included pediatric patients ≤ 16 years old with infantile esotropia and PAET at Dhahran Eye Specialist Hospital (DESH) from 2014 till 2021 treated with increment dose of BTX or BMR. A successful outcome is defined as ocular alignment within 10 PD of deviation after 1– 3 BTX injections or one surgery with a minimum follow-up of 6 months.
Results: Of 177 patients, 101 patients received BTX treatment for either infantile esotropia (n = 37) or PAET (n = 64) and 76 patients underwent BMR for either infantile ET (n = 25) or PAET (n = 51). BTX showed a higher success rate than BMR {65.3% vs 55.3% (p = 0.174)}. In patients with infantile esotropia, the success rate was comparable between BTX group and BMR group {40.5% vs 52% (p = 0.440)}. However, the success rate was statistically significantly higher in BTX group in compare to BMR group {79.7% vs 56.9% (p = 0.014)}. Consecutive exotropia was 0% in BTX group and 9.2% in BMR group (p = 0.002).
Conclusion: The increment dose of BTX injection is comparable to surgery in patients with infantile esotropia but superior to the routine surgery in patients with PAET. BTX has the advantage of a shorter procedure duration, lower costs, less exposure to general anesthesia and being minimally invasive intervention.
Keywords: esotropia, botulinum toxin, partially accommodative esotropia, infantile esotropia
Introduction
Esotropia is a form of ocular misalignment, in which the eye is rotated nasally.1 It is classified according to the age at which infantile esotropia typically occurred. Infantile esotropia usually occurs during the first six months of age while acquired esotropia usually occurs later.2 Acquired esotropia is furthermore classified into nonaccommodative esotropia and accommodative esotropia in which the deviation usually responds to either fully or partially hyperopic spectacles or contact lenses.2 If the deviation persists after total refractive error correction, the strabismus surgery or botulinum toxin (BTX) injection to extraocular muscles will be proposed.3 BTX is a toxin that is produced by Clostridium Botulinum and causes temporal paralysis of the muscle by preventing the release of acetylcholine from the nerve terminal.4 Alan Scott was the first to introduce the use of BTX as a less invasive procedure for treating strabismus in 1981.4 Since then, many studies have revealed that BTX is safe and represents a valuable alternative to strabismus surgery.5–9 Apparently, only one study used increment doses of BTX according to the amount of angle deviation in a different type of esotropia, and it was more effective in a partially accommodative esotropia (PAET) followed by infantile esotropia.6 However, the study was limited by a lack of comparison with a patient who underwent strabismus surgery. Moreover, only one study compared bilateral medial rectus recession (BMR) to BTX in a patient with PAET only without a correlation of BTX dose to the angle of deviation.9
Up to our best knowledge, there are no studies in the literature that have compared the efficacy of increment doses of BTX to BMR in PAET or infantile esotropia.
Aim/Objective
To compare the efficacy of BTX dose increments to BMR in treating children with Infantile esotropia and PAET.
Method
It is a retrospective, non-randomized case–control study that was approved by the research committee in Dhahran Eye Specialist Hospital (DESH), Dhahran, Saudi Arabia, and the consent was already obtained that the information in the file might be used for research purposes by the parents of all patients under 18 years of age in compliance with the Declaration of Helsinki. The medical records of all cases that underwent increment doses of BTX versus BMR for PAET and infantile esotropia in DESH from 2014 till 2021 were reviewed. The Inclusion criteria were pediatric patients ≤16 years with PAET and infantile esotropia, with a minimum follow-up duration of 6 months after the last BTX injection or surgery. Patients were excluded if there was any previous strabismus surgery or previous BTX injection outside DESH, other types of esotropia, presence of vertical deviations, A or V pattern before treatment, dissociated vertical or dissociated horizontal deviation before treatment, nystagmus or presence of other ocular pathologies.
Patients were divided into two groups, the BTX group and the BMR group. Any patient who received BTX then followed by surgery was considered treatment failure in the BTX group and excluded from the BMR group.
The data recorded from the patients’ charts included age at intervention, gender, visual acuity (converted into a logarithm of the minimum angle of resolution (LogMAR)), cycloplegic refraction, a complete orthoptic examination after giving the full optical correction (included measured angle of deviation in the primary position at distance and near with alternate prism cover test if the patient was able to cooperate or by Krimsky otherwise), final diagnosis, treatment option and the angle of deviation post-treatment with a minimum follow-up of 6 months post-BTX injection or surgery.
In the BTX group, the injection was performed by a single surgeon in the operating room under general anesthesia for all patients. 100 IU of BTX (Onabotulinum toxin A, Botox®) diluted with 2 mL of saline. A 30-gauge needle was inserted blindly into the bilateral medial rectus muscle after visualizing the anterior ciliary vessels without electromyogram (EMG) guidance and through intact conjunctiva. The BTX group was sub-divided into four groups according to the mean angle of deviation and corresponding dose of BTX given per muscle (Table 1).
 |
Table 1 BTX Dosages and Their Corresponding Angles of Deviation |
In the BMR group, the BMR was performed by a single surgeon. The surgeon operated on the maximum angle of esotropia, which was measured after full optical correction. The amount of recession depended on the angle of deviation (Table 2).
 |
Table 2 Amount of Recession and Their Corresponding Angles of Deviation |
A successful outcome for both groups was defined as ocular alignment within 10 PD of deviation after 1–3 BTX injections or after one surgery with a minimum follow-up of 6 months.
Patients with residual horizontal deviations >10 PD or patients who required second treatment with strabismus surgery in the BTX group or reoperation in the BMR group were considered treatment failures.
The outcomes that were measured in each group were success, residual esotropia and consecutive exotropia.
Statistical Analysis
The normality of data was assessed with Shapiro–Wilk Test. Normally distributed data were compared with independent-samples t-test. Non-normally distributed data were compared with Mann–Whitney U-Test. Categorical data were compared with Pearson Chi-Square Test. The odds ratios with their p-values were calculated using binary logistic regression. Statistical analysis was performed using Statistical Package for the Social Sciences (IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.). Figures were created using Microsoft Excel (2019, Microsoft Corp.). A p-value less than 0.05 was considered statistically significant.
Results
Between 2014 and 2021, 177 children (≤16years), of whom 101 patients underwent BTX treatment (BTX group) for either infantile esotropia (n = 37) or PAET (n = 64) and 76 patients underwent BMR (BMR group) for either infantile ET (n = 25) or PAET (n = 51) were included in the study. The age at treatment, gender, visual acuity, spherical equivalent, angle of deviation and diagnosis were all similar (p > 0.05) (Table 3).
 |
Table 3 Demographic and Pre-Treatment Clinical Characteristics |
In BTX group, the percent of doses for the first injection were 11.9% (n = 12) for 2.5 IU, 28.7% (n = 29) for 5.0 IU, 19.8% (n = 20) for 7.5 IU and 39.6% (n = 40) for 10 IU with a mean of 7.18 ± 2.69 IU (2.5 IU to 10 IU). In BMR group, patients who underwent BMR of 4.0 mm was 9.2% (n = 7), 4.5 mm was 11.8% (n = 9), 5.0 mm was 22.4% (n = 17), 5.5 mm was 26.3% (n = 20), 6.0 mm was 17.1% (n=13), and 6.5 mm was 13.2% (n = 10) with a mean recession of medial rectus muscle from insertion was 5.34 ± 0.75 mm (3.50 to 6.50 mm).
At 6 months post-treatment, the percentage of patients who underwent 1, 2 and 3 injections in BTX group were 73.3% (n = 74), 21.8% (n=22), and 5% (n = 5), respectively. The cumulative success rate was 47.5%, 62.4% and 65.3% after 1st, 2nd and 3rd injections, respectively. The success rates after only 1 injection per dose (n = 101) were 83.3% (n = 10/12) for 2.5 IU, 62.1% (n = 18/29) for 5.0 IU, 65% (n = 13/20) for 7.5 IU and 17.5% (n = 7/40) for 10 IU (p < 0.001) (Table 4).
 |
Table 4 Success Rate per Number of Botulinum Toxin A Injections per Dose |
The mean number of botulinum toxin injections with successful outcomes was 1.3 ± 0.6 (1 to 3 injections).
The success rate in BMR group was 71.4% for 4.0 mm, 66.7% for 4.5 mm, 64.7% for 5.0 mm, 45% for 5.5 mm, 46.2% for 6.0 mm and 50% for 6.5 mm (p = 0.665) with an overall success rate 55.3% (n = 42) (p = 0.213).
A patient in BTX group was 1.53 times (Odds ratio) more likely to have a successful outcome than that in BMR group (p = 0.174). Residual esotropia was 34.7% (n = 35) and 35.5% (n = 27) in BTX group and BMR group, respectively (p = 1.0). Incidence of consecutive exotropia was 0% (n = 0) and 9.2% (n = 7) in BTX group and BMR group, respectively (p = 0.002) (Figure 1).
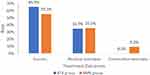 |
Figure 1 Treatment outcomes. |
In patients with infantile esotropia, the treatment outcomes (success, residual esotropia and consecutive exotropia) were not significantly different between BTX group and BMR group (p = 0.275). The success rate was comparable between both groups: 40.5% in BTX group and 52% in BMR group (p = 0.440). The residual esotropia rate was not statistically significantly different between groups: 59.5% in BTX group and 44% in BMR group (p = 0.302). The incidence of consecutive exotropia was not statistically significantly different between groups: 0% in BTX group and 4% in BMR group (p = 0.403).
However, there was a statistically significant difference in the outcomes between groups in patients with PAET (p = 0.004). The success rate was statistically significantly different between groups: 79.7% in BTX group and 56.9% in BMR group (p = 0.014). A patient in BTX group was 2.98 times (p = 0.009) more likely to have a successful outcome than that in BMR group. The residual esotropia rate was not statistically significantly different between groups: 20.3% in BTX group and 31.4% in BMR group (p = 0.199). The incidence of consecutive exotropia was statistically significantly different between groups: 0% in BTX group and 11.8% in BMR group (p = 0.006) (Table 5) (Figure 2).
 |
Table 5 Treatment Outcomes per Diagnosis |
 |
Figure 2 Treatment outcomes per diagnosis. |
Discussion
The successful outcome in our study was higher in patients who underwent increment doses of BTX after the first injection 47.5% (p < 0.001) representing 72.7% of all patients with successful outcomes in the BTX group. Furthermore, a statistical significance was found in patients who received the first injection with the highest success rate in patients who received 2.5 IU (83.3%) and the least successful rate in patients who received 10 IU (17.5%). This could be explained by the small angle at presentation that required small dose of BTX and the fact that any patient beyond 40 PD was given the same dose of 10 IU that would be given to a patient with deviation ranging from (30–40 PD). Those patients who did not achieve successful outcomes after the first injection had a higher success rate after receiving multiple injections with a cumulative success rate of 62.4% and 65.3% after second and third injections, respectively, using the same methodology of increment doses (55.6% and 60% of patients who underwent 2nd and 3rd injection have successful outcomes respectively). Our results were comparable with several studies in terms that the smallest angle of deviation had the highest success rate.3,5,6,8–12
Up to our knowledge, Alshamlan et al6 is the only study that used increment doses of BTX to a specific range of angle of deviation. It showed a success rate of 39.3% out of 56 patients, while our study showed an overall success rate 65.3% of a total of 101 patients. The higher success rate in our study in comparison to Alshamlan study,6 our study used the same increment doses to the same range of angle of deviation as their study, could be attributed to the lower number of patients in the latter study (101 vs 56). In addition, they considered patients who did not achieve ≤10 PD of orthotropia after only the first injection as a failure while we had patients undergo a maximum of 3 injections. Considering successful outcomes after the only first injection, our study had a 47.5% success rate, which is comparable to Alshamlan study6 with a success rate of 39.3%.
Al Taisan et al5 found that the success rate of BTX in strabismus was 54%, with the highest success rate in PAET 70.6% followed by infantile esotropia 36.4% which is consistent with our result which found that the overall success rate 65.3% with 79.7% success rate in PAET and 40.5% in infantile esotropia.
Infantile Esotropia
In our study, it was found that the result of increment doses of BTX in infantile esotropia was comparable to surgery with (p = 0.440) which is similar to Gursoy et al8 results with (p = 0.87) taking into consideration that they did not use increment dose of BTX injection according to the angle of deviation instead they used 4 IU for the first injection and 2.5 IU for the second injection regardless the amount of deviation.
De Alba Campomanes et al7 found that the surgery was superior to BTX injection in large-angle infantile esotropia, with a successful rate after surgery of 65.8% compared to 45% after BTX injection while in our study 52% had a success rate after surgery and 40.5% after BTX injection and was statistically insignificant (p = 0.440). Majority of patients in De Alba Campomanes7 study underwent BTX injection 322 while only 120 patients underwent surgery. Thus, the number in the BTX group was more than double than that in the surgery which ultimately affects the results when comparing the two groups. On the other hand, our study had 37 patients in the BTX group and 25 patients in the BMR group. Even though there was no statistical difference between the BTX injection and surgery in infantile esotropia, the former has the advantage of shorter duration of the procedure, less exposure to general anesthesia and being a minimal invasive intervention.
Partially Accommodative Esotropia
The success rate in PAET was significant between the two groups with a 79.7% success rate in the BTX group and 56.9% in the BMR group (p = 0.014). A patient in the BTX group was 2.98 times (p = 0.009) more likely to have a successful outcome than that in the BMR group.
Our finding is higher than the success rate achieved by Alshamlan et al6 59.1%, and this difference can be explained by the larger number of patients included in our study (n = 64) in comparison to their study (n = 22). In addition, the patients in our study who did not achieve the desired angle from the first injection underwent second and third injection before considering them as a failure. Furthermore, their study lacked comparison to surgery.
Alshammari et al9 study had a lower success rate in the BTX group (53.7%) compared to the BMR group (70.9%) in a patient with PAET (p = 0.006). This can be attributed to the high variability of the dose of BTX (3–10 IU), which was not correlated to the amount of angle of deviation. Thus, it was highly subjective depending on the surgeon preference. In addition, only 20 of 64 patients received a second injection and 25 patients underwent surgery after the first injection, which might have affected the success rate.
The incidence of consecutive exotropia was statistically significant between groups. It was 0% in BTX group and 11.8% in BMR group (p = 0.006). These findings are consistent with Alshammari9 study with 0% of consecutive exotropia in BTX group and 2% in the BMR group.
In our study, BTX injection was done by a single surgeon with an objective scale of increment doses to a specific angle of deviation and surgery was performed by a single surgeon with specific mm of recession to a specific angle of deviation. Thus, the variation was minimized.
The major limitation of our study is that it is a retrospective with a small sample size and stereoacuity assesment was not measured before and after the intevention.
In conclusion, the increment dose of BTX injection in correlation to the angle of deviation is comparable to surgery especially in a patient with infantile esotropia where they usually have a large angle of deviation with BTX injection having the advantage of being shorter in duration, lower costs, less exposure to general anesthesia and minimally invasive intervention. The increment dose of BTX injection in PAET was found to be superior to standard surgery with an incidence of 0% consecutive exotropia.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zou YC, Liu L. The management of childhood esotropia with hyperopia. Curr Med Res Opin. 2011;27(4):731–735. PMID: 21265594. doi:10.1185/03007995.2011.552973
2. Mohney BG. Common forms of childhood strabismus in an incidence cohort. Am J Ophthalmol. 2007;144(3):465–467. PMID: 17765436. doi:10.1016/j.ajo.2007.06.011
3. Rowe FJ, Noonan CP. Botulinum toxin for the treatment of strabismus. Cochrane Database Syst Rev. 2017;3(3):CD006499. PMID: 28253424; PMCID: PMC6464099. doi:10.1002/14651858.CD006499.pub4
4. Scott AB. Botulinum toxin injection of eye muscles to correct strabismus. Trans Am Ophthalmol Soc. 1981;79:734–770. PMID: 7043872; PMCID: PMC1312202.
5. Al Taisan A, Al Shamlan F, Al Mulhim A, Alsomali I, Al Owaifeer A. Botulinum toxin; indications, success rates and complications in the management of horizontal strabismus in Saudi Arabia. J Clin Ophthalmol. 2018;2(1). doi:10.35841/clinical-ophthalmology.2.1.32-37
6. Alshamlan FT, Al Abdulhadi HA, Alwalmany MM, Alotaibi KS. The efficacy of dose increments of botulinum toxin a in the treatment of childhood esotropia. Clin Ophthalmol. 2021;15:113–120. PMID: 33469257; PMCID: PMC7811462. doi:10.2147/OPTH.S294396
7. de Alba Campomanes AG, Binenbaum G, Campomanes Eguiarte G. Comparison of botulinum toxin with surgery as primary treatment for infantile esotropia. J AAPOS. 2010;14(2):111–116. PMID: 20451851. doi:10.1016/j.jaapos.2009.12.162
8. Gursoy H, Basmak H, Sahin A, Yildirim N, Aydin Y, Colak E. Long-term follow-up of bilateral botulinum toxin injections versus bilateral recessions of the medial rectus muscles for treatment of infantile esotropia. J AAPOS. 2012;16(3):269–273. PMID: 22681945. doi:10.1016/j.jaapos.2012.01.010
9. AlShammari S, Alaam M, Alfreihi S. Conventional surgery versus botulinum toxin injections for partially accommodative esotropia. J AAPOS. 2022;26(1):
10. Scott AB, Magoon EH, McNeer KW, Stager DR. Botulinum treatment of childhood strabismus. Ophthalmology. 1990;97(11):1434–1438. PMID: 2255516. doi:10.1016/s0161-6420(90)32390-4
11. Speeg-Schatz C, Burgun P, Gottenkiene S. To what extent may Botulinum toxin type A injections be an alternative choice to surgery in infantile esotropia? Eur J Ophthalmol. 2017;27(3):285–288. PMID: 28362053. doi:10.5301/ejo.5000947
12. Abbasoglu OE, Sener EC, Sanac AS. Factors influencing success and dose-effect relation of botulinum A treatment. Eye. 1996;10(3):385–391. PMID: 8796167. doi:10.1038/eye.1996.78
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
