Back to Journals » Medical Devices: Evidence and Research » Volume 12
Comparison Of Digital Manometer And Water Column Manometer Pressures Measurements During Lumbar Puncture
Authors Sekhri NK , Parikh S, Weber GM
Received 2 August 2019
Accepted for publication 4 October 2019
Published 29 October 2019 Volume 2019:12 Pages 451—458
DOI https://doi.org/10.2147/MDER.S225757
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Nitin K Sekhri,1,2 Shalvi Parikh,1 Garret M Weber1,2
1Department of Anesthesiology, Westchester Medical Center, Valhalla, New York, USA; 2Department of Anesthesiology, New York Medical College, Valhalla, New York, USA
Correspondence: Nitin K Sekhri
Department of Anesthesiology, Westchester Medical Center, 100 Woods Road, Macy Suite W228, Valhalla, NY 10595, USA
Tel +1 9144937693
Fax +1 9144937927
Email [email protected]
Background: Cerebrospinal fluid (CSF) pressure measurement is routinely performed via a conventional water column manometer. There is increasing interest in using a digital manometer in measuring CSF pressures. The aim of this study is to compare column and digital manometers, in addition to measuring time to acquire the pressure readings.
Research design and methods: This prospective study included 27 patients who were referred for a fluoroscopically guided lumbar puncture. Opening pressure and closing pressure measurements were done with a digital manometer and then a traditional water column manometer. The time to obtain each pressure measurement was also recorded and compared.
Results: Mean time to obtain pressure reading was significantly lower in the digital manometer group when compared to the water column manometer group (8.1 seconds vs. 42.2 seconds, P<0.05 for opening pressure and 8.92 seconds vs. 45.15 seconds, P<0.05 for closing pressure). Correlation between the opening pressure measurements (Pearson coefficient r= 0.98) and closing pressure (Pearson coefficient r= 0.89) was strong. However, the digital manometer reading consistently read higher.
Conclusion: Digital manometry during an LP yielded is faster however there might be a clinical difference between the devices. Clinicians must be careful in using the device across all cases.
Keywords: lumbar puncture, opening pressure, closing pressure, IIH, idiopathic intracranial hypertension, normal pressure hydrocephalus, digital manometer
Introduction
The lumbar puncture (LP) was first described in the late 1890s by Dr. Heinrich Irenäus Quincke and continues to be an essential procedure for both diagnostic and therapeutic purposes.1–3
The indications for LP vary but include investigation to diagnose subarachnoid hemorrhage, meningitis, neurological disorders which include demyelinating disorders such as multiple sclerosis, as well as managing and diagnosing disorders of intracranial pressure, such as idiopathic intracranial hypertension (IIH) and normal pressure hydrocephalus.2,3 The opening pressure (OP) in particular has been proven to correlate and serve as a reliable marker for intracranial pressure, thus, can be critical in the diagnoses of many diseases.4 In some instances, such as with idiopathic intracranial hypertension and NPH, the diagnosis can be made or confirmed by OP alone.5–7
As such, the OP measurement is a crucial part of the LP, and accuracy of the OP measurement is paramount.8 Additionally, often for diagnostic and therapeutic purposes, the closing pressure (CP) is taken immediately after the necessary CSF is collected and prior to removal of the needle from the intrathecal space.9
Traditionally, a water column manometer is used for pressure measurement during the LP procedure. However, using a standard water column manometer carries some disadvantages: first, pressure reading can be time-consuming; second, these manometers are bulky in size, therefore require manual dexterity for stability and sometimes one may require two people during measurement; third measurements may easily be altered by the position of the manometer. As such, a disposable digital pressure transducer, the Compass device (Centurion Medical Products, Williamston, MI), is available for direct measurement and monitoring of pressures during LP.10 For central venous catheter placement, a similar compact digital pressure-measuring device was shown to be safe, simple with improved provider satisfaction and less cumbersome than traditional manometry methods (including water column manometry) to confirm venous access.11 However, the authors were not able to identify any research in the literature regarding its utilization during LP.
After using the Compass device for several pressure readings during LPs, the authors reasoned that the digital device allows for CSF readings with significant procedural time reduction. However, there is a scarcity of data on the use of the product for LP pressure measurement. The purpose of this study compared the digital device with the standard of care water column manometry.
Patients And Methods
Approval was obtained and overseen by from New York Medical College institutional review board before the study commenced. All patients provided written informed consent before undergoing study procedures. This study was performed in compliance with the Health Insurance Portability and Accountability Act along with adhering to the principles of Good Clinical Practice and the Declaration of Helsinki.
Patients presenting for fluoroscopic-guided LPs were asked to participate in this prospective study. Written consent was obtained for both procedure and for research study. Patients were positioned in the left lateral decubitus position with slight cervical spine flexion and with knees slightly drawn to their chest as per normal practice for obtaining accurate pressures during lumbar puncture.2,5,12–14 Using sterile technique, a 20-gauge Quincke needle was advanced into the subarachnoid space under fluoroscopic guidance. The L4–5 interspace was the first site of attempt, but if based on imaging, was deemed to be difficult, the L3–4 interspace was then used. Four pressure measurements were then obtained during the procedure. First, an OP using the digital device (OPD), then an OP measured using the water column manometer (OPC). CP also obtained in a similar manner, obtaining the CP first for the digital device (CPD) and then the water column manometer (CPC). Measurements obtained using the digital device were in accordance with the manufacturer’s directions when the measurement stabilized on the display screen after successful calibration, removal of luer cap and stabilization of pressure for 2–3 s.15 The pressure measurements with the water column manometer were done in accordance with good practice.16 The measurements were taken by connecting the needle directly (without tubing) to the manometer via a 4-way stopcock while the patient was in the lateral decubitus. The patient was encouraged to relax, breath normally and not Valsalva. The manometer was kept level with the hub, and the pressure was measured when the CSF meniscus stopped rising and respiratory fluctuations were apparent. All pressures were recorded in cmH2O (see Figure 1 for an example of pressure measurements using the two devices).
Time (in seconds) to obtain each measurement was also recorded as Time for OPD, Time for OPC, Time for CPD and T for CPC.
Basic Demographics of the patients were also recorded, such as gender, height, weight (and thus body mass index) and indication for the procedure.
Patients were excluded if they were unable to consent, a minor (age <18), hemodynamically unstable, required mechanical respiratory support, or patients with OP was above the limit of the water column manometer (56 cmH2O).
Statistical analysis was done using Excel (2016; Microsoft, Redmond, Washington). The digital times and water column manometer times differences were compared using a two sided-tailed paired t-test. To identify the differences in measurements between the digital and water column manometer, a Bland–Altman plot was generated comparing aggregate pressure (both closing and OPs), isolated OP and isolated CP.
Results
Twenty-seven patients were recruited to participate in the study. All of these patients were able to undergo LP with measurement of the four different pressure measurements as described in the materials and methods. Demographics and indications of each patient were recorded (Table 1). Infectious workup accounted for the most common indication (33%). IIH was a common indication accounting for 5 (19%) of the indications. These patients had a higher aggregate pressure as expected, with a mean of 25 cmH2O compared to 20 cmH2O for the rest of the patients.
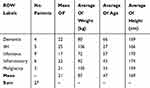 |
Table 1 Demographics And Indications For Referral For The Fluoroscopic LP Along With The Mean Opening Pressure Readings For Each Indication |
When comparing times to obtain the pressure readings, there was a significant difference seen across all pressures. See Table 2 for time comparisons of the water column manometer and the digital manometer.
 |
Table 2 Mean Pressure Readings (cmH2O) And Time (In Seconds) To Obtain Pressure Reading For Digital Manometer And Water Column Manometer With P-Values |
When comparing the OPs measured, there was a significant correlation between the two measurements, with a Pearson coefficient of 0.97 (Figure 2A) along with a strong correlation for CPs with a Pearson coefficient of 0.89 (Figure 2B). However, while there was strong correlation between the two devices, the digital device pressure reading was consistently above that measured by the water column manometer. The mean difference between the measurements was 1.85 cmH2O for OPs (Figure 3A), with the digital device commonly measuring above the water column manometer, and the mean difference for CP was 1.56 cmH2O (Figure 3B), again with the digital device reading above the water column manometer.
Discussion
As stated, prior, LPs are critical for the diagnosis and treatment of many disease processes. Pressure monitoring during the procedure is paramount and can be affected by many things such as patient body habitus particularly obesity, mechanical ventilation, pain, anxiety and position. It is very common, as was seen in this study, for patients to receive an LP for likely pressure-related disorders such as idiopathic intracranial hypertension. Accurate OP measurement is imperative in the diagnosis of idiopathic intracranial hypertension, and clinicians treating patients with this disorder must use everything in their armamentarium to ensure accurate diagnosis given the potentially risky treatment options such as CSF shunting.
While obtaining an accurate OP or CP is typically straightforward using traditional water column manometry, it is not uncommon for clinicians to experience time constraints due to special populations when trying to obtain pressure readings, such as the pediatric population, comatose patients or patients with delirium.17
Because of these special populations, it is understandable that clinician has sought out a more efficient way to measure pressures during these procedures, hence the growing utilization of digital manometry for the measurement of CSF pressure. As was seen in this study, the use of the digital Compass device can be incredibly efficient, with a reduction in measurement time by approximately 80%. However, clinicians must weigh the time saved to the additional cost of the digital device, which has a list price of approximately $59.95 per device. With over 300,000 LPs being done in the United States annually, the potential yearly cost of $18,000,000 to the already financially burdened United States health-care system must not be taken lightly.18
The use of the water column manometer has been tried and true for decades. The digital device did read higher a majority of the time, with an average of close to 2 cmH2O for OP. While this difference is likely not going to have much clinical impact in most patients, many patients are on the border of normal, as was seen in this study as well with an overall average OP being 21 cmH2O. It is critical that any clinician performing an LP utilizes the most accurate methodology to obtain a pressure; however, this method is not known. The speed of the digital device may be appealing, one must consider the accuracy particularly on borderline pressures since using the device one is straying from common medical practice.
The authors do note that the digital device did perform the first pressure for both OPs and CPs. This was done by design as the Compass device would likely utilize the least amount of CSF volume to obtain the pressure, <0.3mL, likely not affecting the water column manometers pressure; however, this may not be entirely true. The pressure may drop with this small decrease in CSF volume, accounting for the difference seen in this study of the pressures. However, one would expect the differences to be close to negligible at the CP measurements where the digital device still reads higher than that of the water column manometer on average making this finding likely a true finding. The pressures were obtained by 2 physicians, and interobserver variability was able to not studied which is an additional limitation to the study.
While vast more attention is paid to the OP, the CP remains an important measurement, particularly when treating idiopathic intracranial hypertension.19 When obtaining CPs, air entrapment often occurs, as was seen in every CP performed during this study with a water column manometer, making reading of the CP difficult (see Figure 4 as an example of air entrapped), but is an essential measurement to a therapeutic LP.20 This is likely a significant reason why there is less of a correlation between the two devices during CPs.
 |
Figure 4 Example of air (stars) being entrapped in water column manometer during closing pressure making pressure reading difficult. |
Conclusion
CSF pressure measurement during LP is critical for both diagnostic and therapeutic reasons. Particularly, this measurement can be difficult to obtain in certain populations, such as in pediatric patient populations and patients with altered mental status. Digital measurement with an electronic device can help decrease the amount of time it takes to obtain these measurements. Digital CSF pressure measurement with an electronic device obtains measurements highly correlating with standard water column manometer and can help decrease the amount of time it takes to obtain these measurements. However, further studies to confirm accuracy in a clinical setting along with analysis of the economic impact are needed before it becomes the standard of care.
Acknowledgment
The authors thank the administration and staff of the radiology department at Westchester Medical Center, Valhalla, NY along with Maureen Cooney, DNP for being a mentor.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Lee SC, Lueck CJ. Cerebrospinal fluid pressure in adults. J Neuroophthalmol. 2014;34(3):278–283. doi:10.1097/WNO.0000000000000155
2. Doherty CM, Forbes RB. Diagnostic lumbar puncture. Ulster Med J. 2014;83(2):93–102.
3. Sladky JH, Piwinski SE. Lumbar puncture technique and lumbar drains. Atlas Oral Maxillofac Surg Clin North Am. 2015;23(2):169–176. doi:10.1016/j.cxom.2015.05.005
4. Lenfeldt N, Koskinen LO, Bergenheim AT, Malm J, Eklund A. CSF pressure assessed by lumbar puncture agrees with intracranial pressure. Neurology. 2007;68(2):155–158. doi:10.1212/01.wnl.0000250270.54587.71
5. Avery RA. Interpretation of lumbar puncture opening pressure measurements in children. J Neuroophthalmol. 2014;34(3):284–287. doi:10.1097/WNO.0000000000000154
6. Mallery RM, Friedman DI, Liu GT. Headache and the pseudotumor cerebri syndrome. Curr Pain Headache Rep. 2014;18(9):446. doi:10.1007/s11916-014-0446-z
7. Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology. 2013;81(13):1159–1165. doi:10.1212/WNL.0b013e3182a55f17
8. Abel AS, Brace JR, McKinney AM, Harrison AR, Lee MS. Practice patterns and opening pressure measurements using fluoroscopically guided lumbar puncture. AJNR Am J Neuroradiol. 2012;33(5):823–825. doi:10.3174/ajnr.A2876
9. McLaren SH, Monuteaux MC, Delaney AC, Landschaft A, Kimia AA. How much cerebrospinal fluid should we remove prior to measuring a closing pressure? J Child Neurol. 2017;32(4):356–359. doi:10.1177/0883073816681352
10. Hulvershorn J 510(k) premarket notification. [
11. Togashi K, Nandate K, Hoaglan C, Sherman B, Bowdle A. A multicenter evaluation of a compact, sterile, single-use pressure transducer for central venous catheter placement. Anesth Analg. 2013;116(5):1018–1023. doi:10.1213/ANE.0b013e31828a6e53
12. Cauley KA. Fluoroscopically guided lumbar puncture. Am J Roentgenol. 2015;205(4):W442–W450. doi:10.2214/AJR.14.14028
13. Avery RA, Mistry RD, Shah SS, et al. Patient position during lumbar puncture has no meaningful effect on cerebrospinal fluid opening pressure in children. J Child Neurol. 2010;25(5):616–619. doi:10.1177/0883073809359198
14. Sithinamsuwan P, Sithinamsuwan N, Tejavanija S, Udommongkol C, Nidhinandana S. The effect of whole body position on lumbar cerebrospinal fluid opening pressure. Cerebrospinal Fluid Res. 2008. 5. 11-8454-5-11. doi:10.1186/1743-8454-5-11
15. Compass [package insert]. Williamston, michigan: Centurion medical products, Inc. 2016 Updated 2016.
16. Ozutemiz C, Rykken JB. Lumbar puncture under fluoroscopy guidance: a technical review for radiologists. Diagn Interv Radiol. 2019;25(2):144–156. doi:10.5152/dir.2019.18291
17. Jiraskova N, Rozsival P. Idiopathic intracranial hypertension in pediatric patients. Clin Ophthalmol. 2008;2(4):723–726. doi:10.2147/opth.s1593
18. Vickers A, Donnelly JP, Moore JX, et al. Epidemiology of lumbar punctures in hospitalized patients in the United States. PLoS One. 2018;13(12):e0208622. doi:10.1371/journal.pone.0208622
19. Fiorito-Torres F, Rayhill M, Perloff M. Idiopathic intracerebral hypertension (IIH)/pseudotumor: removing less CSF is best (P6. 209). Neurology. 2014;82(10 Supplement):
20. Hudgins PA, Fountain AJ, Chapman PR, Shah LM. Difficult lumbar puncture: pitfalls and tips from the trenches. AJNR Am J Neuroradiol. 2017;38(7):1276–1283. doi:10.3174/ajnr.A5128
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



