Back to Journals » Pharmacogenomics and Personalized Medicine » Volume 10
Comparison of CYP2C9, CYP2C19, CYP2D6, ABCB1, and SLCO1B1 gene-polymorphism frequency in Russian and Nanai populations
Authors Sychev DA, Shuev GN , Suleymanov SS, Ryzhikova KA , Mirzaev KB, Grishina EA, Snalina NE, Sozaeva ZA, Grabuzdov AM , Matsneva IA
Received 7 December 2016
Accepted for publication 4 March 2017
Published 31 March 2017 Volume 2017:10 Pages 93—99
DOI https://doi.org/10.2147/PGPM.S129665
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Martin Bluth
Dmitrij Alekseevitch Sychev,1 Grigorij Nikolaevich Shuev,1 Salavat Shejhovich Suleymanov,2 Kristina Anatol’evna Ryzhikova,3 Karin Badavievich Mirzaev,3 Elena Anatol’evna Grishina,3 Natalia Evgenievna Snalina,3 Zhannet Alimovna Sozaeva,3 Anton Mikhailovich Grabuzdov,4 Irina Andreevna Matsneva4
1Department of Internal Medicine and Clinical Pharmacology, Russian Medical Academy of Continuing Professional Education, Ministry of Healthcare, Moscow, 2Saiko Russian–Japanese Medical Center, Khabarovsk, 3Research Centre, Russian Medical Academy of Continuous Professional Education, Ministry of Healthcare, 4Department of General Medicine, Sechenov First Moscow State Medical University, Moscow, Russian Federation
Background: The efficiency and safety of drug therapy depends on the peculiarities of functioning of the P450 cytochrome group and transporting proteins. There are significant differences for single-nucleotide polymorphism (SNP) frequency.
Materials and methods: We studied the peculiarities of P450 cytochrome polymorphisms, SLCO1B1 transporting protein, and P-glycoprotein carriage in healthy volunteers in the Nanai ethnic group living in Russia, and compared them to the carriage of SNPs in the Russian population according to literature data.
Results: After performing the real-time polymerase chain reactions on the samples from 70 healthy volunteers from the Nanai group, for the CYP2C9*2C430T polymorphism we determined 70 CC-genotype carriers. As for the CYP2C9*3A1075C polymorphism, we found 62 AA-genotype carriers and eight AC-genotype carriers. For the CYP2C19*2G681A polymorphism, we determined 39 GG-genotype carriers and 28 GA-genotype carriers, for the CYP2C19*3G636A polymorphism 58 GG-genotype carriers and 12 GA-genotype carriers, and for the CYP2C19*17C806T polymorphism 67 CC-genotype carriers and three CT-genotype carriers. For the CYP2D6*4G1846A polymorphism, the GG genotype had 68 carriers, and the GA genotype two carriers. For the ABCB1*6C3435T polymorphism, there were 19 CC-genotype carriers and 39 CT-genotype carriers. For the SLCO1B1*5T521C polymorphism, the TT genotype had 41 carriers and the CT genotype 25 carriers. The distribution of genotypes fitted the Hardy–Weinberg equilibrium for all the polymorphisms, except those of CYP2C9*2. There were also significant differences in allele frequencies for some polymorphisms between the Nanais and the Russians.
Conclusion: In the Nanai population, there are polymorphisms connected with the decrease in safety and efficiency of drug therapy. Studying the ethnic differences might influence the determination of priority in the introduction of pharmacogenetic tests in clinical practice in different regions of Russia.
Keywords: pharmacogenetics, ethnicity, Asians, Europeans, SNP, P450 cytochrome, ethnic group, P-glycoprotein
Introduction
The efficacy and safety of pharmacological therapy depends on the peculiarities of absorption, metabolism, and excretion of the drugs. The metabolism of drugs is mostly determined by the effect of enzymes of the cytochrome P450 group. The best-known agents determining the absorption and excretion of drugs are solute carrier transporters and P-glycoprotein.1 The most clinically significant are genes encoding cytochrome P450 enzymes – CYP2C9, CYP2D6, CYP2B6, CYP3A4, CYP3A5, and CYP2C19 – which are responsible for the metabolism of almost half of all drug classes (antiplatelet, anticoagulant, antihypertensive, antianginal, lipid-lowering, antiarrhythmic, psychotropic, antidiabetic, antitumor, and other drugs) and genes encoding transport proteins: ABCB1 (P-glycoprotein) and SLCO1B1 (OATP1B1-transporter protein).2–4 Studying the influence of different single-nucleotide polymorphisms (SNPs) on the absorption, distribution, metabolism, and excretion of drugs may help in reducing the problems of the variability of drug responses, potentially resulting in a decrease in prevalence of treatment failure and adverse events.5 However, some SNP frequencies have significant variance in different ethnic groups. For example, CYP2C19*17 was 42- and 24-fold more frequent in Mediterranean–South Europeans and those from the Middle East than in East Asians (P<0.001, in both cases).6 That is why the study of polymorphic gene-carrier frequency is especially important for such a multinational country as Russia. There is a current insufficiency of studies on the prevalence of major pharmacogenetic predictive markers of increased drug sensitivity among the many indigenous ethnic groups. In the present research, we identified frequencies of some of the polymorphisms of genes CYP2C9, CYP2C19, CYP2D6, ABCB1, SLCO1B1 in the Nanai ethnic group (the Nanai is a small native population in the Russian Far East, living along the middle reaches of the Amur River Valley).7
Materials and methods
Sample
A total of 70 healthy volunteers (14 men [20%] and 56 women [80%]) with an average age of 43.5 (22–70) years living in Khabarovsk territory in the Russian Far East were engaged in the research. All the volunteers were informed about the objectives and methods of the research. They also gave informed consent to participate in the research and provided the researchers the right to extract their genetic material. The study was approved by the local ethical committee of the Russian Medical Academy of Continuing Professional Education (record 12, December 8, 2015). Written consent was obtained from all study participants. The criteria for inclusion were no consanguinity among the analyzed individuals and belonging to the Nanai ethnic group, which was determined by volunteers’ and their parents’ self-identification.8 The criteria for exclusion were relatives and descendants of other ethnic groups.
Sample preparation
A 5 mL sample of each volunteer’s blood was extracted to determine the SNPs. This was put into vacuum tubes with ethylenediaminetetraacetic acid. Extraction was executed in December 2015 at the Troitskaya Central District Hospital clinic of the Ministry of Healthcare of Khabarovsk territory in Najhin village. The frozen samples were delivered to the Russian Medical Academy of Continuous Professional Education research center in Moscow, where DNA was extracted from the leukocytes.
The extracted DNA was tested for carriage of the SNPs CYP2C9*2C430T rs1799853, CYP2C9*3А1075С rs1057910, CYP2C19*2G681A rs4244285, CYP2C19*3G636A rs4986893 or rs57081121, CYP2C19*17C806T rs12248560, CYP2D6*4G1846A rs3892097, ABCB1*6C3435T rs1045642, and SLCO1B1*5T521C rs4149056 using real-time polymerase chain reaction with the help of a commercial set provided by Syntol (Moscow, Russia) and a CFX96 Touch (Bio-Rad Laboratories, Hercules, CA, USA). The program included preliminary denaturation at 95°C, which lasted 3 minutes, then 40 cycles of 15 seconds’ denaturation at 95°C, then annealing at 63°C for 40 seconds. We used Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines for interpretation of genotypes.9–11
CYP2C9
The carriers of the *1/*1 genotype were designated extensive metabolizers, carriers of the CYP2C9*2 and CYP2C9*3 alleles in a heterozygous state (*1/*2, *1/*3) designated intermediate metabolizers, and those carrying both the alleles simultaneously (*2/*3) poor metabolizers.9
CYP2C19
Carriers of the *1/*1 genotype were designated extensive metabolizers, with two alleles of CYP2C19*2 or CYP2C19*3 (*2/*2, *2/*3, *3/*3) poor metabolizers, and those carrying CYP2C19*2 or CYP2C19*3 or carrying CYP2C19*17 with one allele of CYP2C19*2 (*1/*2, *1/*3, *2/*17) intermediate metabolizers. Carriers of CYP2C19*17 alleles in homozygous and heterozygous states (*1/*17, *17/*17) were designated ultrarapid metabolizers.10
CYP2D6
Carriers of *1/*1 and *1/*4 genotypes were designated extensive metabolizers, and those with the CYP2D6*4 allele in a homozygous state (*4/*4) poor metabolizers.10
ABCB1 (C435T)
Carriers of the CC genotype have a “normal activity” transporter. The T allele is associated with abnormality pharmacokinetics.12
SLCO1B1
Carriers of *1/*1 genotype have a “normal activity” transporter; SLCO1B1*5 allele in heterozygous state (*1/*5) – “intermediate activity”; *5/*5 homozygotes – “low activity”.11
Comparison group
A population of Russians was chosen as the comparison group, as this is the largest ethnic group in Russia. The control group was arranged according to data in the literature (we used PubMed as the main source), with high priority given to research on healthy volunteers. If there were no groups of healthy volunteers, the priority was given to the research with large numbers of patients. Groups with insignificant differences in allele frequencies on Hardy–Weinberg equilibrium were involved in the research.
Statistical analysis
We performed Hardy–Weinberg tests to confirm the independence of allele distribution in studied polymorphisms. Fisher’s exact test was used to estimate differences between frequencies of allele mutations of Russian and Nanai ethnic groups. Statistical data were processed using InStat software. P<0.05 was considered statistically significant for all tests.
Results
We determined polymorphisms of CYP2C19, CYP2C9, CYP2D6, ABCB1, and SLCO1B1 of 70 healthy volunteers from the Nanai ethnic group. For the CYP2C9 gene, we discovered zero frequency of the T allele of the CYP2C9*2C430T polymorphism, so it was impossible to calculate χ2 value for Hardy–Weinberg proportions, and 5.7% frequency of the C allele of the CYP2C9*3А1075С polymorphism.
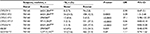
For the CYP2C19 gene, frequency of the A allele of the CYP2C19*2G681A polymorphism was 24.3%, frequency of the A allele of the CYP2C19*3G636A polymorphism was 8.6%, frequency of the T allele of the CYP2C19*17C806T polymorphism was 2.1%. For the CYP2D6 gene, frequency of the A allele of the CYP2D6*4G1846A polymorphism was 1.4%. For the ABCB1 gene, frequency of the T allele of the ABCB1*6C3435T polymorphism was 45%. The frequency of the C allele of the SLCO1B1*5T521C polymorphism was 23.6%. Genotype frequencies did not deviate significantly from Hardy–Weinberg equilibrium. The results are presented in Table 1.
We compared the frequency of alleles in the Nanai ethnic group to frequency in the Russian group, and the results are presented in Table 2. We did not discover any significant differences in frequency of the CYP2C9*3, ABCB1, or SLCO1B1*5 polymorphism between Nanais and Russians. However, polymorphisms of the CYP2C19 gene were found with significantly different frequency: the CYP2C19*2 polymorphism was found more often in the Nanai group (24.3% vs 12.3% in the Russian population, P=0.0002); CYP2C19*3 was also found more often in the Nanai group (8.3% vs 0.3% in the Russian population, P<0.0001); and CYP2C19*17 was found more often in the Russian group (27.3% vs 2.1% in the Nanai group, P<0.0001). Besides, the CYP2D6*4 polymorphism was found significant more rarely in the Nanai group than in the Russian one – 1.4% vs 17.4%. We made a likely functional characteristic of cytochrome activity for the Nanai and Russian populations for CYP2C19, CYP2C19 and CYP2D6 using CPIC guidelines (Table 3).9,10
  | Table 3 Likely phenotypes in Nanai and Russian ethnic groups Note: We used CPIC guidelines for interpretation of pharmacogenetic information.9,10 Abbreviations: CPIC, Clinical Pharmacogenetics Implementation Consortium; EM, extensive metabolizer; IM, intermediate metabolizer; PM, poor metabolizer; UM, ultrarapid metabolizer. |
Discussion
It is known that drug dosages are different for different ethnic groups. For example, the maximum recommended dose for 32% of medicines registered in the period 2001–2007 in the US was nearly twice that of the recommended dose of these drugs in Japan.13 Proteins of cytochrome P450, as well as transport proteins, play a key role in the metabolism and transport of drugs. Knowledge of the prevalence of polymorphisms of genes encoding these proteins among different ethnic groups will help to increase drug efficacy and reduce the number of adverse drug reactions. This might help in determination of priorities in the introduction of pharmacogenetic testing to clinical practice in different regions of Russia, and could also reveal the peculiarities of prevalence of genetic predictors of heightened race/ethnic sensitivity to drugs.
There are a lot of native ethnic groups living in Russia comprising Asians and Caucasians. Studying the carriage of mutant alleles in different populations seems to be up to date, as far as optimization of the implementation of pharmacogenetic testing in clinical practice in different regions of Russia is concerned. Today, we have some data about the existence of polymorphisms in the Yakut population, a large ethnic group living in the Asian part of Russia; it is known that the frequency of CYP2C19*2 is 18.1%, CYP2C19*3 3.1%, CYP2C9*2 5.1%, CYP2C9*3 6.7%, SLCO1B1*5 14%, and VKORC1G1639A 83.2%.14,15 Tatars and Bashkirs, ethnic groups living in the European part of Russia, have frequencies of CYP2C9*2 of 5.1% and 6%, CYP2C9*3 of 5.4% and 6.2%, and CYP2D6*4 of 9.5% and 7.1%, respectively.16,17 The Nenets have a frequency of CYP2D6*4 of 7.3%.18 However, we do not have any pharmacogenetic data for many ethnic groups in Russia, and we do not have such data for the Nanai people. We compared this to the frequency of the alleles of the studied polymorphisms in the Russian ethnic group.
CYP2C9
The CYP2C9*2 polymorphism was not present in this sample, so χ2 by Hardy–Weinberg was not calculated. In the Russian population, the frequency of this polymorphism was 11%. The frequency of the CYP2C9*3 polymorphism in the Nanai population was 5.7% vs 5.8% in Russian population, but differences were not significant (P=1; Table 2). The differences in likely phenotypes of the CYP2C9 gene were found, ie, slow metabolizers (intermediate metabolizer + poor metabolizer) were significantly rarer among the Nanai population: 2.7 times less than in the Russian population (odds ratio [OR] 0.28, 95% confidence interval [CI] 0.1–0.6; P=0.0003; Table 3). Peculiarities in ethnic differences in frequency of CYP2C9*2 and CYP2C9*3 polymorphisms have been described in the literature as Caucasians in Europe (12.1%–14.7% and 6.2%–8.4%) and Asians (0.6%–7.3% and 3.4%-11.7%), respectively.19 Today, there are dosing guidelines by the CPIC and Dutch Pharmacogenetics Working Group (DPWG) for pharmacogenetic testing on the CYP2C9 gene for the personalization of anticoagulant therapy, hypoglycemic therapy, and for some other drugs.20
CYP2C19
According to the results of the research, the frequency of the CYP2C19*2, CYP2C19*3, and CYP2C19*17 polymorphisms in the Nanai ethnic group (24.3%, 8.6%, and 2.1%, respectively) significantly differed from that in the Russian ethnic group. Polymorphisms associated with slow activity (CYP2C19*2 and CYP2C19*3) were found 1.9 (P=0.0002) and 28.6 (P<0.0001) times, respectively, more often in the Nanai population, and the CYP2C19*17 polymorphism, associated with accelerated metabolism, was found 12.9 (P<0.0001) times more rarely (Table 2). Moreover, the “slow” (IM + PM)-likely phenotypes were found 2.1 times (OR 3.7, 95% CI 2.3–6.1; P<0.0001) more often and a “fast”-likely phenotype (ultrarapid metabolizer) found 28.4 times more rarely (OR 0.02, 95% CI 2.3–6.1; P<0.0001) in the Nanai group (Table 3). There are some ethnic differences in known polymorphism frequency, eg, Caucasians have frequencies of CYP2C19*2, CYP2C19*3, CYP2C19*17 of 13.3%–16.2%, 0.1%–0.6%, and 20.1%–42%, and Asians of 18.5%–30.3%, 0.5%–6.9%, and 0.96%–13.7%, respectively.6 Today, there are dosing guidelines from the CPIC and DPWG on pharmacogenetic testing on the CYP2C19 gene for the personalization of clopidogrel, antidepressants, proton-pump inhibitors, and other drug therapies.21
CYP2D6
We studied the CYP2D6*4 polymorphism, which was found 12.2 times more rarely in the Nanai population than in the Russian one (P<0.0001; Table 2). However, we did not find significant differences in likely phenotypes between the Russians and the Nanais (OR 0.19, 95% CI 0.01–3.1; P=0.15; Table 3). There are ethnic differences in polymorphism frequencies, eg, Caucasians have CYP2D6*4 frequency of 18.5%–26.3% and Asians 0.42%–7.7%.22 Today there are dosing guidelines from the CPIC, DPWG, and Canadian Pharmacogenomics Network for Drug Safety on pharmacogenetic testing on the CYP2D6 gene for the personalization of tamoxifen, narcotic analgesics, antipsychotics, and some other drug therapies.23
ABCB1C3435T
Of the Nanais studied, 45% percent had the T allele, the same as in the Russian population(P=0.059; Table 2). According to the literature, the frequency of the T allele in Caucasian and Asian populations is about 50% for each.24 Today, there are no dosing guidelines from the CPIC, European Medicines Agency, or DPWG on using the ABCB1*6C3435T polymorphism for personalizing therapy for patients, but there has been research devoted to the influence of this SNP on the pharmacokinetics of clopidogrel.12
SLCO1B1
We studied the frequency of SLCO1B1*5: this was 23.6% in the Nanais vs 21.8% in Russian population (P=0.69; Table 2). There are some ethnic differences in known polymorphism frequency, eg, the frequency of SLCO1B1*5 in Europe is 14%–23%, while in Asia it is less than 10%.27 Today, there are dosing guidelines from the CPIC on pharmacogenetic testing for the personalization of statin therapy.28
Restrictions of the research
In our research, we compared the frequency of CYP2C9*2C430T, CYP2C9*3А1075С, CYP2C19*2G681A, CYP2C19*3G636A, CYP2C19*17C806T, CYP2D6*4G1846A, ABCB1*6C3435T, and SLCO1B1*5T521C polymorphisms in Nanai and Russian ethnic groups. It was impossible to check the frequency of the CYP2C9*2C430T polymorphism against Hardy–Weinberg equilibrium, so we did not compare the frequency of its mutant alleles in Russian or Nanai groups. The Nanai group consisted of healthy volunteers, living on the territory historically occupied by this ethnic group. We chose Russian as the comparison group, as it is the largest ethnic group in the Russian Federation. We sought data on the frequency of the polymorphisms studied, and found two studies on Russian volunteers. The first focused on the CYP2C9*2C430T, CYP2C9*3А1075С, CYP2C19*2G681A, CYP2C19*3G636A, CYP2D6*4G1846A, and ABCB1*6C3435T polymorphisms (European part of Russia).29 The second focused on CYP2C9*2C430T, CYP2C9*3А1075С, CYP2C19*2G681A, and CYP2D6*4G1846A (European part of Russia).27 We combined the data, but neither the first nor the second study provided information on the CYP2C19*17C806T and SLCO1B1*5T521C polymorphisms. Moreover, we did not find any publications devoted to studying these SNPs among Russian volunteers, so we tried to use only the data of the research with maximal patient numbers where distribution by Hardy–Weinberg equilibrium was not significant. Patients from Moscow with stomach ulcers were included by the CYP2C19*17C806T polymorphism, with χ2 by Hardy–Weinberg of 1.12 (P=0.29).28 Patients from Moscow with hyperlipidemia were included by the SLCO1B1*5T521C polymorphism, with χ2 by Hardy–Weinberg of 2.8 (P=0.09).15
Conclusion
We found CYP2C9*3А1075С, CYP2C19*2G681A, CYP2C19*3G636A, CYP2C19*17C806T, CYP2D6*4G1846A, ABCB1*6C3435T, and SLCO1B1*5T521C polymorphisms in the Nanai ethnic group. Patients carrying these polymorphisms require a much more careful approach in choosing drug therapy, due to severe adverse reactions. Moreover, there are significant differences in the carrying of some polymorphisms between the Russians and the Nanais. Data obtained from this study will help to assess the priority of implementation of genotyping in the region. We must study the prevalence of the other polymorphisms among the Nanais and also estimate the frequency of the polymorphisms in other ethnic groups in Russia.
Acknowledgments
The authors are grateful to ES Il’ina, at the Russian Medical Academy of Postgraduate Education, Ministry of Health of the Russian Federation for assistance in the manuscript preparation. This work was supported by the Russian Science Foundation (project 16-15-00227: “Fundamental research and exploratory research in priority areas of research”.)
Disclosure
The authors report no conflicts of interest in this work.
References
Almazroo OA, Miah MK, Venkataramanan R. Drug metabolism in the liver. Clin Liver Dis. 2017;21(1):1–20. | ||
Maier CL, Duncan A, Hill CE. Pharmacogenetics in oral antithrombotic therapy. Clin Lab Med. 2016;36(3):461–472. | ||
Valdes R Jr, Yin DT. Fundamentals of pharmacogenetics in personalized, precision medicine. Clin Lab Med. 2016;36(3):447–459. | ||
Weber WW. Pharmacogenetics: from description to prediction. Clin Lab Med. 2008;28(4):499–511. | ||
Yasmina A, Deneer VH, Maitland-van der Zee AH, van Staa TP, de Boer A, Klungel OH. Application of routine electronic health record databases for pharmacogenetic research. J Intern Med. 2014;275(6):590–604. | ||
Fricke-Galindo I, Céspedes-Garro C, Rodrigues-Soares F, et al. Interethnic variation of CYP2C19 alleles, ‘predicted’ phenotypes and ‘measured’ metabolic phenotypes across world populations. Pharmacogenomics J. 2016;16(2):113–123. | ||
Korshunova N, Katsuyama H, Demura M, et al. Posttraumatic stress disorders in the Nanai after pollution of the Amur River: ethnocultural analysis. Environ Health Prev Med. 2013;18(6):485–493. | ||
Tang H, Quertermous T, Rodriguez B, et al. Genetic structure, self-identified race/ethnicity, and confounding in case-control association studies. Am J Hum Genet. 2005;76(2):268–275. | ||
Caudle KE, Rettie AE, Whirl-Carrillo M, et al. Clinical Pharmacogenetics Implementation Consortium guidelines for CYP2C9 and HLA-B genotypes and phenytoin dosing. Clin Pharmacol Ther. 2014;96(5):542–548. | ||
Hicks JK, Bishop JR, Sangkuhl K, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline for CYP2D6 and CYP2C19 genotypes and dosing of selective serotonin reuptake inhibitors. Clin Pharmacol Ther. 2015;98(2):127–134. | ||
Ramsey LB, Johnson SG, Caudle KE, et al. The Clinical Pharmacogenetics Implementation Consortium guideline for SLCO1B1 and simvastatin-induced myopathy: 2014 update. Clin Pharmacol Ther. 2014;96(4):423–428. | ||
Karaźniewicz-Łada M, Danielak D, Rubiś B, et al. Impact of common ABCB1 polymorphism on pharmacokinetics and pharmacodynamics of clopidogrel and its metabolites. J Clin Pharm Ther. 2015;40(2):226–231. | ||
Arnold FL, Kusama M, Ono S. Exploring differences in drug doses between Japan and Western countries. Clin Pharmacol Ther. 2010;87(6):714–720. | ||
Vasilyev FF, Danilova DA, Kaimonov VS, Chertovskih YV, Maksimova NR. Frequency distribution of polymorphisms of CYP2C19, CYP2C9, VKORC1 and SLCO1B1 genes in the Yakut population. Res Pharm Sci. 2016;11(3):259–264. | ||
Sychev DA, Shuev GN, Chertovskih JV, Maksimova NR, Grachev AV, Syrkova OA. The frequency of SLCO1B1*5 polymorphism genotypes among Russian and Sakha (Yakutia) patients with hypercholesterolemia. Pharmgenomics Pers Med. 2016;9:59–63. | ||
Korytina G, Kochetova O, Akhmadishina L, Viktorova E, Victorova T. Polymorphisms of cytochrome P450 genes in three ethnic groups from Russia. Balkan Med J. 2012;29(3):252–260. | ||
Mustafina OE, Tuktarova IA, Karimov DD, Somova RS, Nasibullin TR. [CYP2D6, CYP3A5, and CYP3A4 gene polymorphism in Russian, Tatar, and Bashkir populations]. Genetika. 2015;51(1):109–119. Russian. | ||
Duzhak T, Mitrofanov D, Ostashevskii V, et al. Genetic polymorphisms of CYP2D6, CYP1A1, GSTM1 and p53 genes in a unique Siberian population of tundra Nentsi. Pharmacogenetics. 2000;10(6):531–537. | ||
Céspedes-Garro C, Fricke-Galindo I, Naranjo ME, et al. Worldwide interethnic variability and geographical distribution of CYP2C9 genotypes and phenotypes. Expert Opin Drug Metab Toxicol. 2015;11(12):1893–1905. | ||
PharmGKB. Gene: CYP2C9. Available from: https://www.pharmgkb.org/gene/PA126. Accessed March 9, 2017. | ||
PharmGKB. Gene: CYP2C19. Available from: https://www.pharmgkb.org/gene/PA124. Accessed March 9, 2017. | ||
Llerena A, Naranjo ME, Rodrigues-Soares F, Penas-Lledó EM, Fariñas H, Tarazona-Santos E. Interethnic variability of CYP2D6 alleles and of predicted and measured metabolic phenotypes across world populations. Expert Opin Drug Metab Toxicol. 2014;10(11):1569–1583. | ||
PharmGKB. Gene: CYP2D6. Available from: https://www.pharmgkb.org/gene/PA128. Accessed March 9, 2017. | ||
Ameyaw MM, Regateiro F, Li T, et al. MDR1 pharmacogenetics: frequency of the C3435T mutation in exon 26 is significantly influenced by ethnicity. Pharmacogenetics. 2001;11(3):217–221. | ||
Pasanen MK, Neuvonen PJ, Niemi M. Global analysis of genetic variation in SLCO1B1. Pharmacogenomics. 2008;9(1):19–33. | ||
PharmGKB. Gene: SLCO1B1. Available from: https://www.pharmgkb.org/gene/PA134865839. Accessed March 9, 2017. | ||
Gaikovitch EA, Cascorbi I, Mrozikiewicz PM, et al. Polymorphisms of drug-metabolizing enzymes CYP2C9, CYP2C19, CYP2D6, CYP1A1, NAT2 and of P-glycoprotein in a Russian population. Eur J Clin Pharmacol. 2003;59(4):303–312. | ||
Gra O, Mityaeva O, Berdichevets I, et al. Microarray-based detection of CYP1A1, CYP2C9, CYP2C19, CYP2D6, GSTT1, GSTM1, MTHFR, MTRR, NQO1, NAT2, HLA-DQA1, and AB0 allele frequencies in native Russians. Genet Test Mol Biomarkers. 2010;14(3):329–342. | ||
Sychev DA, Denisenko NP, Sizova ZM, Grachev AV, Velikolug KA. The frequency of CYP2C19 genetic polymorphisms in Russian patients with peptic ulcers treated with proton pump inhibitors. Pharmgenomics Pers Med. 2015;8:111–114. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.