Back to Journals » ClinicoEconomics and Outcomes Research » Volume 13
Comparison of Consistency, Feasibility, and Convenience of a Novel Compact System for Assessing Lung Volumes and Carbon Monoxide Diffusing Capacity versus Whole Body Plethysmography
Authors Dal Negro RW , Turco P, Povero M
Received 19 April 2021
Accepted for publication 18 June 2021
Published 7 July 2021 Volume 2021:13 Pages 637—643
DOI https://doi.org/10.2147/CEOR.S316529
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Giorgio Colombo
Roberto W Dal Negro,1 Paola Turco,2 Massimiliano Povero3
1National Centre for Respiratory Pharmacoeconomics and Pharmacoepidemiology, Verona, Italy; 2Research & Clinical Governance, Verona, Italy; 3AdRes Health Economics and Outcome Research, Torino, Italy
Correspondence: Massimiliano Povero
AdRes Health Economics and Outcome Research, Torino, Italy
Email [email protected]
Background: The MiniBox+™ is an innovative technique for assessing lung volumes (LVs) and the diffusing capacity of the lung for carbon monoxide (DLco). Differently from the equipment needed for whole body plethysmography (WBP), the MiniBox+ is a small, transportable instrument, which derives total lung capacity (TLC) during tidal breathing by analyzing gas pressures and airflows immediately preceding and immediately following airway occlusions.
Aim: To compare the consistency and the feasibility of LV and DLco measurements between the two instruments in different lung function disorders, and their cost of execution.
Methods: Consecutive patients of both genders with obstructive and restrictive respiratory disorders were randomly recruited. LVs and DLco were measured by a randomized sequence. The failure risk, number of attempts to achieve the first reliable measurement, corresponding time spent, and costs per patient were compared.
Results: A total of 134 patients were enrolled: 42 asthmatics (32.1%), and 47 patients with obstructive (35.1%) and 44 with restrictive respiratory disorders (32.8%). The overall failure risk was 19.4% for WBP and 8.2% for the MiniBox+ (risk ratio=0.417, 95% CI 0.242 to 0.72). LVs and DLco values proved equal with both techniques, regardless of the patients’ age, sex, schooling level, and initial lung disorder. Number of attempts and total time spent in achieving the first reliable measurement were significantly lower with the MiniBox+. Mean cost per patient was € 87.58 with WBP and € 75.11 with the MiniBox+, with a mean saving of € 12.33 (95% CI 5.93 to 18.73), mainly due to the saving in productivity loss.
Conclusion: LV and DLco measurements with the MiniBox+ were highly consistent with those obtained with WBP. The MiniBox+ proved easier to use (lower failure risk) and more convenient (lower execution costs) than WBP.
Keywords: economic impact, lung volumes, CO diffusing capacity, failure risk, whole body plethysmography, MiniBox+™
Introduction
The assessment of lung volumes (LVs) and the diffusing capacity of the lung for carbon monoxide (DLco) variably contribute in characterizing the pathophysiological pathways of different respiratory condition in clinical practice.1–7 Whole body plethysmography (WBP) is currently regarded as the gold standard; however, the utilization of this consolidated method has some critical aspects. Its widespread use for clinical purposes (including clinical trials) is affected by some limiting factors, such as the volume and immovability of this equipment, the complexity of maneuvers required to obtain reliable measurements; the high degree of patient compliance required, the routine maintenance needed for its appropriate use,2,8 and its intrinsic cost.
The MiniBox+™ (PulmOne Advanced Medical Devices, Ra’ananna, Israel) is an alternative and innovative technique. This novel device has been approved by the Food and Drug Administration but is not yet included in the European Respiratory Society and American Thoracic Society (ERS/ATS) Guidelines.4 In contrast to the whole body plethysmograph, the MiniBox+ is a small and transportable instrument that does not involve a closed box and does not require any complex maneuvers to take measurements.9 It derives total lung capacity (TLC) during tidal breathing by the analysis of gas pressures and airflows immediately preceding and immediately following airway occlusions.9
A multinational study carried out in Europe and the USA, published in 2021, compared for the first time the TLC obtained by the MiniBox™ with that by WBP in the same adult patients.9 Healthy individuals, and patients with obstructive and restrictive respiratory disorders, were investigated. No significant differences were found between the absolute values of TLC obtained with the two techniques. Moreover, results obtained in the whole sample were also confirmed in patients from each of the five centers contributing to this international study.9
In addition to absolute LVs, both WBP and the MiniBox+ allow the measurement of DLco, based on the same single-breath principle for single-breath carbon monoxide uptake in the lung.4 At present, any comparison between DLco values obtained with these two techniques is still lacking.
The aim of this study was to compare the consistency and feasibility of LV and DLco measurements carried out by means of the WBP and the MiniBox+ techniques in different lung function disorders, together with their economic impact. In particular, the primary objective was to compare the failure risk in LV and DLco measurements between the two techniques, while secondary objectives were to compare their consistency and their execution costs.
Materials and Methods
Consecutive patients of both genders suffering from obstructive (ie bronchial asthma and chronic obstructive pulmonary disease [COPD]) and restrictive respiratory disorders were randomly recruited during the period March–August 2018. At recruitment, each subject was requested to provide his or her informed consent to the measurements and to the anonymous use of their data for research purposes. Patients’ characteristics, including body mass index (BMI), smoking status, and schooling level, were also collected.
Only patients who did not provide (or refused to sign) their informed consent, and those with severe physical or cognitive limitations that made any instrumental procedures impossible, were excluded.
After careful instruction and demonstration, LV measurements were taken according to the ERS/ATS guidelines2,4 by two skilled and trained technicians, under the supervision of the pneumologist. Each patient underwent both the WBP (Plethysmography Platinum DX Elite, MedGraphics, USA) and the MiniBox+ (PulmOne Advanced Medical Devices, Ra’ananna, Israel) measurements of their basal LVs on the same day (with a 1-hour interval), in a random sequence, at the Lung Unit of the Specialist Centre – CEMS, Verona, Italy. Parameters collected were: forced expiratory volume in 1 second (FEV1), TLC, and residual volume (RV).
DLco was also measured, in accordance with the specific standards for single-breath carbon monoxide uptake in the lung.4 Before beginning the test, the maneuvers were demonstrated and the subject was carefully instructed. The patients were in a seated position at a stable, comfortable temperature. Tidal breathing was carried out for a sufficient time to ensure that the subject was comfortable and was wearing the mouthpiece and nose clip appropriately, with no leaks.
DLco maneuvers started with unforced exhalation to RV. The exhalation time was prolonged for up to 12 seconds in order to allow most patients with airflow obstruction to exhale sufficiently to achieve a maximal vital capacity for the subsequent inhalation of test gas.4 The breath-hold time was 10–15 seconds, a target easily achieved in the vast majority of patients.10 All measurements were taken between 10 and 12 am in order to avoid diurnal variations. As cigarette smoking is the most common source of carboxyhemoglobin,11 active smokers were invited to quit smoking at least 24 hours before the test. No patient used supplemental oxygen for at least 2 hours prior to the test.
The number of attempts required to achieve accurate and reliable measurements with each method, and the corresponding time (in minutes) spent, were calculated for all patients. Moreover, in agreement with the ERS/ATS recommendations, when repeated measurements were needed, a time interval of 10 minutes between measurements was applied to allow for the adequate elimination of the test gas from the lungs.4
Because making many attempts is absolutely not recommended,12,13 when LVs and/or DLco measurements proved impossible after three repeated sequential attempts (due to the patient’s lack of cooperation), the measurement was stopped and this was recorded as a failure.
Finally, the cost of measurements obtained with each method was calculated by measuring: 1) the time spent by the expert nurse in explaining, demonstrating, and performing the tests, and 2) the time spent by patients (loss of productivity) to perform the test. The nurse’s cost/minute was calculated based on the mean annual salary of a professional hospital nurse14 divided by 1512 hours/year (ie 36 hours/week for 42 working weeks/year). The cost was adjusted to the 2020 value using figures from the Italian consumer price index.15 The economic value of each patient’s day loss for performing the test was valued using the cost of paid and unpaid (household activities, caring for family members and others, and volunteering) work, specific for age and sex,16 updated to 2020.15 For retired patients, only unpaid work was considered. If the subject was accompanied by a caregiver, their paid and unpaid work was also considered.
Statistics
Based on clinicians’ experience, for every five patients performing the LV test by WBP, one patient was expected to fail the test, ie he or she would be unable to achieve the correct measurements. Furthermore, a 40% reduction in failure risk could be considered clinically significant. Using the formula for matched-pairs samples,17 with type I error of 5% and 80% statistical power, at least 107 patients should be enrolled in the study.
Continuous data were presented as means and standard deviation (SD), and categorical data as absolute and relative frequencies. Differences in baseline characteristics among the groups recruited were tested by ANOVA for continuous data and by Fisher’s exact test for categorical variables.
Values for FEV1, TLC, RV, and DLco obtained with each technique, together with the corresponding number of attempts required to achieve the first reliable measurements and the total time spent, were compared by a generalized linear regression model (family gamma). Failure risks occurring with WBP and the MiniBox+ were compared by Poisson regression. All analyses were adjusted considering patients’ baseline characteristics and type of diagnosis as covariates. Failure risks, number of attempts, and time spent performing the tests were also adjusted for the schooling level of each patient. Comparisons were presented as mean difference (Δ) for continuous outcomes or risk ratio (RR) for failure risk, together with the corresponding 95% confidence interval (95% CI).
Ethics
The study was approved by the Ethical and Scientific Commission of the National Centre for Respiratory Pharmacoeconomics and Pharmacoepidemiology of Verona (Italy) during the session of October 6th, 2017 (# 003/MP/2017). This study was conducted in accordance with the Declaration of Helsinki.
Results
A total of 134 patients were enrolled in the study: 42 asthmatics (32.1%), 47 patients with COPD (35.1%), and 44 with restrictive respiratory disorders (32.8%). The cohort consisted of 67 women (50%), the mean age was 67.4 years (SD=13.5), and mean BMI was 25.9 kg/m2 (SD=4.6). At the time of the study, 21 patients (15.7%) were active smokers, 56 (41.8%) were former smokers, defined as having quit for ≥12 months, and 57 (42.5%) were never smokers. Baseline characteristics of the whole sample and by lung disease are reported in Table 1. Age distribution and smoking status were different among patients with asthma, COPD, and restrictive respiratory disorders (ANOVA test p<0.0001 and p=0.005, respectively). Patients with COPD and restrictive disorders were older than asthmatic patients (by about 10 years), while the prevalence of active smokers among COPD patients was more than twice that observed in the asthmatic group (29.8% vs 14.0%, respectively), but almost negligible among patients with restrictive respiratory disorders (2.3%).
 |
Table 1 Baseline Characteristics of the Whole Sample and by Lung Disorder |
A total of 26 patients (19.4%) experienced at least one failure with WBP, and 11 patients (8.21%) with the MiniBox+ (adjusted RR=0.417, 95% CI 0.242 to 0.720) (Figure 1). In particular, when tested by means of WBP, 18/26 patients (69.2%) failed to achieve the DLco measurement, while five (19.2%) failed in the measurement of LVs (ie TLC, FEV1, or RV), and three (11.5%) failed both measurements. When tested by means of the MiniBox+, 11 patients (8.2%) failed the sole DLco measurement and none (0.0%) the LV measurements (Figure 2). Moreover, the overall DLco failure risk was 15.67% when using WBP, and 8.21% with the MiniBox+ (adjusted RR=0.519, 95% CI 0.287 to 0.938) (Figure 1).
 |
Figure 2 MiniBox+™ and WBP: analytic comparison of their failure risks. Abbreviations: DLco, diffusing capacity of the lung for carbon monoxide; LVs, lung volumes; WBP, whole body plethysmograph. |
The mean number of attempts and the total time spent in taking the first reliable measurements were significantly lower with the MiniBox+, both in the case of success and in the case of failure (Table 2). After adjusting for the failure risk, the MiniBox+ was associated with a lower number of attempts (−1.20, 95% CI −1.38 to −1.01) (Table 2) and a shorter total time spent (−6.07, 95% CI −6.85 to −5.30) (Table 2).
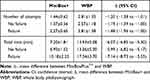 |
Table 2 MiniBox+™ and WBP: Comparison of Their Usability |
Mean values of all lung function parameters collected are reported in Table 3. TLC and DLco values obtained by the two measurement techniques were almost equal. When compared to those obtained by WBP, FEV1 values measured by the MiniBox+ were slightly higher, whereas RV values were slightly lower, although both differences were clinically negligible. The relative error was quite low for both parameters: 2.5% (95% CI 1.1 to 4%) and −5.0% (95% CI −7.9 to −2.1%), respectively.
 |
Table 3 Comparison Among Parameters Measured by the MiniBox+™ and by WBP |
The total cost per test was estimated at €87.58 (95% CI 75.44 to 99.71) with WBP and €75.11 (95% CI 65.70 to 84.52) with the MiniBox+ (Figure 3). The MiniBox+ was associated with a cost reduction of €12.33 (95% CI −18.73 to −5.93), mainly due to the saving in productivity loss (€10.04, 95% CI −16.32 to −3.76).
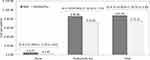 |
Figure 3 MiniBox+™ vs WBP: comparison of their economic impact. Abbreviations: CI, confidence interval; Δ, mean difference.; WBP, whole body plethysmograph. |
Discussion
Despite WBP being generally regarded as the top technique for investigating lung function,2 some major unavoidable procedures can affect its current use: 1) the patient has to enter and breathe inside a sealed box for a while; 2) the patient has to perform some complex respiratory maneuvers of variable duration against a closed shutter;1,18–20 and 3) disabled or obese patients, patient with severe respiratory disease, as well as those with claustrophobia, may not agree or may refuse to enter the box, thus making any measurement impossible.
According to the primary outcome of our study, the influence of the patients’ compliance and the adherence to WBP procedures was clear, as 19.4% of patients (nearly one in five patients, as expected from clinicians’ experience) failed to achieve the measurements. In contrast, the MiniBox+, which uses a technique that avoids the majority of WBP’s limiting factors, was affected by a much lower failure risk (8.2%), with an absolute risk reduction of more than 10%.
In particular, even though the failure risk in performing LV measurements using WBP was significantly higher (5.97% vs 0.0% with the MiniBox+), the most dramatic failure was seen in the DLco measurements using WBP compared to those observed using the MiniBox+ (15.67% vs 8.21%, respectively). These analytic comparisons further emphasize the critical role of the complexity of required procedures in determining such different feasibilities with the two methods. In addition, both the number of attempts and the overall time spent for measurements were always significantly lower with the MiniBox+, both in patients who performed the measurements properly and in those who failed to achieve the measurements, regardless of their age, sex, schooling level, and basic lung disorder. This evidence further supports the higher feasibility of the MiniBox+ method in clinical practice.
The assessment of LVs and DLco represents the essential approach for diagnosing, managing, and monitoring acute and chronic respiratory disorders effectively, both in clinics and in research protocols. Both the suitability and the reliability of methods adopted for measurements are essential features, together with the consistency of the measurements obtained.21 In addition to the technological accuracy of measurements, the easy demonstration by technicians of the actions needed to obtain reliable measurements, patients’ quick comprehension of the maneuvers to perform, the acceptability to the patients, the easy management of the equipment, and the containment of all related costs are other aspects of great relevance from this point of view. They can contribute toward extending the use of complete and appropriate lung function measurements, which otherwise may too frequently be limited to quick flow–volume loops in daily clinical practice.
In terms of absolute values, the data in the present study strongly confirm the high consistency between the measurements of LVs achieved by WBP and the MiniBox+, without any clinically significant overestimation or underestimation. Moreover, DLco measurements obtained with the two techniques proved equivalent independently of the patients’ basic lung disorder, such as bronchial asthma, COPD, or restrictive respiratory disease. Such a comparison has not been investigated before, to the best of our knowledge.
Finally, the last objective of the present paper was to compare the economic impact of the two techniques, this being another aspect that has never been previously investigated. The total cost per test was significantly lower, by 15.8%, with the MiniBox+ and it was shown to be associated with an absolute cost reduction of €12.33 (95% CI −18.73 to −5.93) per patientper test, mainly due to the saving in productivity loss.
Further components of cost (defined in the present study as “critical components of cost”) would also be considered; namely, the basic cost of the equipment, the cost of the calibration gases, and the frequency of service interventions required every year. All of these components, despite being clearly in favor of the MiniBox+, are impossible to calculate exactly as they depend on some uncontrolled variables, such as the extent of the rebate originally obtained from the producers (obviously unknown), the number of tests performed in each center, and the effective frequency and accuracy of equipment maintenance. However, despite not being considered specifically, some critical components of cost were clearly different. The basic current factory cost of the equipment is about €34,000 for WBP and €18,600 for the MiniBox+. The current cost of the calibration gases is €800 for WBP (one cylinder containing O2/CO2 in nitrogen plus one cylinder containing CO/CH4 in air, enough for around 60 tests) and €450 for the MiniBox+ (only one cylinder containing CO/CH4 in air, enough for 80 tests). Moreover, the cost per year for the service interventions is higher for WBP (about €1200 vs €150 for the MiniBox+). A further, although largely unpredictable, component of cost depends of the immovability versus the transportability of the two pieces of equipment: while WBP is absolutely stationary, the MiniBox+ can be easily moved up to the patient’s bed, thus expanding its use and contributing toward further amortizing its overall utilization cost.
The present study represents the first investigation aimed at comparing the economic impact of measurements of LVs and DLco carried out by means of WBP and the MiniBox+. As no other experience is currently available in the literature to use as a reference for discussion, the present results need to be evaluated further in similar studies.
The present study has some limitations. It was a monocentric study, although the results on the reliability of measurements confirmed those of a multinational study on the same topic, published in 2021.9 The economic calculations were not quantitatively exhaustive owing to the incomplete knowledge on some critical components of cost, as a result of their original lack of availability and unpredictability. For these reasons, larger samples of patients would be worth investigating from this point of view. However, points of strength in this study include the procedures strictly following the International Guidelines for obtaining the LV and DLco measurements by both techniques, the randomization of the sequence of measurements, and the statistical methods adopted.
Conclusions
WBP and the MiniBox+ are two effective methods for measuring LVs and DLco, despite requiring a variable complexity of maneuvers to perform the measurements. The feasibility was dramatically different between the two methods, in favor of the MiniBox+, and clearly supported by its significantly lower failure risk. LVs and DLco measured with the two methods proved to be equivalent, regardless of the patients’ basic characteristics. The convenience of the two methods was also different and in favor of the MiniBox+, in view of the number of attempts, the overall time spent in obtaining the first reliable measurement, and the cost of productivity being much lower.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Du Bois AB, Bothelo SY, Bedell GN, Marshall R, Comroe JH
2. Coates AL, Peslin R, Rodenstein D, Stocks J. Measurement of lung volumes by plethysmography. Eur Respir J. 1997;10:1415–1427. doi:10.1183/09031936.97.10061415
3. Stanojevic S, Graham BL, Cooper BG. Official ERS technical standards: global lung function initiative reference values for the carbon monoxide transfer factor for Caucasians. Eur Respir J. 2017;50(3):1700010. doi:10.1183/13993003.00010-2017.
4. Graham BL, Brusasco V, Burgos F, et al. 2017 ERS/ATS standards for single-breath carbon monoxide uptake in the lung. Eur Respir J. 2017;49:1600016. doi:10.1183/13993003.00016-2016
5. Garfield JL, Marchetti N, Gaughan JP, Steiner RM, Criner GJ. Total lung capacity by plethysmography and high-resolution computed tomography in COPD. Int J Chron Obstruct Pulmon Dis. 2012;7:119–126. doi:10.2147/COPD.S26419
6. Fredberg JJ, Cohen I, Adam O, et al. Determination of total lung capacity (TLC) without body plethysmography. Am J Respir Crit Care Med. 2014;189:A2933.
7. Tantucci C, Bottone D, Borghesi A, Guerini M, Quadri F, Pini L. Methods for measuring lung volumes: is there a better one? Respiration. 2016;91(4):273–280. doi:10.1159/000444418
8. Rodenstein DO, Stanescu DC, Francis C. Demonstration of failure of body plethysmography in airway obstruction. J Appl Physiol. 1982;52:949–954. doi:10.1152/jappl.1982.52.4.949
9. Berger KI, Adam O, Dal Negro RW, et al. Validation of a novel compact system for the measurement of lung volumes. Chest. 2021;159(6):2356–2365. doi:10.1016/j.chest.2021.01.052
10. Welle I, Eide G, Bakke P, et al. Applicability of the single-breath carbon monoxide diffusing capacity in a Norwegian community study. Am J Respir Crit Care Med. 1998;158:1745–1750. doi:10.1164/ajrccm.158.6.9712123
11. Schimmel J, George N, Schwarz J, et al. Carboxyhemoglobin levels induced by cigarette smoking outdoors in smokers. J Med Toxicol. 2018;14(1):68–73. doi:10.1007/s13181-017-0645-1
12. Zavorsky G. The rise in carboxyhemoglobin from repeated pulmonary diffusing capacity tests. Respir Physiol Neurobiol. 2013;186:103–108. doi:10.1016/j.resp.2013.01.001
13. Frey T, Crapo R, Jensen R, et al. Diurnal variation of the diffusing capacity of the lung: is it real? Am Rev Respir Dis. 1987;136:1381–1384. doi:10.1164/ajrccm/136.6.1381
14. Occupation in Publich Health [L’occupazione nella sanità pubblica]. Available from: https://www.istat.it/it/files//2020/05/Statistica_today_sanit%C3%A0_2018.pdf.
15. Harmonized Indices of Consumer Prices (HICP), European Commission EuroStat. [Internet]; 2020. Available from: https://ec.europa.eu/eurostat/web/hicp/data/main-tables.
16. Pradelli L, Ghetti G. A general model for the estimation of societal costs of lost production and informal care in Italy. Farmeconomia Heal Econ Ther Pathways. 2017;18.
17. Woolson RF, Clarke WR. Statistical Methods for the Analysis of Biomedical Data.
18. Stanescu DC, Clement J, Pattijn J, Woestijne KP. Glottis opening and airway resistance. J Lab Physiol. 1972;32:460–466.
19. Christie RV. The elastic properties of the emphysematous lung and their clinical significance. J Clin Invest. 1934;13:295–302. doi:10.1172/JCI100588
20. Dayman H. Mechanics of airflow in health and emphysema. J Clin Invest. 1951;30:1175–1185. doi:10.1172/JCI102537
21. Tantucci C. Comparison among different methods on measurement of total lung capacity in COPD. Chest. 2010;1:620–628.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

