Back to Journals » Clinical Ophthalmology » Volume 16
Comparison of Clinical Outcomes Following Gel Stent Implantation via Ab-Externo and Ab-Interno Approaches in Patients with Refractory Glaucoma
Authors Gallardo MJ , Vincent LR, Porter M
Received 21 December 2021
Accepted for publication 27 June 2022
Published 6 July 2022 Volume 2022:16 Pages 2187—2197
DOI https://doi.org/10.2147/OPTH.S354038
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Mark J Gallardo,1– 3 Logan R Vincent,1 Matthew Porter2
1El Paso Eye Surgeons, El Paso, TX, USA; 2Department of Ophthalmology, Texas Tech University School of Medicine, Lubbock, TX, USA; 3Department of Ophthalmology, University of Texas Health Sciences Center at San Antonio, San Antonio, TX, USA
Correspondence: Mark J Gallardo, El Paso Eye Surgeons, 1201 N Mesa St, Ste G, El Paso, TX, 79902, USA, Tel +1 915 542 0279, Email [email protected]
Purpose: To compare clinical outcomes following gel stent implantation via ab externo and ab interno approaches in patients with refractory glaucoma.
Patients and Methods: This retrospective study included 203 eyes of 185 patients aged ≥ 45 years who underwent Xen gel stent implantation as a standalone procedure for medically uncontrolled glaucoma (intraocular pressure (IOP) ≥ 18 mmHg) despite maximum tolerable IOP-lowering medications. One hundred and five eyes underwent gel stent implantation via ab interno approach and 98 via ab externo. Patients with prior conjunctival-incisional glaucoma or cataract surgery were also included. Study parameters were reduction in IOP and number of IOP-lowering medications from baseline to 3, 6, 9 and 12 months postoperatively.
Results: There were no statistically significant differences in the age, sex, preoperative IOP, number of IOP-lowering medications or cup–disc ratio between the ab interno and ab externo groups at baseline (p > 0.05). At all postoperative time points, mean IOP and percentage reduction from baseline were comparable in both groups (p > 0.05) except at postoperative 6 months when the outcomes were significantly better (p < 0.05) in the ab externo group. The rate of postoperative procedures (5-Fluorouracil injections and bleb needling), the incidence of numerical or clinical hypotony and adverse events were comparable in both groups (p > 0.05). The mean number of IOP-lowering medications was comparable in both groups at all time points.
Conclusion: The Xen gel stent, whether implanted ab interno or ab externo, is effective in reducing IOP and dependence on topical medications in eyes with refractory glaucoma. The stent may be used in both phakic and pseudophakic patients and is a reasonable option for patients with prior failed trabeculectomy.
Keywords: subconjunctival gel stent, gel stent, Xen gel stent, ab interno gel stent implantation, ab externo gel stent implantation, refractory glaucoma
Introduction
Innovative minimally invasive glaucoma surgery (MIGS) techniques and devices have been developed in recent years for the surgical management of glaucoma.1 MIGS procedures have been documented to have better safety and more rapid postoperative recovery than traditional glaucoma surgeries.2,3 Several MIGS devices work by improving outflow through the physiological pathway of Schlemm’s canal or the suprachoroidal space.4,5 The Xen Gel Stent (Xen 45, Allergan Inc., Irvine, CA), intended for management of refractory glaucoma, bypasses conventional outflow pathways by creating a filtration route from the anterior chamber to the subconjunctival space, in a manner similar to trabeculectomy.6,7
In the majority of the gel stent studies published to date, an ab-interno implantation technique has been used, an approach used during clinical trials. With this approach, significant reduction in intraocular pressure (IOP) and the number of IOP-lowering medications have been reported.8–10 As glaucoma surgeons have gained experience with this device, some have reported using an alternative, off-label, ab externo, approach to implantation. The potential advantages of an ab-externo approach include reduced surgical manipulation within the anterior chamber, elimination of corneal incisions, optional use of viscoelastic, and decreased likelihood of the distal end of the gel stent becoming embedded in Tenon’s capsule.7 Additionally, an ab externo approach makes possible the implantation of a gel stent in eyes in which it cannot be implanted with an ab interno approach due to corneal opacity or scarring in the superonasal quadrant.
However, there are limited data available on the safety and efficacy of the ab externo approach to gel stent implantation. The purpose of the present study is to compare clinical outcomes following gel stent implantation via an ab externo approach to the conventional ab interno approach in patients with refractory glaucoma on maximum tolerable medical therapy, including eyes with or without prior cataract surgery and with or without prior conjunctival-incisional glaucoma surgery.
Patients and Methods
This single center, retrospective study included chart records of consecutive patients with refractory glaucoma who underwent ab interno Xen 45 gel stent implantation between April 2017 and January 2019 or ab externo Xen 45 gel stent implantation between January 2019 and August 2019 et al Paso Eye Surgeons, PA, a tertiary care practice in El Paso, Texas, USA. As such, the two groups – ab interno and ab externo – were temporally separated. The authors’ intent was to compare the first 100 cases with the new approach (ab externo) to the first 100 cases performed with the standard approach (ab interno). Twelve months of follow-up were evaluated for all eyes. The study was performed in accordance with the tenets of the Declaration of Helsinki and its amendments and was approved by the Medical Executive Committee at the Surgical Centers of El Paso with waiver of informed consent as the data were recorded in patient charts as a part of routine clinical practice, and only de-identified patient data were analyzed.
Inclusion and Exclusion Criteria
Patients aged 45 years or above who were diagnosed with medically uncontrolled glaucoma (IOP ≥ 18 mmHg) or their IOP were above target for the stage of glaucoma despite maximum tolerable IOP-lowering medications and underwent gel stent implantation as a standalone procedure were included in the study. Patients with a history of prior glaucoma conjunctival-based procedures, including trabeculectomy, ExPress shunt, glaucoma drainage devices, and canaloplasty, were also included if the conjunctiva in the targeted implantation region was mobile, healthy, and devoid of fibrosis or excessive vascularization. Patients with a history of angle-based or MIGS surgery or prior cataract surgery were included.
Exclusion criteria included case records with active inflammatory or neovascular disorders, such as proliferative diabetic retinopathy or uveitis, active diabetic retinopathy requiring medical or surgical intervention (clinically significant macular edema), wet age-related macular degeneration, branch retinal or central retinal vein occlusion, clinically significant ocular inflammation within 30 days of surgery (eg, severe ocular surface disease, herpes simplex infection), active use of oral carbonic anhydrase inhibitors, and the presence of silicone oil or vitreous in anterior chamber. Patients who underwent a combined cataract and gel stent implantation procedure were also excluded.
Surgical Technique
All procedures were performed by a single surgeon (MJG).
Ab Interno Implantation
Under topical anesthesia, an anti-fibrotic agent (mitomycin C [MMC] 40 µg (0.2 mL of 0.2 mg/mL concentration)) was injected into the subconjunctival space prior to the creation of corneal incisions. Two paracenteses were created`ne inferotemporal, to facilitate introduction of the injector needle, and the other superotemporal, to allow for counter-traction. Preservative-free lidocaine 2% was infused and the anterior chamber was filled with a cohesive viscoelastic agent (Healon GV, Johnson & Johnson Surgical Vision Inc., Santa Ana, CA). The needle of the injector was then introduced through the inferotemporal paracentesis, into and across the anterior chamber towards the superonasal or 12 o’clock angle position. The needle tip was placed at the non-pigmented trabecular meshwork using indirect visualization with a gonioprism. Once confirmed, the needle was pushed through the sclera and exited 3 mm posterior to the limbus. The needle was further advanced until the stop collar reached the angle. The tip of the needle was rotated towards the 12 o’clock position and the stent was delivered into the subconjunctival space. Intraoperative gonioscopy was performed to ensure that 1 mm of the stent was in the anterior chamber. The external (subconjunctival) portion of the stent was visualized to ensure the stent was mobile. The viscoelastic was evacuated and bleb formation was confirmed using a balanced salt solution. If all three markers were not confirmed (1 mm in the anterior chamber, stent mobility in the subconjunctival portion and bleb formation), the stent was removed via an ab interno approach with micro-surgical forceps, the delivery device was reloaded, and the stent was re-implanted.
Ab Externo Implantation
Under topical anesthesia, the eye was infraducted using 7–0 vicryl suture to provide optimal visualization of the superior bulbar conjunctiva. The conjunctiva was grasped with forceps 8–10 mm posterior to the limbus, and the injector needle was introduced into the subconjunctival space and directed anteriorly towards the limbus. The needle was inserted into the sclera approximately 2–3 mm posterior to the limbus to create a tunnel and pushed forward into the anterior chamber angle. When anatomy was allowed, the position of the needle was confirmed using an indirect gonioprism to ensure the entry site was away from the iris and cornea. The stent was injected into the anterior chamber while pulling back on the injector to ensure 1 mm of the stent was in the anterior chamber and 2–3 mm was in the subconjunctival space. The stent was repositioned by either pushing or pulling on the device with non-toothed forceps to ensure proper stent position. Once implanted, the internal portion of the stent was evaluated using the gonioprism. Bleb formation was also confirmed once the stent was in proper position. MMC was injected into the region of bleb formation. To ensure no MMC entered the anterior chamber, the external ostea of the stent was tamponaded by external pressure with a cotton-tipped applicator.
The postoperative treatment regimen was the same in both groups. This included a topical antibiotic, 4 times-a-day (QID) for 1 week, and a topical steroid, QID for 4 weeks and titrated thereafter based on clinical assessment of the bleb/conjunctiva. Antifibrotic injections of antimetabolites, 5- Fluorouracil (5-FU 5 mg), with or without concomitant bleb manipulation (needling), were performed at the investigator’s discretion at any time point during the postoperative course when the development of subconjunctival fibrosis (based on bleb appearance, excessive conjunctival hyperemia, IOP elevation) or bleb failure were suspected.
Study Outcomes
Patients were assessed preoperatively and at postoperative Day 1, Week 1, and Months 1, 3, 6, 9 and 12. Effectiveness endpoints included a mean reduction in IOP and a mean reduction in the number of IOP-lowering medications from baseline to 3, 6, 9 and 12 months postoperatively. Secondary endpoints included the percentage of subjects achieving ≥20% reduction in IOP on the same or fewer IOP-lowering medications from baseline to 3, 6, 9 and 12 months postoperatively. Safety endpoints included assessment of all adverse events related to the device, such as implant extrusion, migration, obstruction, etc., the rate of postoperative procedures (bleb needling, 5-FU injections) and the rate of complications, including numeric hypotony ≤6mmHg at any one of the postoperative time points without clinical manifestations of low IOP, clinical hypotony ≤6 mmHg at any one of the postoperative time points with clinical manifestations of low IOP, such as vision reduction (2 lines or more) related to change in anterior chamber depth or macular changes consistent with hypotonous maculopathy (macular folds), optic disc edema, and/or serous or hemorrhagic choroidal effusions, IOP >10 mm above baseline, endophthalmitis, and other complications at all follow-up visits through 12 months. In addition, the study followed the recommendations of World Glaucoma Association (WGA) guidelines to evaluate surgical success, qualified success, and failure rates with three alternative upper limits (ie, ≤ 18, 15 and 12 mmHg) and one lower limit (ie, ≤6 mmHg) of IOP and in terms of the percentage reduction in IOP achieved by surgery. Complete success was defined as ≥20% reduction in IOP from baseline and postoperative IOP ≤18/15/12 mmHg without medications. Qualified success was defined as ≥20% reduction in IOP from baseline and postoperative IOP ≤18/15/12 mmHg with same or fewer medications than baseline. Failure rate was defined as postoperative IOP >18 mmHg or ≤6 mmHg at any two consecutive visits, those requiring more medications compared to baseline or secondary surgical intervention for IOP control.
Eyes in both groups (ab interno and ab externo) were also divided into subgroups based on their history of prior conjunctival incisional surgery and lens status (phakic vs pseudophakic).
Statistical Analysis
Data analysis was performed using Microsoft Excel and SPSS software (version 27.0) for Windows (IBM SPSS Statistics 27, IBM Inc., Armonk, NY). Categorical data were analyzed using Chi-Square test; however, Fisher’s exact test was used in cases where more than 20% of the cells had expected cell values of less than 5 or if the expected value in any cell of the contingency table was less than 1. In the case of continuous variables, normality of the data was checked using the Kolmogorov–Smirnov test and quantile–quantile plots. For normally distributed scale data, independent-sample t-test was used to compare the means between the two groups. For data that were not normally distributed, the non-parametric counterpart Mann–Whitney U-test was used. All P-values were two-sided and were considered statistically significant when less than 0.05.
Results
This retrospective study included 203 eyes of 185 patients (107 females and 78 males; mean age 74.0 ± 11.6 years) of which 105 eyes (94 patients; 49 females and 45 males; mean age 75.0 ± 9.6 years) underwent ab interno and 98 eyes (91 patients; 58 females, 33 males; mean age 72.9 ± 13.4 years) underwent ab externo conjunctival gel stent implantation. Demographic and baseline characteristics of the patients in the two groups are listed in Table 1. There were no statistically significant differences in the age, sex, preoperative IOP, number of IOP-lowering medications or cup–disc ratio between the ab interno and ab externo groups at baseline (p > 0.05). Both groups had patients with similar severity of glaucoma based on the Hodapp-Parrish-Anderson method of classification (p = 0.252). While the ab interno comprised 22% cases with moderate and 74% cases of advanced glaucoma, ab externo comprised 14% with moderate and 79% cases of advanced glaucoma.
 |
Table 1 Demographic and Baseline Characteristics of the Patients in Ab Interno and Ab Externo Groups |
The mean IOP and percentage change in IOP in the ab interno and ab externo groups at all postoperative time points is shown in Figure 1. At all postoperative time points, mean IOP and percentage reduction from baseline were comparable in both groups (p > 0.05) except at postoperative 6 months, when the mean IOP was significantly lower and the percentage reduction in IOP was higher in the ab externo group.
The mean number of IOP-lowering medications (Figure 2) and the corresponding reduction in the number of medications were comparable in both groups at all time points.
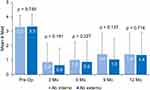 |
Figure 2 Mean number of medications at each visit in eyes implanted with a Xen gel stent via an ab interno or ab externo approach. Error bars indicate standard deviation. |
Figure 3A and B represent the frequency distribution of IOP in the ab interno and ab externo groups, respectively. Preoperatively, 98.1% eyes in the ab interno group and 98% in the ab externo group had IOP >18 mm Hg. Postoperatively, IOP of <18 mmHg was achieved in 87.3% and 95.6% eyes in the ab interno and ab externo group, respectively, at 6 months and in 98.8% and 98.6%, respectively, at 12 months. This improvement in IOP was achieved while reducing the mean number of medications from 3.3 at baseline to 1.4 at 12 months in both groups (Figure 2).
 |
Figure 3 Non-cumulative frequency distribution (percentage) of various IOP ranges in Xen gel stent eyes. (A) Ab interno group. (B) Ab externo group. |
The percentage of eyes achieving ≥20% reduction in IOP was comparable between the two groups at all postoperative time points (p > 0.05) (Table 2). Table 3 shows the success and failure rate (per WGA recommendations) in the ab interno and ab externo groups at different postoperative time points.
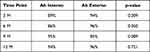 |
Table 2 Comparison of Eyes Achieving ≥20% Reduction in Intraocular Pressure Between Ab Interno and Ab Externo Group |
 |
Table 3 Complete Success, Qualified Success, and Failure Rates in the Ab Interno and Ab Externo Groups at Different Postoperative Time Points |
Subgroup analyses were also performed to compare results in eyes with and without prior conjunctival incisional or cataract surgeries. Figures 4A and B show the mean IOP and the percentage reduction in IOP in eyes with and without prior conjunctival incisional surgery for both the ab interno and ab externo approaches. In the ab interno group, no statistically significant difference between the two subgroups was observed in the mean IOP or reduction in IOP, except at postoperative 6 months when eyes with prior conjunctival incisional surgery had a lower mean IOP and a higher percentage reduction in IOP compared to eyes without prior conjunctival incisional surgery (p = 0.033). In the ab externo group, no statistically significant difference between the two subgroups was observed in the mean IOP or reduction in IOP at any time point. The mean number of medications and the reduction in the number of medications from baseline were comparable in eyes with and without prior conjunctival incisional surgery.
Figures 5A and B show the mean IOP and percentage reduction in IOP in eyes with and without prior cataract surgery, respectively. No statistically significant differences between the eyes with and without prior cataract surgery were observed in the ab interno or ab externo groups. Similarly, the mean number of medications and the reduction in the number of medications from baseline were also comparable in eyes with and without prior cataract surgery.
Table 4 lists the postoperative procedures (use of 5-FU injections and bleb needling) and the adverse events (rates of IOP >10 mmHg from baseline; choroidal effusion; incidence of migrated, exposed or broken implant; and endophthalmitis) observed in each group at any postoperative visit. The rate of postoperative procedures (5-Fluorouracil injections and bleb needling), the incidence of numerical or clinical hypotony and adverse events were comparable in both groups (p > 0.05). Assessment of visual acuity revealed that 85% of eyes in the ab interno group and 87% of eyes in the ab externo group had CDVA better than or equal to baseline CDVA at all postoperative time points.
 |
Table 4 Postoperative Procedures and Adverse Events (at Any Postoperative Visit) Observed in Ab Interno and Ab Externo Groups |
Discussion
Although conventional trabeculectomy and tube shunts are well-established procedures for managing glaucoma, they are associated with the risk of potentially sight-threatening complications such as wound leaks, hypotony, shallow anterior chambers, choroidal effusions, encapsulation and endothelial cell loss.4,11,12 Xen Gel Stent is a procedure that creates a new pathway for the outflow of aqueous humor, similar to conventional trabeculectomy and tube shunt surgeries.13 One of the main advantages of subconjunctival filtration is that it does not impact any of the physiological outflow pathways, and as such, preserves the existing physiological filtration.14 The gel stent was designed to allow controlled passage of aqueous humor, effectively decrease IOP and potentially prevent hypotony in eyes with refractory glaucoma.15–17 The device creates a permanent channel through the sclera, allowing the flow of aqueous humor from the anterior chamber into the subconjunctival space.18 The studies that led to approval of this device relied on an ab interno approach through a small corneal incision19 and, while there are some reports of surgeons using ab externo techniques,20–23 larger studies are needed.
In the present study, we compared the clinical outcomes after ab interno and ab externo gel stent implantation. In terms of efficacy, both approaches yielded similar reduction in IOP through 12 months of follow-up. The percentage of eyes achieving ≥20% reduction in IOP and the mean number of medications were similar at 12 months. In terms of safety, the proportion of eyes that required needling or 5-FU injections was similar for both approaches. While the incidence of hypotony was statistically higher with the ab interno approach, the risk of the implant migrating or becoming exposed appeared higher in the ab externo group, although this difference was not statistically significant. Overall, the incidence of complications in both groups was comparable but trended towards superiority in the ab externo group.
These findings are comparable to the conclusions of Tan et al,24 who reported that an ab externo approach is similar in safety and efficacy to an ab interno approach in a data set of ~80 eyes. We found a greater reduction in IOP with both approaches than reported by Tan et al24 (40.8% vs 28.6% in the ab interno and 45% vs 40.1% in the ab externo approach), as well as a greater reduction in the number of medications (57.6% vs 45.3% in the ab interno and 60.6% vs 50.8% in the ab externo approach). We also evaluated the impact of prior conjunctival incisional surgery or cataract surgery.
Glaucoma surgery in eyes with prior conjunctiva-based filtration surgery is typically considered to be more challenging and an unsuccessful prior filtering surgery is considered a poor prognostic factor for a repeat trabeculectomy, leading many surgeons to avoid implanting gel stents in such eyes.25,26 However, we found that outcomes of gel stent implantation, with either the ab interno or ab externo approach, were not affected by prior conjunctival incisional surgery. Lens status also had little impact on outcomes, suggesting that gel stents may be safely and effectively implanted in phakic or pseudophakic patients with refractory glaucoma.
While both techniques have yielded similar safety and efficacy outcomes, the ab externo approach seems to provide unique benefits. With the ab interno approach, the stent is typically implanted in the superonasal quadrant, for which the surgeon has to take an inferotemporal approach. The injector needle is advanced through the anterior chamber to reach the target location at an angle that penetrates the sclera to position the stent in the subconjunctival space.7,27 If the eye has any corneal opacity, the visibility, perception of depth and the position of the needle can be misleading, with or without gonioscopy. On the other hand, the ab externo approach provides easy accessibility to the entire superior quadrant. In eyes with any previous conjunctival-based surgery, including trabeculectomy, canaloplasty, tube shunt implantation or even scleral tunnel or extracapsular cataract surgery, the gel stent can be precisely positioned in an area with mobile healthy conjunctiva devoid of conjunctival fibrosis using the ab externo approach.17 Furthermore, the ab externo placement avoids viscoelastic injection, intraocular maneuvers are minimal and there is less risk of the distal end of the gel stent becoming embedded in Tenon’s capsule.7 Since the ab externo technique is quite similar to the tube shunt or trabeculectomy, glaucoma surgeons are familiar with this approach. As such, there may be a shorter learning curve than ab interno approach.
The Xen gel stent is indicated for refractory glaucoma, which can have many interpretations, allowing surgeons to offer treatment to a wide range of patients. Trabeculectomy is still the gold standard technique for refractory glaucoma. However, in the author’s experience, gel stent implantation may be the preferred surgical approach for subconjunctival drainage over the more invasive trabeculectomy in certain circumstances. A multicenter comparative study of Xen gel and trabeculectomy may be required to validate the generalizability of the author’s experience.
The proactive use of 5-FU during the postoperative course to modulate healing and reduce the risk of fibrosis seems to be a helpful tool in the authors’ experience. For some patients, needling is an effective means to potentially enhance postoperative outcomes by breaking fibrotic subconjunctival adhesions and/or revitalizing an obstructed Xen tip, which allows for reformation of the bleb.28 There is no consensus on the optimal time to perform a needling procedure after gel stent implantation.28 Vigilance is important to avoid treatment failures due to subconjunctival fibrosis. Per the authors’ experience, curving of the stent indicates the presence of early subconjunctival fibrosis. Needling as soon as any curving of the stent is noted, as was done in this study, may help minimize the risk of treatment failure. This approach to needling is likely responsible for the high needling rate and consequently good outcomes in the present study.
The present study is limited by its retrospective design. Another limitation is the effect of the intraoperative and postoperative management learning curve (earlier cases vs later cases) on the outcomes achieved. Future prospective, controlled, and comparative studies are needed to validate the study outcomes. Additionally, it is important to study outcomes beyond 12 months to assess whether the reduction in IOP and number of medications are maintained over time.
Conclusion
To summarize, the Xen gel stent, whether implanted ab interno or ab externo, is safe and effective in reducing IOP and dependence on topical medications in eyes with refractory glaucoma. Given the comparable outcomes, it is up to the surgeon’s discretion to determine which approach works best in their hands. This type of stent may be used in both phakic and pseudophakic patients and is a reasonable option for patients with a failed prior trabeculectomy who require better IOP control.
Acknowledgment
Raman Bedi, MD (IrisARC – Analytics, Research & Consulting, Chandigarh, India) and Jan Beiting (Wordsmith Consulting, Cary, North Carolina) provided statistical analysis and editorial assistance in the preparation of this manuscript.
Funding
This study was supported by a grant from Allergan Inc., Irvine, CA.
Disclosure
MJG is a clinical investigator, speaker and consultant for Allergan Inc., Irvine, CA. LRV and MP have no relevant conflicts of interest to disclose in this work.
References
1. Buffault J, Graber M, Bensmail D, et al. Efficacy and safety at 6 months of the XEN implant for the management of open angle glaucoma. Sci Rep. 2020;10(1):4527. doi:10.1038/s41598-020-61319-1
2. Fu L, Baker ML, Carley F, Au L. Subconjunctival ab externo gel stent implantation for refractory glaucoma after high-risk penetrating keratoplasty. Cureus. 2020;12(6):e8873. doi:10.7759/cureus.8873
3. Richter GM, Coleman AL. Minimally invasive glaucoma surgery: current status and future prospects. Clin Ophthalmol. 2016;10:189–206. doi:10.2147/OPTH.S80490
4. Bar-David L, Blumenthal EZ. Evolution of glaucoma surgery in the last 25 years. Rambam Maimonides Med J. 2018;9(3):e0024. doi:10.5041/RMMJ.10345
5. Smith M, Charles R, Abdel-Hay A, et al. 1-year outcomes of the Xen45 glaucoma implant. Eye. 2019;33(5):761–766. doi:10.1038/s41433-018-0310-1
6. Reitsamer H, Sng C, Vera V, et al. Two-year results of a multicenter study of the ab interno gelatin implant in medically uncontrolled primary open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol. 2019;257(5):983–996. doi:10.1007/s00417-019-04251-z
7. Vera V, Gagne S, Myers JS, Ahmed IIK. Surgical approaches for implanting Xen Gel stent without conjunctival dissection. Clin Ophthalmol. 2020;14:2361–2371. doi:10.2147/OPTH.S265695
8. Gillmann K, Bravetti GE, Mermoud A, Rao HL, Mansouri K. XEN Gel stent in pseudoexfoliative Glaucoma: 2-year results of a prospective evaluation. J Glaucoma. 2019;28(8):676–684. doi:10.1097/IJG.0000000000001295
9. Lenzhofer M, Kersten-Gomez I, Sheybani A, et al. Four-year results of a minimally invasive transscleral glaucoma gel stent implantation in a prospective multi-centre study. Clin Exp Ophthalmol. 2019;47(5):581–587. doi:10.1111/ceo.13463
10. Mansouri K, Guidotti J, Rao HL, et al. Prospective evaluation of standalone XEN Gel implant and combined phacoemulsification-XEN Gel implant surgery: 1-year results. J Glaucoma. 2018;27(2):140–147. doi:10.1097/IJG.0000000000000858
11. Sheybani A, Lenzhofer M, Hohensinn M, Reitsamer H, Ahmed II. Phacoemulsification combined with a new ab interno gel stent to treat open-angle glaucoma: pilot study. J Cataract Refract Surg. 2015;41(9):1905–1909. doi:10.1016/j.jcrs.2015.01.019
12. Ucar F, Cetinkaya S. Xen implantation in patients with primary open-angle glaucoma: comparison of two different techniques. Int Ophthalmol. 2020;40(10):2487–2494. doi:10.1007/s10792-020-01427-z
13. Pillunat LE, Erb C, Junemann AG, Kimmich F. Micro-invasive glaucoma surgery (MIGS): a review of surgical procedures using stents. Clin Ophthalmol. 2017;11:1583–1600. doi:10.2147/OPTH.S135316
14. Gillmann K, Mansouri K. Minimally invasive glaucoma surgery: where is the evidence? Asia Pac J Ophthalmol. 2020;9(3):203–214. doi:10.1097/APO.0000000000000294
15. Dangda S, Castanos MV, Do A, Panarelli JF. XEN gel stent: a review. Cli Exp Vis Eye Res J. 2019;2(1):30–37. doi:10.15713/ins.clever.25
16. Harris JM, Sola-Del Valle D. Effective treatment of a normal-tension glaucoma patient with bilateral ab externo XEN Gel Stent implantation. Am J Ophthalmol Case Rep. 2020;20:100947. doi:10.1016/j.ajoc.2020.100947
17. Panarelli JF, Yan DB, Francis B, Craven ER, Gel Stent XEN. Open conjunctiva technique: a practical approach paper. Adv Ther. 2020;37(5):2538–2549. doi:10.1007/s12325-020-01278-1
18. Grover DS, Flynn WJ, Bashford KP, et al. Performance and safety of a new ab interno gelatin stent in refractory glaucoma at 12 months. Am J Ophthalmol. 2017;183:25–36. doi:10.1016/j.ajo.2017.07.023
19. Fea AM, Durr GM, Marolo P, Malinverni L, Economou MA, Ahmed I. XEN((R)) Gel stent: a comprehensive review on its use as a treatment option for refractory glaucoma. Clin Ophthalmol. 2020;14:1805–1832. doi:10.2147/OPTH.S178348
20. Yuan L, Lai G, Raiciulescu S, Kim W Outcomes of ab interno placement versus ab externo transconjunctival placement of Xen 45 gel stents.
21. Gagne S. MIGS performed at the slit lamp: ab externo (closed conjunctiva) implantation of a Gel microstent.
22. Myers JS, Zheng CX, Moster SJ, Lin M. Short term outcomes of transconjunctival ab externo XEN 45 Gel Stent implantation. Invest Ophthalmol Vis Sci. 2019;60(9):3735.
23. Purgert R, Lin M, Mehren N Outcomes of ab interno versus ab externo XEN gel stent implantation.
24. Tan NE, Tracer N, Terraciano A, Parikh HA, Panarelli JF, Radcliffe NM. Comparison of safety and efficacy between Ab Interno and Ab Externo approaches to XEN Gel Stent placement. Clin Ophthalmol. 2021;15:299–305. doi:10.2147/OPTH.S292007
25. Piltz-Seymour JR Glaucoma surgery: when the conjunctiva isn’t ideal. review of ophthalmology; 2017. Available from: https://www.reviewofophthalmology.com/article/glaucoma-surgery-when-the-conjunctiva-isnt-ideal.
26. Cankaya AB, Elgin U. Comparison of the outcome of repeat trabeculectomy with adjunctive mitomycin C and initial trabeculectomy. Korean J Ophthalmol. 2011;25(6):401–408. doi:10.3341/kjo.2011.25.6.401
27. Vera V, Ahmed IIK, Stalmans I, Reitsamer H. Gel stent implantation—recommendations for preoperative assessment, surgical technique, and postoperative management. US Ophthalmic Rev. 2018;11(1):38–46. doi:10.17925/USOR.2018.11.1.38
28. Vera V, Sheybani A, Lindfield D, Stalmans I, Ahmed IIK. Recommendations for the management of elevated intraocular pressure due to bleb fibrosis after XEN gel stent implantation. Clin Ophthalmol. 2019;13:685–694. doi:10.2147/OPTH.S195457
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



