Back to Journals » Medical Devices: Evidence and Research » Volume 12
Comparison of blood pressure measurements in the upper and lower extremities versus arterial blood pressure readings in children under general anesthesia
Authors Hayes S, Miller R , Patel A, Tumin D, Walia H, Hakim M , Syed F, Tobias JD
Received 22 March 2019
Accepted for publication 12 August 2019
Published 22 August 2019 Volume 2019:12 Pages 297—303
DOI https://doi.org/10.2147/MDER.S209629
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Seth Hayes,1 Rebecca Miller,1 Ambrish Patel,2,3 Dmitry Tumin,1,2 Hina Walia,1 Mohammed Hakim,1 Faizaan Syed,1 Joseph D Tobias1,2,4
1Department of Anesthesiology and Pain Medicine, Nationwide Children’s Hospital, Columbus, OH 43205, USA; 2Department of Pediatrics, The Ohio State University, Columbus, OH 43210, USA; 3Division of Pediatric Critical Care, Nationwide Children’s Hospital, Columbus, OH 43205, USA; 4Department of Anesthesiology and Pain Medicine, The Ohio State University, Columbus, OH 43210, USA
Correspondence: Seth Hayes
Department of Anesthesiology and Pain Medicine, Nationwide Children’s Hospital, 700 Children’s Drive, Columbus, OH 43205, USA
Tel +1 614 722 4200
Fax +1 614 722 4203
Email [email protected]
Purpose: To compare invasive blood pressure (IBP) readings obtained from an arterial cannula with non-invasive blood pressure (NIBP) measurements from oscillometric cuffs on the upper and lower extremities of infants and children under general anesthesia.
Patients and methods: Patients under 10 years of age were enrolled in our study if they were to receive general anesthesia with planned placement of a radial arterial cannula. At 5 mins intervals, IBP was measured using a fluid-coupled pressure transducer and NIBP was measured with two oscillometers with appropriately sized cuffs placed on the upper arm and lower leg, for 10 readings per patient.
Results: The study enrolled 18 boys and 12 girls, ranging in age from 0 to 8 years. Across 300 data points, the absolute difference between the arm and invasive mean arterial pressure (MAP) measurements was 7±7 mmHg (range: 0–52 mmHg). The absolute difference between the leg and invasive MAP measurements was 8±8 mmHg (range: 0–52 mmHg). Although both non-invasive measurement sites demonstrated frequent deviation from invasive measurement, large deviations were more common when BP was measured at the leg (81 of 298 observations (27%) deviating by >10 mmHg) compared to the arm (60 of 300 observations (20%) deviating by >10 mmHg).
Conclusion: The frequency of clinically significant NIBP deviation in children under general anesthesia supports the importance of IBP monitoring when hemodynamic fluctuations are likely and would be particularly detrimental. NIBP measured at the lower leg is more likely to result in clinically significant deviation from invasively measured MAP than NIBP values obtained from an upper arm.
Keywords: invasive blood pressure, non-invasive blood pressure, blood pressure cuff
Introduction
Blood pressure (BP) monitoring has played an important role in the delivery of a safe general anesthetic since the sphygmomanometer was endorsed by Dr. Harvey Cushing in the early 1900s. It has been a standard required by the American Society of Anesthesiologists (ASA) during any general anesthetic since 1986. With BP measurements guiding major therapeutic decisions in the perioperative area, inaccuracies may complicate the timely diagnosis and treatment of hemodynamic instability. Pediatric anesthesiologists routinely decide to administer fluid, blood products, and inotropic agents based on deviations from what is considered a “normal” BP.1 As intraoperative hyper- and hypotension have been demonstrated to be associated with postoperative morbidities including acute kidney injury, encephalopathy, myocardial infarction, stroke, and increased 30-day mortality, inaccurate BP measurements may result in harmful, unrecognized BP deviations.2–5
Intraoperatively, BP can be obtained non-invasively (NIBP) by an oscillometric BP cuff or invasively (IBP) by an indwelling arterial cannula. Oscillometric cuffs work by inflating to a pressure above a patient’s systolic blood pressure (SBP) to occlude the patient’s artery, then measure pressure fluctuations as the cuff is incrementally deflated. The point with the highest amplitude of pressure fluctuations is the mean arterial pressure (MAP). The SBP and diastolic blood pressure (DBP) are then calculated from the MAP and the pattern of oscillometric changes. Algorithms for these calculations are proprietary and vary depending on the NIBP cuff manufacturer.6 In contrast, invasive arterial cannulas measure SBP and DBP directly from a pressure pulse wave. The MAP is derived from these values.7
Several studies have investigated the correlation of IBPs to NIBPs in children with mixed results. In 2010, Meyer et al conducted a study showing low bias (<1 mmHg) on a Bland-Altman analysis of non-invasively measured mean arterial pressures in preterm infants and suggested that the correlation between IBP and NIBP has improved as NIBP technology has advanced.8 However, O’Shea et al noted a tendency toward falsely elevated NIBP values in this patient population despite development of newer, more sophisticated NIBP devices, even when possible confounding factors such as cuff size and level of activity were eliminated.9 Further studies have evaluated BP measurements in critically ill pediatric patients. Two of these found “much variability” between invasive and non-invasive monitoring techniques and concluded that underappreciated hyper- and hypotension in PICU patients may result in under-treatment.10,11 In contrast, Ray et al studied BP values in two pediatric intensive care units and concluded from a trend of lower mean and diastolic NIBP-values that over-treatment of hypotension may be occurring up to 40% of the time.12
It is known that the use of an appropriately sized cuff is imperative to produce the most accurate noninvasive reading. The American Heart Association (AHA) recommends the cuff bladder width and length be 40% and 80%, respectively, of the mid-arm circumference.13 It is also known that NIBP can be affected by subject movement and activity, as external stimuli can interfere with the accuracy of BP measurement.13,14 Although these potential sources of error in NIBP measurement are generally recognized, the extent of deviation from IBP measurement is still not well characterized in children. If non-invasive monitoring tends to over- or under-estimate BP, it may provide falsely reassuring values in hemodynamically unstable patients. By studying NIBP values in children under general anesthesia subject movement and activity are eliminated, potentially resulting in more accurate measurements. Therefore, we conducted this prospective, observational study to compare IBP obtained from an arterial cannula with NIBP measurements from oscillometric cuffs on the upper and lower extremities of children under general anesthesia. Our primary hypothesis was that NIBP readings over-estimate BP when compared to an invasive device. With little evidence comparing NIBP readings obtained from upper and lower limbs, the decision to use a specific limb is often a practical one determined by ease of access and the need to avoid peripherally placed intravenous catheters. Therefore, our secondary aim was to investigate the correlation and bias between upper arm versus lower leg NIBP measurements.
Materials and methods
The study was approved by the Institutional Review Board (IRB) at Nationwide Children’s Hospital (Columbus, OH, USA) and was conducted in accordance with the Declaration of Helsinki. The study was registered at clinicaltrials.gov (NCT03220906). Thirty patients were enrolled according to the availability of research staff to complete this study. Verbal informed consent was obtained from the parents of the patients prior to study participation (a waiver of written consent was obtained from the IRB). Patients under 10 years of age, with American Society of Anesthesiologists (ASA) classification 1–3, were enrolled in our study if they were to receive general anesthesia with a planned radial arterial cannula. IBPs were measured using a fluid-coupled pressure transducer (Edwards Lifesciences TruWave) with continuous BP display (Philips Intellivue). NIBPs were measured with two separate oscillometers of the same make (Philips Intellivue) with appropriately sized BP cuffs (as defined by the AHA recommendations) placed on the upper arm and lower leg.
Systolic, diastolic, and mean arterial pressures (MAP) from 3 sites (radial artery, arm cuff, and leg cuff) were recorded at 5 mins intervals for 10 readings per patient. For patients placed on cardio-pulmonary bypass (CPB) during surgery, 5 readings were obtained prior to CPB initiation and 5 readings were obtained after bypass conclusion. An a priori power analysis was performed for a one-sample test of proportions. We calculated that the study would require 185 cases to have 80% power for demonstrating an error rate with non-invasive measurement greater than 10%, compared to a maximum acceptable error rate of 5%, at a statistical significance level of 95%. Enrollment was curtailed after 30 patients were enrolled for a total of 300 BP observations.
The primary outcome was clinically significant bias as defined by the deviation of BP of >5 mmHg between IBP and NIBP. We also examined the occurrence of deviations in excess of 10 mmHg. Continuous data were compared between sites using Bland-Altman analysis.15 On multivariable analysis, we modeled the absolute difference between NIBP and IBP as a function of IBP, age, gender, weight, and patient position (prone vs supine), using mixed effects linear regression with a patient-level random intercept. The patient-level random intercept was used to account for patient factors which were not explicitly included in the model, but that still varied between patients.16 Data analysis was performed using Stata/IC 14.2 (College Station, TX: StataCorp, LP), and p<0.05 was considered statistically significant. Individual deidentified participant data will not be shared by the investigators/authors.
Results
The study cohort included 30 patients, 18 boys and 12 girls, ranging in age from 0 to 8 years. Procedures included 28 (93%) cases of thoracic surgery, 1 (3%) neurological procedure, and 1 (3%) orthopedic procedure. Demographic characteristics and average measures of SBP, DBP, and MAP at each site are summarized for the study population in Tables 1 and 2. Ten BP measurements or approximately 50 mins were analyzed in each patient, for a total of 300 measurements or 15,000 mins of monitoring.
 |
Table 1 Demographic characteristics and blood pressure measurements of study population (N=30) |
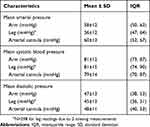 |
Table 2 Blood pressure measurements across all observations in study population (N=300) |
On a Bland-Altman plot (Figure 1), the bias and precision of NIBP (MAP) measured at the arm, relative to IBP, were −2 and 10 mmHg, respectively (95% limits of agreement: −21, +17 mmHg). The bias and precision of MAP measured at the leg, relative to IBP, were −5 and 11 mmHg, respectively (95% limits of agreement: −26, +16 mmHg). When comparing IBP to NIBP at the arm, the absolute difference in MAP was 7±7 mmHg (range: 0–52 mmHg) with 143 of 300 observations (48%) deviating by >5 mmHg and 60 of 300 observations (20%) deviating by >10 mmHg. When comparing IBP to NIBP at the leg, the absolute difference in MAP was 8±8 mmHg (range: 0–52 mmHg) with 169 of 298 observations (57%) deviating by >5 mmHg and 81 of 298 observations (27%) deviating by >10 mmHg.
 |
Figure 1 Bland-Altman plot of agreement between invasive mean arterial pressure (MAP) measurement and non-invasive MAP measurement. |
Comparisons of SBP and DBP between sites are summarized in Table 3. Although both NIBP sites demonstrated deviations from IBP, large deviations were more common when NIBP was obtained at the leg. A multivariable model predicting the magnitude of MAP deviation from IBP-values using arm and leg NIBP measurements is shown in Table 4. Gender, age, weight, and patient position were not associated with the magnitude of deviation from invasive MAP measurement. Leg, as compared to arm NIBP measurements, had a 1.5 mmHg greater absolute deviation in MAP from the IBP measurement (95% CI: 0.4, 2.6; p=0.009). Direct comparison of arm NIBP to leg NIBP (Figure 2) showed an absolute difference in MAP of 2.5±10 mmHg (95% limits of agreement: −17.1, +22.0 mmHg).
 |
Table 3 Comparison of mean arterial pressure, systolic blood pressure, and diastolic blood pressure in arm and leg to arterial cannula |
 |
Table 4 Mixed effects linear regression model predicting magnitude of deviation of mean arterial pressure from invasive measurement |
 |
Figure 2 Bland-Altman plot of agreement between arm and leg non-invasive mean arterial pressure (MAP) measurements. |
Discussion
Previous studies comparing NIBP to IBP measurements in anesthetized children are limited. While data in neonates are conflicting, several studies point toward a trend of overestimating BP when measured non-invasively. In a critically ill pediatric population, Joffe et al found the differences between NIBP and IBP measurements in 100 children were on average small, but the standard deviations, interquartile ranges, and limits of agreement on Bland-Altman plots were wide. These studies were not performed on patients under general anesthesia, a potentially beneficial feature of our study that could reduce error from patient movement or activity. Similar to the results of Joffe, however, our results suggest that although IBP and NIBP measurements in anesthetized children generally correlated with one another, individual NIBP measurements were often inaccurate with both over- and under-estimation of BP noted. Clinically significant discrepancies using NIBP occurred frequently during the study period. These deviations from IBP were greater and more frequent from the lower leg NIBP measurements as compared to those obtained from the upper arm.
Comparisons of pediatric arm versus leg NIBP measurements have been previously reported. In 2000, Short et al studied NIBP in 50 anesthetized children. In children age 8 years and under, BP obtained from the lower leg was significantly lower than that measured from the upper arm (p<0.05).17 In contrast to this, our study compared arm and leg NIBP to IBP measurements. Our results showed both over- and under-estimation of BP occurred more frequently in the leg, potentially indicating that lower leg NIBP is less reliable than upper arm NIBP.
Our study used thresholds of 5 and 10 mmHg to assess the degree of BP deviation, values which have precedent in the evaluation of the accuracy of automated BP measuring devices.18 While MAP differences of 5 or 10 mmHg may not have much clinical significance in an adult with an adequate perfusing BP, these deviations may be more significant in pediatric patients, especially those with borderline high or low BP, given their lower normal BP. An awake BP for a 2-year-old (our study population’s mean age) is 90–105/55–70. An infant 0–3 months old has a normal pressure of 65–85/45–55.19 A deviation of 10 mmHg in the latter patient’s MAP could lead to significant over- or under-perfusion, a problem that could result in end-organ damage and dysfunction. Additionally, these normal awake BP values will decrease further under general anesthesia.20
Despite the lack of a consistent trend in over- or under-measuring MAP by the two NIBP measurement sites, our findings extend the conclusions of previous studies comparing invasive and non-invasive BP measurements in children that noted discrepancies in NIBP and IBP are common. Importantly, our study eliminated error in NIBP measurements caused by patient movement or activity as our patients were under general anesthesia. Our results highlight the need for ongoing development of accurate, non-invasive monitors of blood pressure and hemodynamic function. The frequency of clinically significant variation also supports the importance of invasive monitoring when hemodynamic instability is anticipated or when moderate hypertension or hypotension would be particularly detrimental to a patient.
The findings of the current study may be limited by potential sources of error. We considered IBP as the gold standard against which we compared NIBP measurements. When invasive arterial BP is measured with a fluid-coupled transducer, inaccuracies with over- or under-measurement can occur based on the size of the intra-arterial catheter, air bubbles within the system, kinked or compressed tubing, or malpositioning of the arterial cannula.9 Errors in initial calibration or in positioning the transducer at the level of the patient’s right atrium are possible. NIBP measurements can be affected by incorrectly sized BP cuffs or external stimuli. While recommendations were made to follow the AHA cuff selection guidelines, cuff size selection was ultimately determined by the in-room anesthesiologist. This method created a cuff selection process consistent with our standard clinical practice. The resulting deviations in pressure represent clinically relevant deviations that would be expected to occur outside the context of this study. Additionally, there is no AHA recommendation for calf BP cuff size selection, so the AHA arm sizing guidelines were recommended to providers for the lower leg cuffs. It is unlikely the patients’ level of activity changed under general anesthesia, but external compression of the cuff by a surgeon, equipment, or operating room staff was possible.
Our study compared MAP measurements that were measured directly from oscillatory cuffs and derived from invasively obtained pressure pulse waves. Similarly, the derived SBP and DBP of oscillatory cuffs were compared to directly measured pulse pressure wave values. We did not control for potential confounding factors such as the use of vasopressors, and it is possible that vasoconstriction of the radial artery may have increased bias between IBP and NIBP. It is also important to note that BP varies in different parts of the body. A deviation detected between leg NIBP and arm BP (invasive or non-invasive) may represent a true difference in blood pressure in those locations. Additionally, many of our patients were undergoing thoracic surgeries, procedures which may affect arm BPs more than leg BPs. While we did not explicitly control for whether NIBP and IBP measurements were made in the same or different patient positions, we used mixed-effects regression to account for patient-level factors that were not explicitly included in our model. By doing this, the random effect absorbed these patient-level differences that were constant between observations from the same patient. While our inclusion criteria for study participants were children under 10, the majority of our patients were in fact much younger. As a consequence, our results may not be generalizable to older children. Our results are also limited to the monitoring devices used. Variations in BP values have been seen between different monitoring manufacturers. Oscillometric cuff manufacturers have different proprietary algorithms, and our results are only applicable to the devices used in our study.13,21–24
The possibility of such sources of error is noted by the fact that some of the values were more than 30–40 mmHg off from the IBP reading. As the data were recorded by research staff, it was not possible to determine the cause of such large variations and to determine if the readings were accurate. To maintain the integrity of the study, these values were recorded and included in the study cohort. Furthermore, we used 5 mins interval manual recording of BP data, but suspect that analysis of electronically collected continuous NIBP monitoring data may have revealed even more frequent inconsistencies between IBP and NIBP measurements.
Conclusion
Our data are novel in that they were obtained from patients under general anesthesia, but they are consistent with previous studies comparing the correlation of invasive and non-invasive BP readings. The frequency of clinically significant NIBP deviation supports the importance of IBP monitoring when hemodynamic fluctuations are likely or when these fluctuations would be particularly detrimental. Additionally, NIBP in a lower leg was more likely to result in clinically significant deviation from invasively measured MAP than NIBP values obtained from an upper arm. Given our study findings, the decision regarding site of cuff placement should not be arbitrary, but rather, we would suggest use of an arm when feasible during intraoperative BP monitoring.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Mogane P. Is blood pressure measurement important in children? S Afr Fam Pract. 2013;55(Suppl 1):S36–S39.
2. Walsh M, Devereaux PJ, Garg AX, et al. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: toward an empirical definition of hypotension. Anesthesiology. 2013;119:507–515.
3. Salmasi V, Maheshwari K, Yang D, et al. Relationship between intraoperative hypotension, defined by either reduction from baseline or absolute thresholds, and acute kidney and myocardial injury after noncardiac surgery. Anesthesiology. 2017;126:47–65.
4. Bijker JB, Persoon S, Peelen L, et al. Intraoperative hypotension and perioperative ischemic stroke after general surgery. Anesthesiology. 2012;116:658–664.
5. McCann ME, Schouten ANJ, Dobija N, et al. Infantile postoperative encephalopathy: perioperative factors as a cause for concern. Pediatrics. 2014;133:e751–757.
6. Alpert BS, Quinn D, Gallick D. Oscillometric blood pressure: a review for clinicians. J Am Soc Hypertens. 2014;12:930–938.
7. Barasch PG, Cullen BF, Stoelting RK, Cahalan MK, Stock MC, Ortega R. Clinical Anesthesia.
8. Meyer S, Sander J, Graber S, Gottschling S, Gortner L. Agreement of invasive versus non-invasive blood pressure in preterm neonates is not dependent on birth weight or gestational age. J Paediatr Child Health. 2010;46:249–254.
9. O’Shea J, Dempsey EM. A comparison of blood pressure measurements in newborns. Am J Perinatol. 2009;26:113–116.
10. Holt TR, Withington DE, Mitchell E. Which pressure to believe? A comparison of direct arterial with indirect blood pressure measurement techniques in the pediatric intensive care unit. Pediatr Crit Care Med. 2011;12:e391–e394.
11. Joffe R, Duff J, Guerra GG, Pugh J, Joffe AR. The accuracy of blood pressure measured by arterial line and non-invasive cuff in critically ill children. Crit Care. 2016;20:177.
12. Ray S, Rogers L, Noren DP, et al. Risk of over-diagnosis of hypotension in children: a comparative analysis of over 50,000 blood pressure measurements. Intensive Care Med. 2017;43(10):1540–1541.
13. Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: a statement for professionals from the subcommittee of professional and public education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111:697–716.
14. Clark JA, Lieh-Lai MW, Sarnaik A, Mattoo TK. Discrepancies between direct and indirect blood pressure measurements using various recommendations for arm cuff selection. Pediatrics. 2002;110:920–923.
15. Mantha S, Roizen MF, Fleischer LA, Thisted R, Foss J. Comparing methods of clinical measurement: reporting standards for Bland and Altman analysis. Anesth Analg. 2000;90:593–602.
16. Froysteter AB, Tumin D, Whitaker EE, et al. Changes in tissue and cerebral oxygenation following spinal anesthesia in infants: a prospective study. J Anes. 2018;32:288–292.
17. Short JA. Noninvasive blood pressure measurement in the upper and lower limbs of anaesthetized children. Paedetr Anaesthesia. 2000;10:591–593.
18. O’Brien E, Petrie J, Littler W, et al. The British Hypertension Society protocol for the evaluation of automated and semi-automated blood pressure measuring devices with special reference to ambulatory systems. J Hypertens. 1990;8:607–619.
19. Cote C, Lerman J, Anderson B. A Practice of Anesthesia for Infants and Children.
20. de Graaf JC, Pasma W, van Buuren S, et al. Reference values for noninvasive blood pressure in children during anesthesia: a multicentered retrospective observational cohort study. Anesthesiology. 2016;125(5):904–913.
21. Dannevig I, Dale HC, Liestøl K, Lindemann R. Blood pressure in the neonate: three non-invasive oscillometric pressure monitors compared with invasively measured blood pressure. Acta Pediatr. 2005;94:191–196.
22. Papadopoulos G, Mieke S, Elisaf M. Assessment of the performances of three oscillometric blood pressure monitors for neonates using a simulator. Blood Press Monit. 1999;4:27–33.
23. Diprose GK, Evans DH, Archer LN, Levene MI. Dinamap fails to detect hypotension in very low birthweight infants. Arch Dis Child. 1986;61:771–773.
24. Philips Medical Systems. 510(k) Premarket Notifications for Intellivue Information Center Software. Silver Springs, MD: U.S. Department of Health and Human Services Food and Drug Administration; 2019. Available from: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMN/pmn.cfm?start_search=1&Center=&Panel=&ProductCode=DSI&KNumber=&Applicant=PHILIPS%20MEDICAL%20SYSTEMS&DeviceName=&Type=&ThirdPartyReviewed=&ClinicalTrials=&Decision=&DecisionDateFrom=&DecisionDateTo=07%2F24%2F2019&IVDProducts=&Redact510K=&CombinationProducts=&ZNumber=&PAGENUM=10&SortColumn=dd%5Fdesc. Accessed August 14, 2019.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
