Back to Journals » Clinical Ophthalmology » Volume 9
Comparing resident cataract surgery outcomes under novice versus experienced attending supervision
Authors Puri S, Kiely A, Wang J, Woodfield A, Ramanathan S, Sikder S
Received 31 March 2015
Accepted for publication 21 May 2015
Published 15 September 2015 Volume 2015:9 Pages 1675—1681
DOI https://doi.org/10.2147/OPTH.S85769
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Sidharth Puri,1 Amanda E Kiely,2 Jiangxia Wang,3 Alonzo S Woodfield,4 Saras Ramanathan,5 Shameema Sikder2
1Johns Hopkins School of Medicine, Baltimore, MD, 2Wilmer Eye Institute, Johns Hopkins University School of Medicine, Baltimore, MD, 3Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, 4Kaiser Permanente South Sacramento Medical Center, Sacramento, 5San Francisco School of Medicine, University of California, San Francisco, CA, USA
Purpose: To determine whether supervision by an attending new to surgical teaching or an experienced attending measurably influences intraoperative complications rates or outcomes in phacoemulsification performed by ophthalmology residents.
Setting: Single tertiary hospital.
Design: Retrospective cohort study.
Methods: Resident-performed phacoemulsification cases supervised by one novice attending (N=189) and experienced attending (N=172) over 1 year were included. Data included: resident year, patient age, sex, preoperative risk factors (4+ dense/white/brunescent cataracts, Flomax, zonular dialysis, pseudoexfoliation, glaucoma risk, post-vitrectomy), intraoperative risk factors (Trypan blue, iris hooks), and intraoperative complications (capsule tears, vitreous loss, zonular dialysis, zonular dehiscence, burns, nuclear fragment loss, Descemet’s tear). Experienced attending data were compared against those of the novice attending.
Results: Regarding preoperative risks, experienced attending cases more likely involved 4+ cataract (P=0.005), Flomax (P<0.001), or glaucoma risk (P=0.001). For intraoperative risks, novice attending cases more likely involved Trypan blue (P<0.001). Regarding complications, novice attending cases were associated with vitreous loss (P=0.002) and anterior capsule tears (P<0.001). When comparing total complications, the novice attending was more likely to have both increased number of cases with complications and total complications than the experienced attending. The novice attending’s overall complication rate trended downward (rate from 28% in first 25 cases to 6.67% in last 15).
Conclusion: Early cases for the novice attending were accompanied by greater complications (vitreous loss and anterior capsule tear), likely due to a learning curve. Surgical judgment in the operating room likely develops with experience. Training programs may focus on these specific areas to aid new instructors.
Keywords: cataract surgery, attending experience, complication rate
Introduction
Cataract surgery is one of the most commonly performed surgeries worldwide.1–5 Ophthalmology residency programs require residents to complete extensive training in cataract extraction, specifically using phacoemulsification.2,3,6,7 Resident-performed phacoemulsification has been shown in the literature to have favorable outcomes, with roughly 74%–98% of patients with post-operative best corrected visual acuity ≥20/40.3 Further, intraoperative complication rates in resident-performed surgeries may vary from 2% to 14.7%.3
While outcomes have been favorable, many studies have sought to measure variables affecting resident-performed phacoemulsification, such as resident surgical experience, intraoperative complications, and surgical risks.1–9 Woodfield et al demonstrated that residency year did not significantly influence intraoperative complication rates, even when controlling for case difficulty.1 Intraoperative complications may include cases of vitreous loss, retinal detachment, vitreous hemorrhage, and posterior capsular rupture.4 Investigation into these complication rates have determined that there are surgical learning curves for trainees.
Several studies have delved into surgical learning curves for ophthalmological training.2,8–14 Investigation into surgical learning curves revealed that rates of capsular tears, vitreous loss, and phacoemulsification time decreased after the first 80 cases.2 Moreover, learning curves may project past the first 200 cases. As a result, programs can track and measure the progress of residents to ensure efficient patient care and surgical performance.
While many studies have observed the complex relationships between trainee experience and complications, there is limited understanding of how attending experience may impact resident surgical success.8 Surgical attendings supervise resident performance in the operating room and aim to prevent inappropriate and potentially dangerous surgical events.8,14 Attendings may also take over the surgery in cases of emergencies.8 As a result, attending experience and expertise should be salient for handling emergencies that may arise in the operating room. However, few studies actually exist to address this issue of experience. One comparable study by Martin and Burton demonstrated that a single well-trained attending relatively novice to phacoemulsification was still on a learning curve.14 It was observed in this study that there was a drop in capsular rupture/vitreous loss after 600 cases (4.3% to 2.3%, 3.7% to 0.7%, respectively) and a second drop in rate of capsular rupture after 1,200 cases (2.0% to 0.3%, ≤1.3% thereafter).
The question arises then: are novice attendings truly on a learning curve and in what particular areas do they require additional training to best teach residents? It is of critical importance for residency training programs to determine how best to train and prepare new attendings for supervising surgeries to reduce potential patient complications. The goal of this study is to determine the impact of a novice attending upon second and third year residents’ intraoperative complication rates and surgical outcomes. We will compare the complication rates over 1 year for residents under the tutelage of a novice attending (having recently completed a cornea fellowship) versus an experienced attending (11 years’ experience).
Materials and methods
Case selection
The research protocol and informed consent were approved by the Johns Hopkins Hospital Institutional Review Board. The study is a retrospective cohort study observing all phacoemulsification cataract surgeries supervised by a single novice attending at Johns Hopkins Hospital in 1 year (July 2011–July 2012) and by an experienced attending at Johns Hopkins Hospital in 1 year (July 2007–July 2008). Primary surgeons were second and third year residents. The curricula were the same for both resident groups and was solely dependent upon independent preparation by each resident with a clear delineation of resources available, such as independent reading, wet lab access, faculty access for wet lab supervision. All surgeries were determined from electronic medical records. No cases were excluded.
Regarding cases supervised by the novice surgeon, 189 patients were included in this study. The mean age of these patients was 63.5 years old. Forty-five percent (85/189) patients were male and 55% (104/189) were female (Table 1). Fifty-one percent (96/189) of surgeries were for the left eye and 49% (93/189) were for the right eye. Nine residents conducted the surgeries: seven third year residents and two second year residents.
  | Table 1 Demographic breakdown for patient population (N=189) for novice attending |
For cases supervised by the experienced surgeon, 172 patients were included in the study. Cases were conducted by only second and third year residents. Ten residents conducted surgeries: seven third year residents and three second year residents. Due to limitations of collected data, demographic data (sex, age, eye) for the patients were not able to be obtained.
Data
Clinical data were collected for each surgery, including: type of surgery, patient age, sex, preoperative risk factors, intraoperative risk factors, intraoperative complications, and any adverse short-term outcomes. Preoperative risk factors were designated as: 4+ on the four point scale for dense/white/brunescent cataract, Flomax, zonular dialysis, pseudoexfoliation, glaucoma risk, and post-vitrectomy. Intraoperative risk indicators were designated as: Trypan blue and iris hooks. Intraoperative complications were designated as: anterior capsule (AC) tear, posterior capsule tear, vitreous loss, zonular dialysis, zonular dehiscence, burns, nuclear fragment loss, Descemet’s tear. Adverse short-term outcomes were designated as: additional surgery, decreased vision from baseline in first 90 days. Adverse outcome data were not available for the experienced attending.
Preoperative risk factors, intraoperative risk factors, and intraoperative complications were compared between the cases supervised by the novice attending and experienced attending. Experienced attending-supervised cases were used as a control to compare against complication rates for cases supervised by the novice attending.
Complication rates were then compared against adverse short-term outcomes only for cases supervised by the novice attending. Total number of complications were then compared between the novice and experienced attending-supervised cases. Total number of complications is defined in this study as all the tabulated complications noted during the observed cases. Additional analysis was conducted to compare the sheer presence (yes/no) of a case with a complication for the novice- and experienced-supervised cases. To clarify, sheer presence (yes/no) of a case with a complication is distinct from individually tabulating total numbers of complications within observed cases.
Statistical analysis
Fisher’s exact tests were conducted with preoperative risk factors, intraoperative risk factors, and intraoperative complications to show whether there was a difference between the novice and experienced attending-supervised cases. Due to the disparity in the number of cases for the novice and experienced attendings (189 versus 172 cases), the cases were compared in groups of 25 in chronological order over 1 year. However, with the difference in total case number, the final grouping of cases should be noted to be 15, not 25 cases.
Results
Preoperative and intraoperative risk factors were reported in Table 2 for novice and experienced attending cases. The table shows the frequency and proportion of risk factors and complications in each group. Regarding preoperative risk factors, it was found that there were significantly more experienced attending cases involving 4+ cataract, Flomax, or glaucoma risk (P=0.005, P<0.001, P=0.001, respectively) than novice attending cases. Regarding intraoperative risk factors, it was found that there were significantly more novice attending cases involving Trypan blue (P<0.001) than experienced attending cases.
Intraoperative complications were recorded for novice and experienced attending-supervised cases in Table 3. Novice attending-supervised cases were significantly more likely to be associated with vitreous loss and AC tears (P=0.002 and P<0.001, respectively) than experienced attending cases.
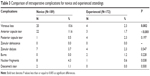  | Table 3 Comparison of intraoperative complications for novice and experienced attendings |
Intraoperative complication rates were trended against adverse outcome rates in Figure 1 for the novice attending cases. Complication rates were trended from 28% in the first 25 cases to 6.67% in last 15 cases. Adverse outcomes were trended from 8% in the first 25 cases to 0% in last 15 cases.
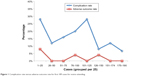  | Figure 1 Complication rate versus adverse outcome rate for first 189 cases for novice attending. |
Total number of intraoperative complications was trended for both novice and experience attendings in Figure 2. Total number of complications for the novice attending shifted from 16 in the first 25 cases to one in the last 15. Total number of complications for the experienced attending began with one in the first 25 cases and shifted to four in the last 23 cases.
  | Figure 2 Comparison of total complication rate for experienced versus novice attending. |
Sheer presence of a case with a complication was evaluated in Figure 3 for both the novice and experienced attendings. For the novice attending, presence of complications trended from seven in the first 25 cases to one in the last 15 cases. For the experienced attending, presence of complications trended from one in the first 25 cases to two in the last 23 cases.
  | Figure 3 Comparison of presence of complication for experienced versus novice attending. |
Discussion
Our data presented in this study suggest that attending experience may impact complication rates and outcomes for attending-supervised surgeries. Surgical attendings are expected to preside over resident cases and provide guidance to prevent operative complications. The role of the instructor can never be underestimated, in that he/she can impact a resident’s entire approach to surgery. The quality and strength of this guidance, however, may be reflected in surgical complications.
In our study, it was suggested that early cases in the year of supervision for a novice attending were accompanied by greater presence of complications and adverse outcomes. In Figure 2, the first 25 cases supervised by a novice attending had 16 complications while those supervised by the experienced attending only had one complication in the first 25 cases. Similarly, the findings in Figure 1 demonstrate a complication rate of 28% in the first 25 cases supervised by a novice attending. These elevated levels of complications early on in the year for the novice attending suggest that the instructor may have difficulty in his/her new role of supervision. Adapting and coaching residents may truly be a skill that comes with experience, as our data indicate with the overall lower number of complications in the cases supervised by the experienced attending.
Despite the initial spike in complications, our study demonstrates an overall decline in complications over 1 year for the novice attending-supervised cases. Figure 1 reveals an initial complication rate of 28% in the first 25 cases that falls to 6.67% in the last 15 cases. In tandem, the adverse outcomes trend from 8% in the first 25 cases to 0% in the last 15 cases. Even the sheer presence of a case with a complication in Figure 3 drops significantly for the novice attending over the year, from seven cases in the first 25 cases to one case in the last 15 cases. This improvement over the year suggests that there may be a learning curve for novice attendings. Instructors themselves require training on how best to guide their students and prevent errors. In the operating room, the attending with greater experience may prove more adept at predicting surgical mishaps and appropriately guiding residents.
Recognizing the importance of the novice attending’s learning curve is salient in ensuring patient safety and reducing surgical risk. Our study helped to suggest that cases supervised by novice attendings have increased risk for specific complications, such as vitreous loss rates and AC tears (P=0.002 and P<0.001, respectively). Similarly, the single-surgeon study by Martin and Burton found that capsule rupture and vitreous loss were significant problems for the surgeon relatively novice to phacoemulsification.14 It should be noted that there was improvement after the first 600 cases.14 By identifying areas of weakness, our study suggests that novice attendings may require additional training to better identify improper resident technique that increases the chance of capsule tears or vitreous loss. Ophthalmology programs should be encouraged to emphasize conservative surgical approach for novice attendings to improve these specific areas of concern.
Continuing simulation programs and development of surgical judgment will aid new surgeons who are transitioning to the role of attending. There is a definite need for faculty development and creating efficient educators in the field of ophthalmology. The relationship between the attending and resident is truly one that impacts the resident’s education.15 Through close interaction, the attending can pass on clear technical skills and emphasize the importance of patient-centered care. Educational institutions must begin to refocus upon how best to train their own teachers. As in any other setting, be it college or medical school, the educator is the gateway to knowledge for the student. In the setting of ophthalmology, mentorship amongst attendings can aid novice attendings in fine-tuning their skills out of fellowship. Additionally, ophthalmology programs can incorporate peer observation and feedback into their curricula for attendings as well. Proficiency in phacoemulsification is a continuously evolving skill. All educators have something to learn and experienced attendings should be incorporated into peer-training exercises early on in the academic year to aid novice attendings. Even by overseeing a surgery, an experienced attending may have the opportunity early on to teach a novice attending how best to provide surgical suggestions to a resident and anticipate poor outcomes given particular surgical risk factors.
Further, our study noted particular trends for preoperative and intraoperative risk factors. The greater presence of 4+ cataract, Flomax, and glaucoma risk in experienced attending cases may be due to uncontrollable factors such as case distribution and institutional factors. Also, we observed an increased use of Trypan blue by the novice attending. The significantly increased use of Trypan blue by the novice surgeon was likely due to a desire to facilitate the surgery and not necessarily correlated to the level of cataract. Though Trypan blue has the potential to serve as a surrogate marker for case complexity, the novice attending may have employed the use of Trypan blue to ensure safe measures when overseeing residents creating the rhexis. Knowledge of such variations in surgical practice can help clarify areas for improvement for training surgical leaders.
While this is one of the first studies to explore and demonstrate significant differences between novice and experienced attendings, there were several limitations. First, we only observed one novice and experienced attending. By having only two attendings in this study, our conclusions may not be fully applicable to the generalized attending population. Further, these attendings supervised different groups of residents during different years. As a result, collected data were unable to account for the confounding factors of case difficulty, prior resident experience from other rotations, or effects of anesthesia. Patient volume and case distribution may have varied as a result of the different years and uncontrollable institutional changes. Improvement in resident skill also may confound the findings of this study. Residents were the primary surgeons on the cases and residents’ progress at different rates based upon rotation schedule and case volume. The demographics for patient populations for the experienced attending were also unavailable.
Additionally, there is no consensus in the literature on standards for assessing complications. “Overall complications” are difficult to define. Rutar et al presented an attempt at complication classification: “major” (vitreous loss, wound burn, suprachoroidal hemorrhage, vitreous hemorrhage/retinal detachment/endophthalmitis within 90 days, requirement for reoperation) and “minor” (capsulorhexis failure, iris prolapse, iridodialysis, capsular or zonular tear without vitreous loss, intraocular lens problems.3
Even with these limitations, however, it is important to look toward the future. An ideal future study would contain multiple novice and experienced attendings working with a single set of residents. Also, it would be useful to determine in future studies if there were trends amongst specific complications (vitreous loss and capsule tears) over a year for the novice attending. However, this is the first study to address the issue of attending experience as a significant factor impacting resident education and patient outcome.
Overall, our data suggest that cases supervised by a surgeon placed in a new role of supervision may experience greater complications and specific types of complications (vitreous loss and capsule tears). Learning curves may exist for novice attendings. Surgical training programs should aim to reinforce these areas of potential weakness to create top surgical educators. From peer-based learning to hands-on feedback sessions, experienced attendings should be incorporated as surgical and educational mentors for novice attendings. By exploring this unique question of how attending experience may influence resident training, we can better prepare new attendings for the fulfilling role as the educator in the operating room.
Acknowledgments
This manuscript was presented as a short talk at the 12th Annual Educating the Educators Meeting at the Association of University Professors of Ophthalmology Meeting on January 28, 2015 in Tucson, AZ, USA. Funding was provided by Stephen J Ryan Faculty Scholar.
Author contributions
Design (SP, AEK, SS) and conduct (SP, AEK, JW, SS, SR) of the study; collection (SP, AEK, ASW, SR), management (SP, AEK), analysis (SP, AEK, JW, SS), and interpretation (SP AEK, SS, SR) of the data; and preparation (SP, AEK, SS) of the manuscript. All authors contributed toward drafting and critically revising the paper, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors have no conflicts of interest to disclose.
References
Woodfield AS, Gower EW, Cassard SD, Ramanathan S. Intraoperative phacoemulsification complication rates of second- and third-year ophthalmology residents a 5-year comparison. Ophthalmology. 2011;118(5):954–958. | ||
Randleman JB, Wolfe JD, Woodward M, et al. The resident surgeon phacoemulsification learning curve. Arch Ophthalmol. 2007;125(9):1215–1219. | ||
Rutar T, Porco TC, Naseri A. Risk factors for intraoperative complications in resident-performed phacoemulsification surgery. Ophthalmology. 2009;116(3):431–436. | ||
Bhagat N, Nissirios N, Potdevin L, et al. Complications in resident-performed phacoemulsification cataract surgery at New Jersey Medical School. Br J Ophthalmol. 2007;91(10):1315–1317. | ||
Briszi A, Prahs P, Hillenkamp J, Helbig H, Herrmann W. Complication rate and risk factors for intraoperative complications in resident-performed phacoemulsification surgery. Graefes Arch Clin Exp Ophthalmol. 2012;250(9):1315–1320. | ||
Quillen DA, Phipps SJ. Visual outcomes and incidence of vitreous loss for residents performing phacoemulsification without prior planned extracapsular cataract extraction experience. Am J Ophthalmol. 2003;135(5):732–733. | ||
Prakash G, Jhanji V, Sharma N, et al. Assessment of perceived difficulties by residents in performing routine steps in phacoemulsification surgery and in managing complications. Can J Ophthalmol. 2009;44(3):284–287. | ||
Lee JS, Hou CH, Yang ML, Lip KZ, Lin K. A different approach to assess resident phacoemulsification learning curve: analysis of both completion and complication rates. Eye (Lond). 2009;23(3):683–687. | ||
Blomquist PH, Rugwani RM. Visual outcomes after vitreous loss during cataract surgery performed by residents. J Cataract Refract Surg. 2002;28(5):847–852. | ||
Tayanithi P, Pungpapong K, Siramput P. Vitreous loss during phacoemulsification learning curve performed by third-year residents. J Med Assoc Thai. 2005;88 Suppl 9:S89–S93. | ||
Allinson RW, Metrikin DC, Fante RG. Incidence of vitreous loss among third-year residents performing phacoemulsification. Ophthalmology. 1992;99(5):726–730. | ||
Tarbet KJ, Mamalis N, Theurer J, Jones BD, Olson RJ. Complications and results of phacoemulsification performed by residents. J Cataract Refract Surg. 1995;21(6):661–665. | ||
Corey RP, Olson RJ. Surgical outcomes of cataract extractions performed by residents using phacoemulsification. J Cataract Refract Surg. 1998;24(1):66–72. | ||
Martin KR, Burton RL. The Phacoemulsification Learning Curve: Per-operative complications in the first 3000 cases of an experienced surgeon. Eye (Lond). 2000;14(Pt 2):190–195. | ||
Butler KL. Patient-centered instruction: the cornerstone of surgical education. Acad Med. 2015;90(4):398. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

